Diclofenac (Systemic, Local) (Monograph)
Brand names: Cambia, Flector, Licart, Voltaren, Zipsor
Drug class: Reversible COX-1/COX-2 Inhibitors
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke). Risk may occur early in treatment and may increase with higher dosages.
-
Contraindicated in the setting of CABG surgery.
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine). Serious GI events can occur at any time and may not be preceded by warning signs and symptoms. Geriatric individuals and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.
Introduction
NSAIA; also exhibits analgesic and antipyretic activity.
Uses for Diclofenac (Systemic, Local)
Inflammatory Diseases
Orally for symptomatic treatment of osteoarthritis (diclofenac sodium delayed-release tablets and extended-release tablets; diclofenac potassium tablets).
Topically (as 1.5 or 2% solution) for the symptomatic treatment of osteoarthritis of the knee.
Topically (as 1% gel) for self-medication for temporary relief of arthritis pain in the hand, wrist, elbow, foot, ankle, or knee.
American College of Rheumatology (ACR) recommends topical/oral NSAIAs for treatment of osteoarthritis, among other interventions. Therapy selection is patient-specific; factors to consider include patients' values and preferences, risk factors for serious adverse GI effects, existing comorbidities (e.g., hypertension, heart failure, other cardiovascular disease, chronic kidney disease), injuries, disease severity, surgical history, and access to and availability of the interventions.
Orally for symptomatic treatment of rheumatoid arthritis (diclofenac sodium delayed-release tablets and extended-release tablets; diclofenac potassium tablets).
Guidelines on the treatment of rheumatoid arthritis from ACR recommend initiation of a disease-modifying antirheumatic drug (DMARD) for most patients; role of NSAIAs not discussed.
Orally for symptomatic treatment of ankylosing spondylitis (diclofenac sodium delayed-release tablets).
Continuous NSAIA treatment is considered first-line for active ankylosing spondylitis in current guidelines. On-demand NSAIAs are recommended for stable ankylosing spondylitis. No preference is given to one NSAIA over another.
Diclofenac sodium also commercially available in an oral fixed-combination preparation with misoprostol for symptomatic treatment of rheumatoid arthritis and osteoarthritis in adults at high risk of developing NSAIA-induced gastric and duodenal ulcers and their complications. See full prescribing information for use of this combination product.
Orally for management of juvenile rheumatoid arthritis† [off-label].
Orally for symptomatic relief of gout† [off-label] and acute painful shoulder† [off-label] .
Pain
Orally for relief of mild to moderate pain (diclofenac potassium tablets and capsules).
Transdermally for relief of acute pain due to minor strains, sprains, and contusions (diclofenac epolamine transdermal systems).
American College of Physicians recommends topical NSAIAs (with or without menthol gel) as first-line therapy to reduce or relieve symptoms (including pain) and improve physical function in patients with non-low back pain musculoskeletal injury. Oral NSAIAs and acetaminophen also suggested to reduce pain and (for NSAIAs) improve physical function.
Current guidelines on postoperative pain management recommend a multimodal approach to analgesia. NSAIAs recommended as part of multimodal analgesia in patients without contraindications. When selecting therapy for a specific patient, consider potential risks associated with NSAIAs.
Diclofenac sodium also has been used for symptomatic relief of oral surgery pain† [off-label] and low back pain† [off-label] .
Migraine
Orally (as diclofenac potassium solution) for acute treatment of migraine attacks with or without aura; should not be used for prophylaxis of migraine.
Safety and efficacy not established for treatment of cluster headache (an older, predominantly male population).
Agents with established efficacy in adults with acute migraine include triptans, ergotamine derivatives, gepants, lasmiditan, NSAIAs (aspirin, celecoxib oral solution, diclofenac, ibuprofen, naproxen), and the combination of acetaminophen, aspirin, and caffeine. Nonspecific analgesic therapies such as NSAIAs and acetaminophen/aspirin/caffeine are used for mild-to-moderate attacks, while migraine-specific therapies (e.g., triptans, ergotamine derivatives, gepants, lasmiditan) are used for moderate-to-severe attacks or mild-to-moderate attacks that respond poorly to non-specific therapy. Selection of an agent for acute treatment should be based on patient-specific factors such as comorbid disease states, individual treatment history, and concomitant medications.
Dysmenorrhea
Orally for symptomatic management of primary dysmenorrhea (diclofenac potassium tablets).
Diclofenac sodium also has been used for symptomatic management of primary dysmenorrhea.
First-line treatment options for primary dysmenorrhea include combined oral contraceptives, progesterone-only contraceptives, and NSAIAs; treatment selection should be based on patient-specific considerations (e.g., comorbidities, desire/need for contraception). The American College of Obstetricians and Gynecologists does not address specific role for diclofenac in primary dysmenorrhea.
Other Uses
Diclofenac sodium ophthalmic solution used for treatment of postoperative ocular inflammation in patients undergoing cataract extraction and for temporary relief of pain and photophobia in patients undergoing corneal refractive surgery.
Diclofenac (Systemic, Local) Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in women of reproductive potential before initiating diclofenac sodium in fixed combination with misoprostol (Arthrotec).
-
Measure serum aminotransferase concentrations at baseline.
-
Correct dehydration and hypovolemia before initiating therapy.
Patient Monitoring
-
Monitor blood pressure closely when initiating diclofenac and throughout therapy.
-
Obtain serum aminotransferase values 4–8 weeks after therapy with the drug is initiated and monitor periodically during long-term therapy.
-
Concomitant use of nonsteroidal anti-inflammatory agents (NSAIAs), such as diclofenac, with angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, or β-adrenergic blocking agents may reduce the blood pressure response to the antihypertensive agent; therefore, monitoring of blood pressure is recommended with concomitant use of these drugs.
-
Perform a CBC and chemistry profile periodically in patients receiving long-term NSAIA therapy.
-
Monitor renal function during therapy in patients with preexisting renal or hepatic impairment, heart failure, dehydration, or hypovolemia.
-
Monitor patients receiving NSAIAs (including those without previous symptoms of cardiovascular disease) for the possible development of cardiovascular events throughout therapy.
-
Monitor patients receiving concomitant low-dose aspirin therapy for cardiac prophylaxis closely for evidence of GI bleeding.
Dispensing and Administration Precautions
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes diclofenac on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings. The criteria are intended to apply to adults 65 years of age and older in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings. For non-COX-2-selective oral NSAIAs such as diclofenac, the Beers Criteria Expert Panel specifically recommends that chronic use be avoided unless other alternatives are not effective and the patient can take a gastroprotective agent (proton-pump inhibitor or misoprostol). Additionally, short-term scheduled use should be avoided in combination with oral or parenteral corticosteroids, anticoagulants, or antiplatelet agents unless other alternatives are not effective and the patient can take a gastroprotective agent.
Other General Considerations
-
Because patients may have aspirin-sensitive asthma, patients with asthma but without known aspirin sensitivity who are receiving diclofenac should be monitored for changes in manifestations of asthma.
-
To minimize the potential risk of adverse GI effects, the lowest effective dosage and shortest possible duration of therapy should be employed, and use of more than one NSAIA at a time should be avoided.
-
Use of NSAIAs should be avoided in patients at higher risk of bleeding unless the benefits of therapy are expected to outweigh the increased risk of bleeding. Higher risk patients include those with a history of ulcer disease or other factors that may increase the risk for GI bleeding, including concomitant use of oral corticosteroids, anticoagulants, aspirin, or selective-serotonin reuptake inhibitors (SSRIs); longer duration of NSAIA therapy; smoking; alcohol use; older age; poor general health status; advanced liver disease; and/or coagulopathy.
-
Diclofenac should be avoided in patients with recent myocardial infarction unless the benefits of therapy are expected to outweigh the risk of recurrent cardiovascular thrombotic events; if diclofenac is used in such patients, they should be monitored for cardiac ischemia.
Administration
Oral Administration
Oral Solution
Empty the contents of one packet containing 50 mg of buffered diclofenac potassium powder for oral solution into a cup containing 30–60 mL of water, mix well, and administer immediately. Do not use liquids other than water.
Administration with food may decrease peak plasma concentrations and reduce efficacy compared with administration on an empty stomach.
Topical Administration
Diclofenac Sodium 1.5 or 2% Topical Solution
Topical 1.5% solution: Administer as drops dispensed directly onto affected knee(s); alternatively, administer into palm of hand and apply to affected knee(s). To avoid spillage, apply drops in 4 increments of 10 drops each per joint; following each incremental application, spread solution evenly around the front, back, and sides of the knee.
Topical 2% solution: Administer via pump dispenser (2 pump actuations per affected joint) into palm of hand; then evenly apply the entire volume of solution around the front, back, and sides of the knee. Pump must be primed before first use by fully depressing the pump mechanism 4 times while holding the bottle in an upright position.
Wait until treated area is dry before covering with clothing; wait ≥30 minutes before bathing or showering.
Wash hands after application.
Avoid skin-to-skin contact between other individuals and the treated area until the area is completely dry.
Do not apply to open wounds, infected or inflamed areas of skin, or areas affected with exfoliative dermatitis; avoid contact with eyes and mucous membranes.
Do not expose treated knee to external heat, and avoid exposing treated knee to natural or artificial sunlight; also avoid use of occlusive dressings.
Allow treated knee to dry completely before applying other topical preparations (e.g., sunscreen, insect repellant, lotions, moisturizers, cosmetics, other topical medications) to the same area.
Diclofenac Epolamine Transdermal System
Apply transdermal system to the most painful area once daily (Licart) or twice daily (Flector). Apply to intact skin; do not apply to damaged skin (e.g., wounds, burns, infected areas of skin, areas affected with eczema or exudative dermatitis).
Wash hands after handling the system.
Avoid contact with eyes and mucous membranes.
Do not wear the transdermal system while bathing or showering.
If a system should begin to peel off during the period of use, the edges of the system may be taped to the skin. If problems with adhesion persist, a nonocclusive mesh netting sleeve (e.g., Curad Hold Tite, Surgilast Tubular Elastic Dressing) may be used when appropriate (e.g., over ankles, knees, or elbows) to secure the system.
Ophthalmic Administration
Apply 0.1% ophthalmic solution topically as an eye drop.
Avoid use in patients with soft contact lenses (except for bandage hydrogel soft contact lenses during the first 3 days following refractive surgery).
Dosage
Available as diclofenac potassium, diclofenac sodium, or diclofenac epolamine.
Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals. Adjust dosage based on individual requirements and response.
Different strengths and formulations of oral diclofenac are not interchangeable. Commercially available diclofenac sodium delayed-release tablets, diclofenac sodium extended-release tablets, and diclofenac potassium immediate-release tablets are not necessarily bioequivalent on a mg-per-mg basis. In addition, the frequency of administration may vary across available products; diclofenac potassium liquid-filled capsules are administered 4 times daily, while diclofenac potassium conventional tablets are administered 2–4 times daily.
Each actuation of the pump dispenser of diclofenac sodium 2% topical solution delivers 20 mg of diclofenac sodium in 1 g of solution. The 1.5% topical solution contains diclofenac sodium 16.05 mg/mL.
Each mL of 0.1% diclofenac sodium ophthalmic solution delivers 1 mg of diclofenac sodium.
Pediatric Patients
Acute Pain
Oral
Pediatric patients ≥12 years of age: Diclofenac potassium liquid-filled capsules: 25 mg 4 times daily.
Topical (transdermal system)
Pediatric patients ≥6 years of age: Apply 1 transdermal system (diclofenac epolamine 1.3%) twice daily (Flector).
Adults
Cataract Surgery
Ophthalmic
Apply 1 drop of 0.1% solution 4 times daily starting 24 hours after cataract surgery; continue for 2 weeks postoperatively.
Corneal Refractive Surgery
Ophthalmic
Apply 1–2 drops of 0.1% solution to the operative eye 1 hour prior to surgery. Within 15 minutes after surgery, apply 1–2 drops to affected eye and continue 4 times daily for up to 3 days.
Inflammatory Diseases
Osteoarthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
100–150 mg daily, given as 50 mg 2 or 3 times daily |
|
Diclofenac sodium delayed-release tablets |
100–150 mg daily, given as 50 mg 2 or 3 times daily or 75 mg twice daily |
|
Diclofenac sodium extended-release tablets |
100 mg once daily |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 times daily |
Diclofenac sodium 1.5% topical solution: 40 drops (approximately 1.2 mL) applied to each affected knee 4 times daily.
Diclofenac sodium 2% topical solution: 40 mg (2 pump actuations) applied to each affected knee twice daily.
Rheumatoid Arthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
150–200 mg daily, given as 50 mg 3 or 4 times daily |
|
Diclofenac sodium delayed-release tablets |
150–200 mg daily, given as 50 mg 3 or 4 times daily or 75 mg twice daily |
|
Diclofenac sodium extended-release tablets |
100 mg once daily; may increase to 100 mg twice daily |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 or 4 times daily |
Ankylosing Spondylitis
Oral100–125 mg daily (as diclofenac sodium delayed-release tablets); administer as 25 mg 4 times daily, with 5th dose at bedtime as needed.
Pain
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets). Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).
25 mg 4 times daily (as diclofenac potassium liquid-filled capsules) for mild to moderate acute pain.
Topical (transdermal system)
Apply 1 transdermal system (diclofenac epolamine 1.3%) once daily (Licart) or twice daily (Flector).
Migraine
Oral
Single 50-mg dose (contents of one packet containing diclofenac potassium for oral solution mixed with water). Safety and efficacy of administering a second dose not established.
Dysmenorrhea
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets). Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).
Special Populations
Hepatic Impairment
Reduction of oral dosage may be necessary.
Manufacturer of diclofenac potassium liquid-filled capsules recommends initiating treatment at the lowest dosage; if efficacy is not achieved at that dosage, discontinue diclofenac and consider alternative therapy.
Monitoring of renal function recommended in patients with hepatic impairment.
Renal Impairment
Reduction of oral dosage does not appear to be necessary.
Avoid use of diclofenac in advanced renal disease unless benefits are expected to outweigh risks of therapy. If diclofenac administered, monitor patients for signs of worsening renal function.
Correct volume status in dehydrated or hypovolemic patients prior to initiating diclofenac. Monitoring of renal function recommended, especially with concomitant ACE inhibitors of angiotensin II receptor antagonists, or in patients with heart failure, dehydration, or hypovolemia.
Geriatric Patients
Increased risk of NSAIA-associated serious cardiovascular, gastrointestinal, and/or renal adverse effects compared to younger adults. Risk possibly increased in patients with renal impairment or those receiving concomitant ACE inhibitor or angiotensin II receptor antagonists. If potential benefits outweigh potential risks, initiate therapy at the lower end of the dosage range and monitor for adverse effects.
Avoid diclofenac in fixed combination with misoprostol in geriatric patients with cardiovascular and/or renal risk factors. If use cannot be avoided, use the lowest recommended dosage for the shortest possible duration with additional monitoring for cardiac and renal adverse effects. Monitor renal function in geriatric patients receiving diclofenac in fixed combination with misoprostol, particularly during concomitant therapy with an ACE inhibitor or angiotensin II receptor antagonist.
Cautions for Diclofenac (Systemic, Local)
Contraindications
-
Known hypersensitivity (e.g., anaphylaxis, serious dermatologic reactions) to diclofenac or any ingredient in the formulation.
-
History of asthma, urticaria, or other sensitivity reaction precipitated by aspirin or other NSAIAs.
-
In the setting of CABG surgery.
-
Diclofenac sodium in fixed combination with misoprostol: Active GI bleeding.
-
Diclofenac sodium in fixed combination with misoprostol: Pregnancy.
-
Diclofenac potassium liquid-filled capsules: Hypersensitivity to bovine protein.
-
Diclofenac epolamine transdermal system: Use on nonintact or damaged skin, regardless of etiology (e.g., exudative dermatitis, eczema, infected lesions, burns, wounds).
Warnings/Precautions
Warnings
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease (see Boxed Warning).
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI; absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.
Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia. Contraindicated in the setting of CABG surgery.
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events associated with NSAIAs.
GI Bleeding, Ulceration, and Perforation
Serious, sometimes fatal, GI toxicity (e.g., bleeding, ulceration, perforation of esophagus, stomach, or small or large intestine) can occur with or without warning symptoms (see Boxed Warning).
Risk for GI bleeding increased more than tenfold in patients with a history of peptic ulcer disease and/or GI bleeding who are receiving NSAIAs compared with patients without these risk factors.
Other risk factors for GI bleeding include concomitant use of oral corticosteroids, anticoagulants, aspirin, or SSRIs; longer duration of NSAIA therapy; smoking; alcohol use; older age; poor general health status; and advanced liver disease and/or coagulopathy.
Use at lowest effective dosage for the shortest duration necessary.
Avoid use of more than one NSAIA at a time.
Avoid use of NSAIAs in patients at higher risk for GI toxicity unless expected benefits outweigh increased risk of bleeding; consider alternate therapies in high-risk patients and those with active GI bleeding.
Monitor for GI ulceration and bleeding; even closer monitoring for GI bleeding recommended in those receiving concomitant low-dose aspirin for cardiac prophylaxis.
If serious adverse GI event suspected, promptly initiate evaluation and discontinue diclofenac until serious adverse GI event ruled out.
Other Warnings and Precautions
Heart Failure and Edema
Fluid retention and edema reported.
NSAIAs increase the risk of MI, hospitalization for heart failure, and death.
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema.
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.
Hepatotoxicity
Monitor for symptoms and/or signs suggesting liver dysfunction.
Measure serum aminotransferase concentrations at baseline and 4–8 weeks after initiating therapy; monitor periodically during long-term therapy.
Use at lowest effective dosage for the shortest duration necessary; use with caution in patients receiving other potentially hepatotoxic drugs (e.g., acetaminophen, certain antibiotics, anticonvulsant agents).
Discontinue immediately if abnormal liver function test results persist or worsen, if clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations (e.g., eosinophilia, rash) occur.
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events.
Monitor BP during initiation of diclofenac and throughout therapy.
Impaired response to ACE inhibitors and certain diuretics may occur.
Renal Toxicity and Hyperkalemia
Potential for overt renal decompensation. Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure, in geriatric patients, in patients with volume depletion, and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist.
Correct fluid depletion prior to initiating diclofenac; monitor renal function during therapy in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia.
Hyperkalemia reported with NSAIAs, even in some patients without renal impairment; in such patients, effects attributed to a hyporenin-hypoaldosterone state.
Anaphylactic Reactions
Anaphylactic reactions reported in patients with and without known hypersensitivity to diclofenac and in patients with aspirin-sensitive asthma.
Exacerbation of Asthma Related to Aspirin Sensitivity
Patients with asthma can have aspirin-sensitive asthma, which manifests principally as chronic rhinosinusitis with severe (possibly fatal) bronchospasm and usually nasal polyps.
Avoid in patients with cross-sensitivity to aspirin. In patients with asthma but without known aspirin sensitivity, monitor for changes in manifestations of asthma.
Serious Skin Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning. Fixed drug eruption (FDE), or more severe, potentially life-threatening generalized bullous fixed drug eruption (GBFDE) can occur.
Discontinue at first appearance of rash or any other sign of hypersensitivity (e.g., blisters, fever, pruritus).
Drug Reaction with Eosinophilia and Systemic Symptoms
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs. Clinical presentation variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis). Symptoms may resemble those of acute viral infection. Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in absence of rash. If signs or symptoms of DRESS develop, discontinue diclofenac and immediately evaluate the patient.
Fetal/Neonatal Morbidity and Mortality
NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus, and use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios, and in some cases, neonatal renal impairment.
Avoid NSAIAs in pregnant women at about ≥30 weeks of gestation; if NSAIA therapy necessary between about 20−30 weeks of gestation, use lowest effective dosage and for shortest possible duration.
Fixed combination of diclofenac and misoprostol: Contraindicated in pregnant women. Misoprostol exhibits abortifacient activity and can cause serious fetal harm. Use in women of reproductive potential only if they require NSAIA therapy and are considered at high risk of complications resulting from NSAIA-induced gastric or duodenal ulceration or at high risk of developing gastric or duodenal ulceration.
Verify pregnancy status in women of reproductive potential within 2 weeks of initiating diclofenac sodium in fixed combination with misoprostol.
Hematologic Toxicity
Anemia reported. May be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. Determine hemoglobin concentration or hematocrit if signs or symptoms of anemia or blood loss occur.
NSAIAs may increase the risk of bleeding. Patients with certain coexisting conditions (e.g., coagulation disorders) or receiving concomitant therapy with anticoagulants, antiplatelet agents, or serotonin-reuptake inhibitors may be at increased risk; monitor such patients for bleeding.
Masking of Inflammation and Fever
Antipyretic and anti-inflammatory effects of diclofenac may mask usual signs and symptoms of infection.
Laboratory Monitoring
Monitor CBC and chemistry profile periodically in patients receiving long-term therapy.
Precautions Specific to Transdermal or Other Topical Use
Avoid exposure of treated areas to natural or artificial sunlight. The potential effects of topical diclofenac gel or solution on skin response to UV damage in humans are not known.
Application to nonintact skin may alter absorption and tolerability; apply only to intact skin.
Avoid contact with the eyes and mucous membranes. If contact with the eyes occurs, thoroughly rinse the eyes with water or saline. If ocular irritation persists for >1 hour, consult a clinician.
Do not apply to nonintact or damaged skin.
Patient should bathe or shower after removing one transdermal system and before applying a new system; the transdermal system should not be worn during bathing or showering.
Store and discard transdermal systems in a manner that avoids accidental exposure or ingestion by children or pets.
Medication Overuse Headache
Excessive use of drugs indicated for the management of acute migraine attacks (e.g., use of NSAIAs, 5-HT1 receptor agonists, ergotamine, or opiates on a regular basis for ≥10 days per month) may result in migraine-like daily headaches or a marked increase in the frequency of migraine attacks. Detoxification, including withdrawal of the overused drugs and treatment of withdrawal symptoms (which often include transient worsening of headaches), may be necessary.
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice.
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs. Oligohydramnios is often, but not always, reversible following NSAIA discontinuance. Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation. In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios. Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis). Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of risk of adverse fetal and neonatal outcomes with maternal NSAIA use. Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants uncertain.
Effects of diclofenac on labor and delivery not known. In animal studies, NSAIAs, including diclofenac, increased incidence of dystocia, delayed parturition, and increased stillbirths.
Fixed combination of diclofenac and misoprostol: Contraindicated in pregnant women. Misoprostol exhibits abortifacient activity and can cause serious fetal harm.
Lactation
May be distributed into human milk; consider the developmental and health benefits of breast-feeding along with the mother's clinical need for diclofenac and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Females and Males of Reproductive Potential
NSAIAs may be associated with reversible infertility in some women. Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.
Pediatric Use
Safety and efficacy of diclofenac epolamine transdermal system (Flector) established in pediatric patients ≥6 years of age; safety comparable between pediatric patients and adults.
Safety and efficacy of diclofenac epolamine transdermal system (Flector) not established in pediatric patients <6 years of age.
Safety and efficacy of diclofenac potassium liquid-filled capsules established in pediatric patients 12−17 years of age; plasma concentrations of diclofenac similar to those observed in adult patients.
Safety and efficacy of other formulations of diclofenac not established in children.
Good results with oral diclofenac obtained in a limited number of children 3–16 years of age for the management of juvenile rheumatoid arthritis† .
Geriatric Use
Increased risk for serious adverse cardiovascular, GI, and renal effects. Risk of these adverse effects may be increased in geriatric patients with renal impairment or who are receiving concomitant ACE inhibitor or angiotensin II receptor antagonist therapy. Many of the spontaneous fatal adverse GI effects in patients receiving NSAIAs involve geriatric patients. If anticipated benefits outweigh potential risks, initiate at lower end of dosing range and monitor for adverse effects.
Diclofenac sodium 1.5% topical solution: No age-related differences in incidence of adverse effects observed.
Diclofenac epolamine transdermal system: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.
Diclofenac potassium oral solution: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.
Diclofenac sodium in fixed combination with misoprostol: Avoid in geriatric patients with cardiovascular and/or renal risk factors.
Use diclofenac with caution because of age-related decreases in renal function. May be useful to monitor renal function.
Hepatic Impairment
Almost completely metabolized in the liver; reduction of oral dosage may be necessary.
Diclofenac oral solution should only be used in patients with hepatic impairment if benefits outweigh risks.
Diclofenac epolamine transdermal system: Pharmacokinetics not evaluated in hepatic impairment.
Renal Impairment
No differences in diclofenac pharmacokinetics observed in patients with renal insufficiency. Avoid use in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function.
Diclofenac epolamine transdermal system: Pharmacokinetics not evaluated in renal impairment.
Common Adverse Effects
Diclofenac sodium delayed-release tablets, diclofenac potassium conventional tablets, or other NSAIAs (reported in 1–10% of patients): GI effects (abdominal pain, constipation, diarrhea, dyspepsia, flatulence, gross bleeding/perforation, heartburn, nausea, GI ulcers, and vomiting). Additionally, abnormal renal function, anemia, dizziness, edema, elevations in hepatic transaminases, headaches, increased bleeding time, pruritic, rashes, and tinnitus.
Diclofenac in fixed combination with misoprostol (reported in ≥2% of patients): Abdominal pain, diarrhea, dyspepsia, nausea, flatulence, gastritis, vomiting, constipation, headache, dizziness, increases in ALT, and decreases in hematocrit.
Diclofenac epolamine transdermal system (Flector): Pruritis (5%) and nausea (3%) reported. The most common adverse effects in pediatric patients were headache (9%) and application site pruritis (7%). Application site pruritis and application site reactions also common adverse effects in patients receiving diclofenac epolamine transdermal system (Licart).
Diclofenac potassium for oral solution (reported in ≥1% of patients): Nausea and dizziness.
Diclofenac sodium ophthalmic solution: Transient burning and stinging (15%), elevated intraocular pressure following cataract surgery (15%) and keratitis in up to 28% of patients, although keratitis was noted prior to treatment in many of these patients. Lacrimation complaints were also reported in approximately 30% of cases undergoing incisional refractive surgery. Other adverse effects reported in ≤10% of patients include abnormal vision, acute elevated intraocular pressure, blurred vision, conjunctivitis, corneal deposits, corneal edema, corneal opacity, corneal lesions, discharge, eyelid swelling, eye pain, injection (redness), iritis, irritation, itching, lacrimation disorder, and ocular allergy.
Drug Interactions
Metabolized by CYP isoenzymes, mainly CYP2C9. CYP3A4, uridine diphosphate-glucuronosyltransferase (UGT) 2B7, and CPY2C8 may contribute to metabolism.
Drugs Affecting Hepatic Microsomal Enzymes
CYP2C9 inhibitors: Possible increased systemic exposure to diclofenac and risk of adverse effects. Dosage adjustment may be required. Examples include, but are not limited to, voriconazole.
CYP2C9 inducers: Possible reduced efficacy of diclofenac. Dosage adjustment may be required. Examples include, but are not limited to, rifampin.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment |
Monitor BP Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function |
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonist Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment |
Monitor BP Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function |
|
Antacids |
Delayed diclofenac absorption |
|
|
Anticoagulants (warfarin) |
Possible bleeding complications |
Caution advised; carefully observe for signs of bleeding |
|
β-Adrenergic blocking agents |
Reduced BP response to β-blocker |
Monitor BP |
|
Cyclosporine |
Possible increase in nephrotoxic effects of cyclosporine |
Monitor for worsening renal function |
|
Digoxin |
Increased serum concentrations and prolonged half-life of digoxin |
Monitor serum digoxin concentrations |
|
Diuretics (furosemide, thiazides, potassium-sparing) |
Reduced natriuretic effects Concomitant use of potassium-sparing diuretics may be associated with increased serum potassium concentrations |
Monitor for worsening renal function and for adequacy of diuretic and antihypertensive effects |
|
Lithium |
Increased plasma lithium concentrations |
Monitor for lithium toxicity |
|
Methotrexate |
Possible increased risk of methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction) |
Monitor for methotrexate toxicity |
|
NSAIAs |
Concomitant NSAIAs and aspirin (analgesic dosages): Therapeutic effect not greater than that of NSAIAs alone Concomitant NSAIAs and aspirin: Increased risk for bleeding and serious adverse GI effects Concomitant use of oral and topical NSAIAs may result in higher incidence of hemorrhage and abnormal Scr, urea, and hemoglobin concentrations Protein binding of NSAIAs reduced by aspirin, but clearance of unbound NSAIA not altered; clinical importance unknown No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs |
Concomitant use of diclofenac with analgesic dosages of aspirin generally not recommended Do not use topical diclofenac formulations with oral NSAIAs unless expected benefits outweigh risks and periodic laboratory evaluations are performed Advise patients not to take low-dose aspirin without consulting clinician; closely monitor patients receiving concomitant antiplatelet agents (e.g., aspirin) for bleeding |
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid administration beginning 2 days before and continuing through 2 days after pemetrexed administration Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid administration beginning at least 5 days before and continuing through 2 days after pemetrexed administration Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity |
|
Serotonin-reuptake inhibitors (e.g., SSRIs, SNRIs) |
Possible increased risk of bleeding |
Monitor for bleeding |
|
Voriconazole |
Peak concentration and AUC of diclofenac increased by 114 and 78%, respectively |
Dosage adjustment may be required |
Diclofenac (Systemic, Local) Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration. Undergoes first-pass metabolism; only 50% of a dose reaches systemic circulation as unchanged drug.
Peak plasma concentration usually attained within about 0.47 hours (diclofenac potassium liquid-filled capsules), 1 hour (diclofenac potassium conventional tablets), 2.3 hours (diclofenac sodium delayed-release tablets), or 5.3 hours (diclofenac sodium extended-release tablets).
Absorbed into systemic circulation following topical administration as gel, solution, or transdermal system; plasma concentrations generally very low compared with oral administration.
Following application of a single diclofenac epolamine transdermal system (Flector) to intact skin on the upper arm, peak plasma concentrations occur in 10–20 hours; moderate exercise does not alter absorption. Plasma diclofenac concentrations similar in pediatric patients ≥6 years of age compared to adults.
Following application of diclofenac epolamine transdermal system (Licart) to anterior thigh, peak concentrations occur in 4–20 hours; moderate exercise, application of an occlusion dressing over the system, or moderate heat increases peak plasma concentrations and systemic exposure by approximately 20%.
Following topical application of diclofenac sodium 1.5% solution to knees, peak plasma concentrations occur in about 4 hours. Not established whether occlusive dressings, application of heat, or exercise affects absorption of diclofenac sodium 2% solution.
Food
Conventional, delayed-release, or extended-release tablets: Food delays time to reach peak plasma concentration but does not affect extent of absorption.
Diclofenac potassium oral solution: Administration after a high-fat meal reduces peak plasma concentrations by approximately 70% but does not substantially affect extent of absorption.
Diclofenac potassium liquid-filled capsules: Food decreases rate of absorption (47% decrease in peak concentration, twofold increase in time to peak concentration) but does not substantially affect extent of absorption.
Distribution
Extent
Distributes into human milk.
Plasma Protein Binding
>99%.
Elimination
Metabolism
Metabolized in the liver via hydroxylation and conjugation. Five metabolites detected in plasma and urine.
Formation of 4′-hydroxydiclofenac (principal metabolite) is mediated mainly by CYP2C9; formation of 5-hydroxydiclofenac and 3′-hydroxydiclofenac (minor metabolites) is mediated by CYP3A4. UGT2B7 and CYP2C8 may mediate acyl glucuronidation and oxidation reactions, respectively.
Elimination Route
Excreted in urine (65%) and in feces via biliary elimination (35%).
Half-life
Diclofenac sodium: 2.3 hours.
Diclofenac potassium: 1.9 hours.
Diclofenac epolamine transdermal system: Approximately 12 hours.
Special Populations
In patients with renal impairment, plasma clearance not substantially altered.
Stability
Storage
Oral
Capsules, Liquid-filled
Tight container at 20–25°C (may be exposed to 15–30°C). Protect from moisture.
Powder for Oral Solution
25°C (may be exposed to 15–30°C).
Tablets
Tight containers at room temperature (20–25°C); consult manufacturer's labeling for specific storage recommendation. Protect from moisture.
Diclofenac sodium in fixed combination with misoprostol: 25°C (may be exposed to 15–30°C).
Topical
Solution
Diclofenac sodium 0.1% ophthalmic solution: 20–25°C protected from light.
Diclofenac sodium 1.5% topical solution: 20–25°C (may be exposed to 15–30°C).
Diclofenac sodium 2% topical solution: 25°C (may be exposed to 15–30°C).
Transdermal System
20–25°C (may be exposed to 15–30°C). Licart systems stable for up to 6 months after envelope is opened if stored at room temperature in the resealed envelope.
Actions
-
NSAIA; inhibits cyclooxygenase-1 (COX-1) and COX-2.
-
Mode of action associated principally with reduction of prostaglandin synthesis in peripheral tissues; exhibits anti-inflammatory, analgesic, and antipyretic activity.
Advice to Patients
-
Advise patients to read the medication guide for nonsteroidal anti-inflammatory agents (NSAIAs) that is provided each time the drug is dispensed.
-
Inform patients of the risk of serious cardiovascular thrombotic events. Stress importance of reporting signs and symptoms of a cardiovascular event (e.g., chest pain, shortness of breath, weakness, slurred speech) immediately to a healthcare provider.
-
Inform patients to report symptoms of GI bleeding and ulceration (e.g., epigastric pain, dyspepsia, melena, hematemesis) to their healthcare provider. Notify patients receiving concomitant low-dose aspirin of the increased risk of GI bleeding.
-
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, anorexia, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms). If these occur, inform patients to stop diclofenac and seek immediate medical attention.
-
Inform patients of the risk of serious skin reactions, including drug reaction with eosinophilia and systemic symptoms (DRESS). Advise patients to stop taking diclofenac immediately if they develop any type of rash or fever and to promptly contact their clinician.
-
Stress importance of seeking immediate medical attention if an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat) occurs.
-
Inform patients of the risk of heart failure or edema, and to watch out for symptoms of heart failure such as shortness of breath, unexplained weight gain, or edema, and to contact their healthcare provider if these occur.
-
Warn patients to keep diclofenac transdermal system out of the reach of children and pets and to safely dispose of used units.
-
Stress importance of avoiding or limiting exposure of skin treated with diclofenac gel or solution to natural or artificial sunlight.
-
Advise patients receiving diclofenac topical solution to avoid applying to open wounds, infections, inflammation, or exfoliative dermatitis.
-
Advise patients receiving diclofenac topical solution to wait until the treated area is completely dry before applying sunscreen, insect repellent, lotion, moisturizer, cosmetics, or other topical medications.
-
Advise patients receiving diclofenac topical solution to promptly contact their clinician if any type of rash develops at the application site.
-
Advise patients receiving diclofenac topical solution that other individuals should avoid contact with the application site(s) until the site is completely dry.
-
Inform patients that if topical formulations of diclofenac come into contact with the eye(s), to rinse the affected eye(s) with water or saline and consult a clinician if irritation persists for >1 hour.
-
Inform patients that if diclofenac transdermal system begins peeling off that the edges of the system may be taped down. If problems with adhesion persist, a nonocclusive mesh netting sleeve (e.g., Curad Hold Tite™, Surgilast Tubular Elastic Dressing) may be used when appropriate (e.g., over ankles, knees, or elbows) to secure the system. Inform patients that Flector must not be worn when bathing or showering, and to wash hands after applying, handling, or removing the system. Inform patients to only apply the system to non-damaged skin.
-
Advise patients with migraine headaches that overuse of drugs intended for acute treatment of migraine attacks (e.g., use on ≥10 days per month) may exacerbate headaches; encourage patients to record the frequency of migraine headaches and medication use.
-
Stress importance of patients informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform women of reproductive potential that Arthrotec is contraindicated in pregnancy.
-
Inform pregnant women to avoid NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.
-
Advise patients who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.
-
Inform patients that diclofenac may mask the signs of an infection (e.g., fever).
-
Inform patients receiving long-term NSAIA therapy that a CBC and chemistry profiles may be monitored periodically.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs. Advise patients that concomitant use of other NSAIAs with diclofenac provides little or no increase in efficacy but increases risk of GI toxicity, and is not recommended. Advise patients not to use concomitant low-dose aspirin without consulting their clinician. Inform patients that many OTC drugs used to treat cold, fever, or insomnia contain NSAIAs.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
Transdermal System |
1.3% |
Flector |
IBSA |
|
Licart |
IBSA |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, liquid-filled |
25 mg* |
Diclofenac Potassium Capsules |
|
|
Zipsor |
Assertio |
|||
|
For oral solution |
50 mg* |
Cambia |
Assertio |
|
|
Diclofenac Potassium for Oral Solution |
||||
|
Tablets, film-coated |
25 mg* |
Diclofenac Potassium Tablets |
||
|
Cataflam |
||||
|
50 mg* |
Diclofenac Potassium Tablets |
|||
|
Cataflam |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release |
25 mg* |
Diclofenac Sodium Delayed-release Tablets |
|
|
50 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
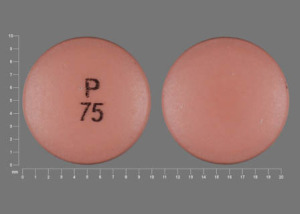
75 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
Tablets, extended-release |
100 mg* |
Diclofenac Sodium Extended-release Tablets |
||
|
Topical |
Gel |
3%* |
Diclofenac Sodium Topical Gel |
|
|
Solution |
1.5%* |
Diclofenac Sodium Topical Solution |
||
|
2%* |
Diclofenac Sodium Topical Solution |
|||
|
Ophthalmic Solution |
0.1%* |
Diclofenac Sodium Ophthalmic Solution |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release (enteric-coated core), film-coated |
50 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
||||
|
75 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
||
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Can I take ibuprofen with blood pressure medications?
- Which painkiller should you use?
- Can you Double up on Pain Medications? Safe Painkiller Combinations
- Why is diclofenac prescription only but ibuprofen is OTC?
- Can NSAIDs be used to treat a COVID-19 fever?
- Does diclofenac contain narcotics or affect a drug test?
More about diclofenac
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (702)
- Drug images
- Latest FDA alerts (11)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
- En español
Patient resources
- Diclofenac drug information
- Diclofenac (Intravenous) (Advanced Reading)
- Diclofenac (Oral) (Advanced Reading)
Professional resources
- Diclofenac prescribing information
- Diclofenac Capsule (FDA)
- Diclofenac Delayed Release Tablets (FDA)
- Diclofenac Extended Release Tablets 100mg (FDA)
- Diclofenac Oral Solution (FDA)
Other brands
Voltaren, Cataflam, Cambia, Voltaren-XR, ... +3 more