Diclofenac (Systemic, Local) (Monograph)
Brand names: Cambia, Flector, Licart, Voltaren, Zipsor
Drug class: Reversible COX-1/COX-2 Inhibitors
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke).1 302 303 317 Risk may occur early in treatment and may increase with higher dosages.1 302 303 317
-
Contraindicated in the setting of CABG surgery.1 284 302 303 317 324 326 327 328 331 336
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine).1 302 303 317 Serious GI events can occur at any time and may not be preceded by warning signs and symptoms.1 302 303 317 Geriatric individuals and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.1 302 303 317
Introduction
NSAIA; also exhibits analgesic and antipyretic activity.1
Uses for Diclofenac (Systemic, Local)
Inflammatory Diseases
Orally for symptomatic treatment of osteoarthritis (diclofenac sodium delayed-release tablets and extended-release tablets; diclofenac potassium tablets).1 81 82 84 85 86 89 90 108 109 111 112 113 114 126 133 302 303 336
Topically (as 1.5 or 2% solution) for the symptomatic treatment of osteoarthritis of the knee.326 327 337 342 343 344 345
Topically (as 1% gel) for self-medication for temporary relief of arthritis pain in the hand, wrist, elbow, foot, ankle, or knee.318 321 340 341 353
American College of Rheumatology (ACR) recommends topical/oral NSAIAs for treatment of osteoarthritis, among other interventions.330 Therapy selection is patient-specific; factors to consider include patients' values and preferences, risk factors for serious adverse GI effects, existing comorbidities (e.g., hypertension, heart failure, other cardiovascular disease, chronic kidney disease), injuries, disease severity, surgical history, and access to and availability of the interventions.330
Orally for symptomatic treatment of rheumatoid arthritis (diclofenac sodium delayed-release tablets and extended-release tablets; diclofenac potassium tablets).1 74 75 76 77 78 79 80 87 88 115 116 117 118 119 125 126 129 133 302 303 336 354 356 361
Guidelines on the treatment of rheumatoid arthritis from ACR recommend initiation of a disease-modifying antirheumatic drug (DMARD) for most patients; role of NSAIAs not discussed.2001
Orally for symptomatic treatment of ankylosing spondylitis (diclofenac sodium delayed-release tablets).1 120 127 338
Continuous NSAIA treatment is considered first-line for active ankylosing spondylitis in current guidelines.2008 On-demand NSAIAs are recommended for stable ankylosing spondylitis.2008 No preference is given to one NSAIA over another.2008
Diclofenac sodium also commercially available in an oral fixed-combination preparation with misoprostol for symptomatic treatment of rheumatoid arthritis and osteoarthritis in adults at high risk of developing NSAIA-induced gastric and duodenal ulcers and their complications.284 See full prescribing information for use of this combination product.284
Orally for management of juvenile rheumatoid arthritis† [off-label].128 210
Orally for symptomatic relief of gout† [off-label]2006 and acute painful shoulder† [off-label] .134 136 154 222 346
Pain
Orally for relief of mild to moderate pain (diclofenac potassium tablets and capsules).277 278 279 303 331 333 334 336 358
Transdermally for relief of acute pain due to minor strains, sprains, and contusions (diclofenac epolamine transdermal systems).317 320 324
American College of Physicians recommends topical NSAIAs (with or without menthol gel) as first-line therapy to reduce or relieve symptoms (including pain) and improve physical function in patients with non-low back pain musculoskeletal injury.2010 Oral NSAIAs and acetaminophen also suggested to reduce pain and (for NSAIAs) improve physical function.2010
Current guidelines on postoperative pain management recommend a multimodal approach to analgesia.2013 NSAIAs recommended as part of multimodal analgesia in patients without contraindications.2013 When selecting therapy for a specific patient, consider potential risks associated with NSAIAs.2013
Diclofenac sodium also has been used for symptomatic relief of oral surgery pain† [off-label]92 352 and low back pain† [off-label] .92
Migraine
Orally (as diclofenac potassium solution) for acute treatment of migraine attacks with or without aura; should not be used for prophylaxis of migraine.328 329
Safety and efficacy not established for treatment of cluster headache (an older, predominantly male population).328
Agents with established efficacy in adults with acute migraine include triptans, ergotamine derivatives, gepants, lasmiditan, NSAIAs (aspirin, celecoxib oral solution, diclofenac, ibuprofen, naproxen), and the combination of acetaminophen, aspirin, and caffeine.1223 Nonspecific analgesic therapies such as NSAIAs and acetaminophen/aspirin/caffeine are used for mild-to-moderate attacks, while migraine-specific therapies (e.g., triptans, ergotamine derivatives, gepants, lasmiditan) are used for moderate-to-severe attacks or mild-to-moderate attacks that respond poorly to non-specific therapy.1223 Selection of an agent for acute treatment should be based on patient-specific factors such as comorbid disease states, individual treatment history, and concomitant medications.1223
Dysmenorrhea
Orally for symptomatic management of primary dysmenorrhea (diclofenac potassium tablets).303 336 359 360
Diclofenac sodium also has been used for symptomatic management of primary dysmenorrhea.92 104 105 140
First-line treatment options for primary dysmenorrhea include combined oral contraceptives, progesterone-only contraceptives, and NSAIAs; treatment selection should be based on patient-specific considerations (e.g., comorbidities, desire/need for contraception).2012 2015 The American College of Obstetricians and Gynecologists does not address specific role for diclofenac in primary dysmenorrhea.2012
Other Uses
Diclofenac sodium ophthalmic solution used for treatment of postoperative ocular inflammation in patients undergoing cataract extraction and for temporary relief of pain and photophobia in patients undergoing corneal refractive surgery.264
Diclofenac (Systemic, Local) Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in women of reproductive potential before initiating diclofenac sodium in fixed combination with misoprostol (Arthrotec).284
-
Measure serum aminotransferase concentrations at baseline.1 302 303 317
-
Correct dehydration and hypovolemia before initiating therapy.1 284 302 303
Patient Monitoring
-
Monitor blood pressure closely when initiating diclofenac and throughout therapy.1 302 303 317
-
Obtain serum aminotransferase values 4–8 weeks after therapy with the drug is initiated and monitor periodically during long-term therapy.1 302 303 317
-
Concomitant use of nonsteroidal anti-inflammatory agents (NSAIAs), such as diclofenac, with angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, or β-adrenergic blocking agents may reduce the blood pressure response to the antihypertensive agent; therefore, monitoring of blood pressure is recommended with concomitant use of these drugs.1 302 303 317
-
Perform a CBC and chemistry profile periodically in patients receiving long-term NSAIA therapy.1 302 303 317
-
Monitor renal function during therapy in patients with preexisting renal or hepatic impairment, heart failure, dehydration, or hypovolemia.1 302 303 317
-
Monitor patients receiving NSAIAs (including those without previous symptoms of cardiovascular disease) for the possible development of cardiovascular events throughout therapy.1 302 303 317
-
Monitor patients receiving concomitant low-dose aspirin therapy for cardiac prophylaxis closely for evidence of GI bleeding.1 302 303
Dispensing and Administration Precautions
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes diclofenac on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings.999 The criteria are intended to apply to adults 65 years of age and older in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings.999 For non-COX-2-selective oral NSAIAs such as diclofenac, the Beers Criteria Expert Panel specifically recommends that chronic use be avoided unless other alternatives are not effective and the patient can take a gastroprotective agent (proton-pump inhibitor or misoprostol).999 Additionally, short-term scheduled use should be avoided in combination with oral or parenteral corticosteroids, anticoagulants, or antiplatelet agents unless other alternatives are not effective and the patient can take a gastroprotective agent.999
Other General Considerations
-
Because patients may have aspirin-sensitive asthma, patients with asthma but without known aspirin sensitivity who are receiving diclofenac should be monitored for changes in manifestations of asthma.1 302 303 317
-
To minimize the potential risk of adverse GI effects, the lowest effective dosage and shortest possible duration of therapy should be employed, and use of more than one NSAIA at a time should be avoided.1 302 303 317
-
Use of NSAIAs should be avoided in patients at higher risk of bleeding unless the benefits of therapy are expected to outweigh the increased risk of bleeding.1 302 303 317 Higher risk patients include those with a history of ulcer disease or other factors that may increase the risk for GI bleeding, including concomitant use of oral corticosteroids, anticoagulants, aspirin, or selective-serotonin reuptake inhibitors (SSRIs); longer duration of NSAIA therapy; smoking; alcohol use; older age; poor general health status; advanced liver disease; and/or coagulopathy.1 302 303 317
-
Diclofenac should be avoided in patients with recent myocardial infarction unless the benefits of therapy are expected to outweigh the risk of recurrent cardiovascular thrombotic events; if diclofenac is used in such patients, they should be monitored for cardiac ischemia.1 302 303
Administration
Oral Administration
Oral Solution
Empty the contents of one packet containing 50 mg of buffered diclofenac potassium powder for oral solution into a cup containing 30–60 mL of water, mix well, and administer immediately.328 Do not use liquids other than water.328
Administration with food may decrease peak plasma concentrations and reduce efficacy compared with administration on an empty stomach.328
Topical Administration
Diclofenac Sodium 1.5 or 2% Topical Solution
Topical 1.5% solution: Administer as drops dispensed directly onto affected knee(s); alternatively, administer into palm of hand and apply to affected knee(s).326 To avoid spillage, apply drops in 4 increments of 10 drops each per joint; following each incremental application, spread solution evenly around the front, back, and sides of the knee.326
Topical 2% solution: Administer via pump dispenser (2 pump actuations per affected joint) into palm of hand; then evenly apply the entire volume of solution around the front, back, and sides of the knee.327 Pump must be primed before first use by fully depressing the pump mechanism 4 times while holding the bottle in an upright position.327
Wait until treated area is dry before covering with clothing; wait ≥30 minutes before bathing or showering.326 327
Wash hands after application.326 327
Avoid skin-to-skin contact between other individuals and the treated area until the area is completely dry.326 327
Do not apply to open wounds, infected or inflamed areas of skin, or areas affected with exfoliative dermatitis; avoid contact with eyes and mucous membranes.326 327
Do not expose treated knee to external heat, and avoid exposing treated knee to natural or artificial sunlight; also avoid use of occlusive dressings.326 327
Allow treated knee to dry completely before applying other topical preparations (e.g., sunscreen, insect repellant, lotions, moisturizers, cosmetics, other topical medications) to the same area.326 327
Diclofenac Epolamine Transdermal System
Apply transdermal system to the most painful area once daily (Licart) or twice daily (Flector).317 324 Apply to intact skin; do not apply to damaged skin (e.g., wounds, burns, infected areas of skin, areas affected with eczema or exudative dermatitis).317 324
Wash hands after handling the system.317 324
Avoid contact with eyes and mucous membranes.317 324
Do not wear the transdermal system while bathing or showering.317 324
If a system should begin to peel off during the period of use, the edges of the system may be taped to the skin.317 324 If problems with adhesion persist, a nonocclusive mesh netting sleeve (e.g., Curad Hold Tite, Surgilast Tubular Elastic Dressing) may be used when appropriate (e.g., over ankles, knees, or elbows) to secure the system.317 324
Ophthalmic Administration
Apply 0.1% ophthalmic solution topically as an eye drop.264
Avoid use in patients with soft contact lenses (except for bandage hydrogel soft contact lenses during the first 3 days following refractive surgery).264
Dosage
Available as diclofenac potassium, diclofenac sodium, or diclofenac epolamine.1 302 303 317
Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.1 302 303 317 Adjust dosage based on individual requirements and response.1 302 303 317
Different strengths and formulations of oral diclofenac are not interchangeable.331 Commercially available diclofenac sodium delayed-release tablets, diclofenac sodium extended-release tablets, and diclofenac potassium immediate-release tablets are not necessarily bioequivalent on a mg-per-mg basis.1 302 303 336 In addition, the frequency of administration may vary across available products; diclofenac potassium liquid-filled capsules are administered 4 times daily, while diclofenac potassium conventional tablets are administered 2–4 times daily.331 336
Each actuation of the pump dispenser of diclofenac sodium 2% topical solution delivers 20 mg of diclofenac sodium in 1 g of solution.327 The 1.5% topical solution contains diclofenac sodium 16.05 mg/mL.326
Each mL of 0.1% diclofenac sodium ophthalmic solution delivers 1 mg of diclofenac sodium.264
Pediatric Patients
Acute Pain
Oral
Pediatric patients ≥12 years of age: Diclofenac potassium liquid-filled capsules: 25 mg 4 times daily.331
Topical (transdermal system)
Pediatric patients ≥6 years of age: Apply 1 transdermal system (diclofenac epolamine 1.3%) twice daily (Flector).317
Adults
Cataract Surgery
Ophthalmic
Apply 1 drop of 0.1% solution 4 times daily starting 24 hours after cataract surgery; continue for 2 weeks postoperatively.264
Corneal Refractive Surgery
Ophthalmic
Apply 1–2 drops of 0.1% solution to the operative eye 1 hour prior to surgery.264 Within 15 minutes after surgery, apply 1–2 drops to affected eye and continue 4 times daily for up to 3 days.264
Inflammatory Diseases
Osteoarthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.284
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
|
|
Diclofenac sodium delayed-release tablets |
100–150 mg daily, given as 50 mg 2 or 3 times daily or 75 mg twice daily1 |
|
Diclofenac sodium extended-release tablets |
100 mg once daily302 |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 times daily284 |
Diclofenac sodium 1.5% topical solution: 40 drops (approximately 1.2 mL) applied to each affected knee 4 times daily.326
Diclofenac sodium 2% topical solution: 40 mg (2 pump actuations) applied to each affected knee twice daily.327
Rheumatoid Arthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.284
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
|
|
Diclofenac sodium delayed-release tablets |
150–200 mg daily, given as 50 mg 3 or 4 times daily or 75 mg twice daily1 |
|
Diclofenac sodium extended-release tablets |
100 mg once daily; may increase to 100 mg twice daily 302 |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 or 4 times daily284 |
Ankylosing Spondylitis
Oral100–125 mg daily (as diclofenac sodium delayed-release tablets); administer as 25 mg 4 times daily, with 5th dose at bedtime as needed.1
Pain
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets).303 Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).303 336
25 mg 4 times daily (as diclofenac potassium liquid-filled capsules) for mild to moderate acute pain.331
Topical (transdermal system)
Apply 1 transdermal system (diclofenac epolamine 1.3%) once daily (Licart) or twice daily (Flector).317 324
Migraine
Oral
Single 50-mg dose (contents of one packet containing diclofenac potassium for oral solution mixed with water).328 Safety and efficacy of administering a second dose not established.328
Dysmenorrhea
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets).303 Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).303 336
Special Populations
Hepatic Impairment
Reduction of oral dosage may be necessary.1 302 303 331
Manufacturer of diclofenac potassium liquid-filled capsules recommends initiating treatment at the lowest dosage; if efficacy is not achieved at that dosage, discontinue diclofenac and consider alternative therapy.331
Monitoring of renal function recommended in patients with hepatic impairment.284 302 303
Renal Impairment
Reduction of oral dosage does not appear to be necessary.1 302 303
Avoid use of diclofenac in advanced renal disease unless benefits are expected to outweigh risks of therapy.284 302 303 317 If diclofenac administered, monitor patients for signs of worsening renal function.284 302 303 317
Correct volume status in dehydrated or hypovolemic patients prior to initiating diclofenac.1 284 302 303 Monitoring of renal function recommended, especially with concomitant ACE inhibitors of angiotensin II receptor antagonists,284 or in patients with heart failure, dehydration, or hypovolemia.1 302 303
Geriatric Patients
Increased risk of NSAIA-associated serious cardiovascular, gastrointestinal, and/or renal adverse effects compared to younger adults.1 284 302 303 Risk possibly increased in patients with renal impairment or those receiving concomitant ACE inhibitor or angiotensin II receptor antagonists.284 If potential benefits outweigh potential risks, initiate therapy at the lower end of the dosage range and monitor for adverse effects.1 302 303
Avoid diclofenac in fixed combination with misoprostol in geriatric patients with cardiovascular and/or renal risk factors.284 If use cannot be avoided, use the lowest recommended dosage for the shortest possible duration with additional monitoring for cardiac and renal adverse effects.284 Monitor renal function in geriatric patients receiving diclofenac in fixed combination with misoprostol, particularly during concomitant therapy with an ACE inhibitor or angiotensin II receptor antagonist.284
Cautions for Diclofenac (Systemic, Local)
Contraindications
-
Known hypersensitivity (e.g., anaphylaxis, serious dermatologic reactions) to diclofenac or any ingredient in the formulation.1 264 284 302 303 317 324 326 327 328 331 336
-
History of asthma, urticaria, or other sensitivity reaction precipitated by aspirin or other NSAIAs.1 302 303 317 324 326 327 328 331 336
-
In the setting of CABG surgery.1 284 302 303 317 324 326 327 328 331 336
-
Diclofenac sodium in fixed combination with misoprostol: Active GI bleeding.284
-
Diclofenac sodium in fixed combination with misoprostol: Pregnancy.284
-
Diclofenac potassium liquid-filled capsules: Hypersensitivity to bovine protein.331
-
Diclofenac epolamine transdermal system: Use on nonintact or damaged skin, regardless of etiology (e.g., exudative dermatitis, eczema, infected lesions, burns, wounds).317 324
Warnings/Precautions
Warnings
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease (see Boxed Warning).1 302 303
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.1 302 303
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.1 302 303
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.1 302 303
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.1 302 303
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI; absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.1 302 303
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.1 302 303 317
Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia.1 302 303 Contraindicated in the setting of CABG surgery.1 302 303
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events associated with NSAIAs.1 302 303 317
GI Bleeding, Ulceration, and Perforation
Serious, sometimes fatal, GI toxicity (e.g., bleeding, ulceration, perforation of esophagus, stomach, or small or large intestine) can occur with or without warning symptoms (see Boxed Warning).1 302 303 317
Risk for GI bleeding increased more than tenfold in patients with a history of peptic ulcer disease and/or GI bleeding who are receiving NSAIAs compared with patients without these risk factors.1 302 317
Other risk factors for GI bleeding include concomitant use of oral corticosteroids, anticoagulants, aspirin, or SSRIs; longer duration of NSAIA therapy; smoking; alcohol use; older age; poor general health status; and advanced liver disease and/or coagulopathy.1 302 303 317
Use at lowest effective dosage for the shortest duration necessary.1 302 303 317
Avoid use of more than one NSAIA at a time.1 302 303 317
Avoid use of NSAIAs in patients at higher risk for GI toxicity unless expected benefits outweigh increased risk of bleeding; consider alternate therapies in high-risk patients and those with active GI bleeding.1 302 303 317
Monitor for GI ulceration and bleeding; even closer monitoring for GI bleeding recommended in those receiving concomitant low-dose aspirin for cardiac prophylaxis.1 302 303 317
If serious adverse GI event suspected, promptly initiate evaluation and discontinue diclofenac until serious adverse GI event ruled out.1 302 303 317
Other Warnings and Precautions
Heart Failure and Edema
Fluid retention and edema reported.1 302 303 317
NSAIAs increase the risk of MI, hospitalization for heart failure, and death.1 302 303 317
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema.1 302 303 317
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.1 302 303 317
Hepatotoxicity
Monitor for symptoms and/or signs suggesting liver dysfunction.1 302 303 317
Measure serum aminotransferase concentrations at baseline and 4–8 weeks after initiating therapy; monitor periodically during long-term therapy.1 302 303 317
Use at lowest effective dosage for the shortest duration necessary; use with caution in patients receiving other potentially hepatotoxic drugs (e.g., acetaminophen, certain antibiotics, anticonvulsant agents).1 302 303 317
Discontinue immediately if abnormal liver function test results persist or worsen, if clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations (e.g., eosinophilia, rash) occur.1 302 303 317
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events.1 302 303 317
Monitor BP during initiation of diclofenac and throughout therapy.1 302 303 317
Impaired response to ACE inhibitors and certain diuretics may occur.1 302 303 317
Renal Toxicity and Hyperkalemia
Potential for overt renal decompensation.1 302 303 317 Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure, in geriatric patients, in patients with volume depletion, and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist.1 302 303 317
Correct fluid depletion prior to initiating diclofenac; monitor renal function during therapy in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia.1 302 303 317
Hyperkalemia reported with NSAIAs, even in some patients without renal impairment; in such patients, effects attributed to a hyporenin-hypoaldosterone state.1 302 303 317
Anaphylactic Reactions
Anaphylactic reactions reported in patients with and without known hypersensitivity to diclofenac and in patients with aspirin-sensitive asthma.1 302 303 317
Exacerbation of Asthma Related to Aspirin Sensitivity
Patients with asthma can have aspirin-sensitive asthma, which manifests principally as chronic rhinosinusitis with severe (possibly fatal) bronchospasm and usually nasal polyps.1 302 303 317
Avoid in patients with cross-sensitivity to aspirin.1 302 303 317 In patients with asthma but without known aspirin sensitivity, monitor for changes in manifestations of asthma.1 302 303 317
Serious Skin Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning.1 302 303 317 Fixed drug eruption (FDE), or more severe, potentially life-threatening generalized bullous fixed drug eruption (GBFDE) can occur.1 302 303 317
Discontinue at first appearance of rash or any other sign of hypersensitivity (e.g., blisters, fever, pruritus).1 302 303 317
Drug Reaction with Eosinophilia and Systemic Symptoms
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs.1 302 303 317 Clinical presentation variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).1 302 303 317 Symptoms may resemble those of acute viral infection.1 302 303 317 Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in absence of rash.1 302 303 317 If signs or symptoms of DRESS develop, discontinue diclofenac and immediately evaluate the patient.1 302 303 317
Fetal/Neonatal Morbidity and Mortality
NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus, and use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios, and in some cases, neonatal renal impairment.1 302 303 317
Avoid NSAIAs in pregnant women at about ≥30 weeks of gestation; if NSAIA therapy necessary between about 20−30 weeks of gestation, use lowest effective dosage and for shortest possible duration.1 302 303 317
Fixed combination of diclofenac and misoprostol: Contraindicated in pregnant women.284 Misoprostol exhibits abortifacient activity and can cause serious fetal harm.284 Use in women of reproductive potential only if they require NSAIA therapy and are considered at high risk of complications resulting from NSAIA-induced gastric or duodenal ulceration or at high risk of developing gastric or duodenal ulceration.284
Verify pregnancy status in women of reproductive potential within 2 weeks of initiating diclofenac sodium in fixed combination with misoprostol.284
Hematologic Toxicity
Anemia reported.1 302 303 317 May be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis.1 302 303 317 Determine hemoglobin concentration or hematocrit if signs or symptoms of anemia or blood loss occur.1 302 303 317
NSAIAs may increase the risk of bleeding.1 302 303 317 Patients with certain coexisting conditions (e.g., coagulation disorders) or receiving concomitant therapy with anticoagulants, antiplatelet agents, or serotonin-reuptake inhibitors may be at increased risk; monitor such patients for bleeding.1 302 303 317
Masking of Inflammation and Fever
Antipyretic and anti-inflammatory effects of diclofenac may mask usual signs and symptoms of infection.1 302 303 317
Laboratory Monitoring
Monitor CBC and chemistry profile periodically in patients receiving long-term therapy.1 302 303 317
Precautions Specific to Transdermal or Other Topical Use
Avoid exposure of treated areas to natural or artificial sunlight.326 327 The potential effects of topical diclofenac gel or solution on skin response to UV damage in humans are not known.326 327
Application to nonintact skin may alter absorption and tolerability; apply only to intact skin.326 327
Avoid contact with the eyes and mucous membranes.326 327 If contact with the eyes occurs, thoroughly rinse the eyes with water or saline.326 327 If ocular irritation persists for >1 hour, consult a clinician.326 327
Do not apply to nonintact or damaged skin.317 324
Patient should bathe or shower after removing one transdermal system and before applying a new system; the transdermal system should not be worn during bathing or showering.317 324
Store and discard transdermal systems in a manner that avoids accidental exposure or ingestion by children or pets.317 324
Medication Overuse Headache
Excessive use of drugs indicated for the management of acute migraine attacks (e.g., use of NSAIAs, 5-HT1 receptor agonists, ergotamine, or opiates on a regular basis for ≥10 days per month) may result in migraine-like daily headaches or a marked increase in the frequency of migraine attacks.328 Detoxification, including withdrawal of the overused drugs and treatment of withdrawal symptoms (which often include transient worsening of headaches), may be necessary.328
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.1 302 303 317
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice.1 302 303 317
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs.1 302 303 317 Oligohydramnios is often, but not always, reversible following NSAIA discontinuance.1 302 303 317 Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation.1 302 303 317 In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios.1 302 303 317 Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis).1 302 303 317 Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of risk of adverse fetal and neonatal outcomes with maternal NSAIA use.1 302 303 317 Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants uncertain.1 302 303 317
Effects of diclofenac on labor and delivery not known.1 302 303 In animal studies, NSAIAs, including diclofenac, increased incidence of dystocia, delayed parturition, and increased stillbirths.1 302 303
Fixed combination of diclofenac and misoprostol: Contraindicated in pregnant women.284 Misoprostol exhibits abortifacient activity and can cause serious fetal harm.284
Lactation
May be distributed into human milk; consider the developmental and health benefits of breast-feeding along with the mother's clinical need for diclofenac and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.1 302 303 317
Females and Males of Reproductive Potential
NSAIAs may be associated with reversible infertility in some women.1 302 303 317 Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.1 302 303 317
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.1 302 303 317
Pediatric Use
Safety and efficacy of diclofenac epolamine transdermal system (Flector) established in pediatric patients ≥6 years of age; safety comparable between pediatric patients and adults.317
Safety and efficacy of diclofenac epolamine transdermal system (Flector) not established in pediatric patients <6 years of age.317
Safety and efficacy of diclofenac potassium liquid-filled capsules established in pediatric patients 12−17 years of age; plasma concentrations of diclofenac similar to those observed in adult patients.331
Safety and efficacy of other formulations of diclofenac not established in children.1 302 303 324 326 327 328 336
Good results with oral diclofenac obtained in a limited number of children 3–16 years of age for the management of juvenile rheumatoid arthritis† .128 210
Geriatric Use
Increased risk for serious adverse cardiovascular, GI, and renal effects.1 302 303 317 Risk of these adverse effects may be increased in geriatric patients with renal impairment or who are receiving concomitant ACE inhibitor or angiotensin II receptor antagonist therapy.284 Many of the spontaneous fatal adverse GI effects in patients receiving NSAIAs involve geriatric patients.1 302 303 317 If anticipated benefits outweigh potential risks, initiate at lower end of dosing range and monitor for adverse effects.1 302 303 317
Diclofenac sodium 1.5% topical solution: No age-related differences in incidence of adverse effects observed.326 327
Diclofenac epolamine transdermal system: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.317 324
Diclofenac potassium oral solution: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.328
Diclofenac sodium in fixed combination with misoprostol: Avoid in geriatric patients with cardiovascular and/or renal risk factors.284
Use diclofenac with caution because of age-related decreases in renal function.302 303 May be useful to monitor renal function.302 303
Hepatic Impairment
Almost completely metabolized in the liver; reduction of oral dosage may be necessary.1 302 303
Diclofenac oral solution should only be used in patients with hepatic impairment if benefits outweigh risks.328
Diclofenac epolamine transdermal system: Pharmacokinetics not evaluated in hepatic impairment.317 324
Renal Impairment
No differences in diclofenac pharmacokinetics observed in patients with renal insufficiency.1 302 303 Avoid use in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function.1 302 303
Diclofenac epolamine transdermal system: Pharmacokinetics not evaluated in renal impairment.284
Common Adverse Effects
Diclofenac sodium delayed-release tablets, diclofenac potassium conventional tablets, or other NSAIAs (reported in 1–10% of patients): GI effects (abdominal pain, constipation, diarrhea, dyspepsia, flatulence, gross bleeding/perforation, heartburn, nausea, GI ulcers, and vomiting).1 303 Additionally, abnormal renal function, anemia, dizziness, edema, elevations in hepatic transaminases, headaches, increased bleeding time, pruritic, rashes, and tinnitus.1 303
Diclofenac in fixed combination with misoprostol (reported in ≥2% of patients): Abdominal pain, diarrhea, dyspepsia, nausea, flatulence, gastritis, vomiting, constipation, headache, dizziness, increases in ALT, and decreases in hematocrit.284
Diclofenac epolamine transdermal system (Flector): Pruritis (5%) and nausea (3%) reported.317 The most common adverse effects in pediatric patients were headache (9%) and application site pruritis (7%).317 Application site pruritis and application site reactions also common adverse effects in patients receiving diclofenac epolamine transdermal system (Licart).324
Diclofenac potassium for oral solution (reported in ≥1% of patients): Nausea and dizziness.328
Diclofenac sodium ophthalmic solution: Transient burning and stinging (15%), elevated intraocular pressure following cataract surgery (15%) and keratitis in up to 28% of patients, although keratitis was noted prior to treatment in many of these patients.264 Lacrimation complaints were also reported in approximately 30% of cases undergoing incisional refractive surgery.264 Other adverse effects reported in ≤10% of patients include abnormal vision, acute elevated intraocular pressure, blurred vision, conjunctivitis, corneal deposits, corneal edema, corneal opacity, corneal lesions, discharge, eyelid swelling, eye pain, injection (redness), iritis, irritation, itching, lacrimation disorder, and ocular allergy.264
Drug Interactions
Metabolized by CYP isoenzymes, mainly CYP2C9.302 CYP3A4, uridine diphosphate-glucuronosyltransferase (UGT) 2B7, and CPY2C8 may contribute to metabolism.302
Drugs Affecting Hepatic Microsomal Enzymes
CYP2C9 inhibitors: Possible increased systemic exposure to diclofenac and risk of adverse effects. 302 Dosage adjustment may be required.302 Examples include, but are not limited to, voriconazole.302
CYP2C9 inducers: Possible reduced efficacy of diclofenac.302 Dosage adjustment may be required.302 Examples include, but are not limited to, rifampin.302
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor1 302 303 317 Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment302 |
Monitor BP302 Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter302 Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function302 |
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonist1 302 303 317 Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment302 |
Monitor BP302 Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter302 Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function302 |
|
Antacids |
Delayed diclofenac absorption284 |
|
|
Anticoagulants (warfarin) |
Caution advised; carefully observe for signs of bleeding 302 |
|
|
β-Adrenergic blocking agents |
Monitor BP302 |
|
|
Cyclosporine |
Possible increase in nephrotoxic effects of cyclosporine1 302 303 |
Monitor for worsening renal function302 |
|
Digoxin |
Increased serum concentrations and prolonged half-life of digoxin302 |
Monitor serum digoxin concentrations302 |
|
Diuretics (furosemide, thiazides, potassium-sparing) |
Reduced natriuretic effects1 302 303 317 Concomitant use of potassium-sparing diuretics may be associated with increased serum potassium concentrations284 |
Monitor for worsening renal function and for adequacy of diuretic and antihypertensive effects1 302 303 317 |
|
Lithium |
||
|
Methotrexate |
Possible increased risk of methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction)302 |
Monitor for methotrexate toxicity302 |
|
NSAIAs |
Concomitant NSAIAs and aspirin (analgesic dosages): Therapeutic effect not greater than that of NSAIAs alone302 Concomitant NSAIAs and aspirin: Increased risk for bleeding and serious adverse GI effects302 Concomitant use of oral and topical NSAIAs may result in higher incidence of hemorrhage and abnormal Scr, urea, and hemoglobin concentrations317 324 Protein binding of NSAIAs reduced by aspirin, but clearance of unbound NSAIA not altered; clinical importance unknown302 No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs302 317 |
Concomitant use of diclofenac with analgesic dosages of aspirin generally not recommended302 Do not use topical diclofenac formulations with oral NSAIAs unless expected benefits outweigh risks and periodic laboratory evaluations are performed317 324 Advise patients not to take low-dose aspirin without consulting clinician; closely monitor patients receiving concomitant antiplatelet agents (e.g., aspirin) for bleeding302 |
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity302 |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid administration beginning 2 days before and continuing through 2 days after pemetrexed administration302 Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid administration beginning at least 5 days before and continuing through 2 days after pemetrexed administration302 Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity302 |
|
Serotonin-reuptake inhibitors (e.g., SSRIs, SNRIs) |
Possible increased risk of bleeding302 |
Monitor for bleeding302 |
|
Voriconazole |
Peak concentration and AUC of diclofenac increased by 114 and 78%, respectively302 |
Dosage adjustment may be required302 |
Diclofenac (Systemic, Local) Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.1 302 303 Undergoes first-pass metabolism; only 50% of a dose reaches systemic circulation as unchanged drug.1 302 303
Peak plasma concentration usually attained within about 0.47 hours (diclofenac potassium liquid-filled capsules), 1 hour (diclofenac potassium conventional tablets), 2.3 hours (diclofenac sodium delayed-release tablets), or 5.3 hours (diclofenac sodium extended-release tablets).1 302 303 331 336
Absorbed into systemic circulation following topical administration as gel, solution, or transdermal system; plasma concentrations generally very low compared with oral administration.317 324 326
Following application of a single diclofenac epolamine transdermal system (Flector) to intact skin on the upper arm, peak plasma concentrations occur in 10–20 hours; moderate exercise does not alter absorption.317 Plasma diclofenac concentrations similar in pediatric patients ≥6 years of age compared to adults.317
Following application of diclofenac epolamine transdermal system (Licart) to anterior thigh, peak concentrations occur in 4–20 hours; moderate exercise, application of an occlusion dressing over the system, or moderate heat increases peak plasma concentrations and systemic exposure by approximately 20%.324
Following topical application of diclofenac sodium 1.5% solution to knees, peak plasma concentrations occur in about 4 hours.326 Not established whether occlusive dressings, application of heat, or exercise affects absorption of diclofenac sodium 2% solution.327
Food
Conventional, delayed-release, or extended-release tablets: Food delays time to reach peak plasma concentration but does not affect extent of absorption.1 302 303
Diclofenac potassium oral solution: Administration after a high-fat meal reduces peak plasma concentrations by approximately 70% but does not substantially affect extent of absorption.328
Diclofenac potassium liquid-filled capsules: Food decreases rate of absorption (47% decrease in peak concentration, twofold increase in time to peak concentration) but does not substantially affect extent of absorption.331
Distribution
Extent
Distributes into human milk.1 302 303
Plasma Protein Binding
Elimination
Metabolism
Metabolized in the liver via hydroxylation and conjugation.1 302 303 Five metabolites detected in plasma and urine.302
Formation of 4′-hydroxydiclofenac (principal metabolite) is mediated mainly by CYP2C9; formation of 5-hydroxydiclofenac and 3′-hydroxydiclofenac (minor metabolites) is mediated by CYP3A4.302 UGT2B7 and CYP2C8 may mediate acyl glucuronidation and oxidation reactions, respectively.302
Elimination Route
Excreted in urine (65%) and in feces via biliary elimination (35%).302
Half-life
Diclofenac sodium: 2.3 hours.1 302
Diclofenac potassium: 1.9 hours.303
Diclofenac epolamine transdermal system: Approximately 12 hours.317 324
Special Populations
In patients with renal impairment, plasma clearance not substantially altered.1 302 303
Stability
Storage
Oral
Capsules, Liquid-filled
Tight container at 20–25°C (may be exposed to 15–30°C).331 Protect from moisture.331
Powder for Oral Solution
25°C (may be exposed to 15–30°C).328
Tablets
Tight containers at room temperature (20–25°C); consult manufacturer's labeling for specific storage recommendation.1 302 303 Protect from moisture.302 303
Diclofenac sodium in fixed combination with misoprostol: 25°C (may be exposed to 15–30°C).284
Topical
Solution
Diclofenac sodium 0.1% ophthalmic solution: 20–25°C protected from light.264
Diclofenac sodium 1.5% topical solution: 20–25°C (may be exposed to 15–30°C).326
Diclofenac sodium 2% topical solution: 25°C (may be exposed to 15–30°C).327
Transdermal System
20–25°C (may be exposed to 15–30°C).317 324 Licart systems stable for up to 6 months after envelope is opened if stored at room temperature in the resealed envelope.324
Actions
-
NSAIA; inhibits cyclooxygenase-1 (COX-1) and COX-2.1
-
Mode of action associated principally with reduction of prostaglandin synthesis in peripheral tissues;1 exhibits anti-inflammatory, analgesic, and antipyretic activity.1 317
Advice to Patients
-
Advise patients to read the medication guide for nonsteroidal anti-inflammatory agents (NSAIAs) that is provided each time the drug is dispensed.1 284 302 303 317 324 326 327 328 331
-
Inform patients of the risk of serious cardiovascular thrombotic events.1 284 302 303 317 324 326 327 328 331 Stress importance of reporting signs and symptoms of a cardiovascular event (e.g., chest pain, shortness of breath, weakness, slurred speech) immediately to a healthcare provider.1 284 302 303 317 324 326 327 328 331
-
Inform patients to report symptoms of GI bleeding and ulceration (e.g., epigastric pain, dyspepsia, melena, hematemesis) to their healthcare provider.1 284 302 303 317 324 326 327 328 331 Notify patients receiving concomitant low-dose aspirin of the increased risk of GI bleeding.1 284 302 303 317 324 326 327 328 331
-
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, anorexia, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms).1 284 302 303 317 324 326 327 328 331 If these occur, inform patients to stop diclofenac and seek immediate medical attention.1 284 302 303 317 324 326 327 328 331
-
Inform patients of the risk of serious skin reactions, including drug reaction with eosinophilia and systemic symptoms (DRESS).1 284 302 303 317 324 326 327 328 331 Advise patients to stop taking diclofenac immediately if they develop any type of rash or fever and to promptly contact their clinician.1 284 302 303 317 324 326 327 328 331
-
Stress importance of seeking immediate medical attention if an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat) occurs.1 284 302 303 317 324 326 327 328 331
-
Inform patients of the risk of heart failure or edema, and to watch out for symptoms of heart failure such as shortness of breath, unexplained weight gain, or edema, and to contact their healthcare provider if these occur.1 284 302 303 317 324 326 327 328 331
-
Warn patients to keep diclofenac transdermal system out of the reach of children and pets and to safely dispose of used units.317 324
-
Stress importance of avoiding or limiting exposure of skin treated with diclofenac gel or solution to natural or artificial sunlight.326 327
-
Advise patients receiving diclofenac topical solution to avoid applying to open wounds, infections, inflammation, or exfoliative dermatitis.326 327
-
Advise patients receiving diclofenac topical solution to wait until the treated area is completely dry before applying sunscreen, insect repellent, lotion, moisturizer, cosmetics, or other topical medications.326 327
-
Advise patients receiving diclofenac topical solution to promptly contact their clinician if any type of rash develops at the application site.326 327
-
Advise patients receiving diclofenac topical solution that other individuals should avoid contact with the application site(s) until the site is completely dry.326 327
-
Inform patients that if topical formulations of diclofenac come into contact with the eye(s), to rinse the affected eye(s) with water or saline and consult a clinician if irritation persists for >1 hour.326 327
-
Inform patients that if diclofenac transdermal system begins peeling off that the edges of the system may be taped down.317 324 If problems with adhesion persist, a nonocclusive mesh netting sleeve (e.g., Curad Hold Tite™, Surgilast Tubular Elastic Dressing) may be used when appropriate (e.g., over ankles, knees, or elbows) to secure the system.317 324 Inform patients that Flector must not be worn when bathing or showering, and to wash hands after applying, handling, or removing the system.317 Inform patients to only apply the system to non-damaged skin.317 324
-
Advise patients with migraine headaches that overuse of drugs intended for acute treatment of migraine attacks (e.g., use on ≥10 days per month) may exacerbate headaches; encourage patients to record the frequency of migraine headaches and medication use.328
-
Stress importance of patients informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 284 302 303 317 324 326 327 328 331
-
Inform women of reproductive potential that Arthrotec is contraindicated in pregnancy.284
-
Inform pregnant women to avoid NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.1 284 302 303 317 324 326 327 328 331
-
Advise patients who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.1 284 302 303 317 324 326 327 328 331
-
Inform patients that diclofenac may mask the signs of an infection (e.g., fever).1 284 302 303 317 324 326 327 328 331
-
Inform patients receiving long-term NSAIA therapy that a CBC and chemistry profiles may be monitored periodically.1 284 302 303 317 324 326 327 328 331
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.1 284 302 303 317 324 326 327 328 331 Advise patients that concomitant use of other NSAIAs with diclofenac provides little or no increase in efficacy but increases risk of GI toxicity, and is not recommended.1 284 302 303 317 324 326 327 328 331 Advise patients not to use concomitant low-dose aspirin without consulting their clinician.1 284 302 303 317 324 326 327 328 331 Inform patients that many OTC drugs used to treat cold, fever, or insomnia contain NSAIAs.1 284 302 303 317 324 326 327 328 331
-
Inform patients of other important precautionary information.1 284 302 303 317 324 326 327 328 331
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
Transdermal System |
1.3% |
Flector |
IBSA |
|
Licart |
IBSA |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, liquid-filled |
25 mg* |
Diclofenac Potassium Capsules |
|
|
Zipsor |
Assertio |
|||
|
For oral solution |
50 mg* |
Cambia |
Assertio |
|
|
Diclofenac Potassium for Oral Solution |
||||
|
Tablets, film-coated |
25 mg* |
Diclofenac Potassium Tablets |
||
|
Cataflam |
||||
|
50 mg* |
Diclofenac Potassium Tablets |
|||
|
Cataflam |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release |
25 mg* |
Diclofenac Sodium Delayed-release Tablets |
|
|
50 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
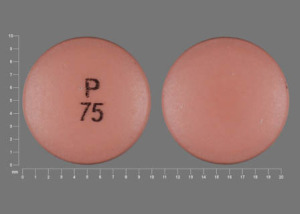
75 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
Tablets, extended-release |
100 mg* |
Diclofenac Sodium Extended-release Tablets |
||
|
Topical |
Gel |
3%* |
Diclofenac Sodium Topical Gel |
|
|
Solution |
1.5%* |
Diclofenac Sodium Topical Solution |
||
|
2%* |
Diclofenac Sodium Topical Solution |
|||
|
Ophthalmic Solution |
0.1%* |
Diclofenac Sodium Ophthalmic Solution |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release (enteric-coated core), film-coated |
50 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
||||
|
75 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
||
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Carlsbad Technology, Inc. Diclofenac sodium delayed-release tablets prescribing information. Carlsbad, CA; 2024 Jul.
74. Bendix T, Schmidt I, Rasmussen KJE et al. Diclofenac (Voltaren) and ketoprofen (Orudis), in rheumatoid arthritis: a randomized double-blind multicentre trial. Curr Ther Res. 1983; 33:192-9.
75. Huntwork JC. Efficacy and safety of diclofenac compared with aspirin in the treatment of rheumatoid arthritis. Curr Ther Res. 1986; 40:576-86.
76. Keiding G, Sorensen K. A randomized, double- blind, within-patient trial of diclofenac sodium (Voltaren) and naproxen in the treatment of rheumatoid arthritis. Curr Ther Res. 1981; 29:183-92.
77. Hirsch U. Effect and tolerability of diclofenac and indomethacin administered per os and as suppositories: a comparative trial. Curr Ther Res. 1980; 28:359-66.
78. Meyers OL, Quantock OP, Joubert PG et al. A multicentre trial of Voltaren in the treatment of rheumatoid arthritis. S Afr Med J. 1974; 48:2013-7. https://pubmed.ncbi.nlm.nih.gov/4612752
79. Caldwell JR. Efficacy and safety of diclofenac sodium in rheumatoid arthritis: experience in the United States. Am J Med. 1986; 80(Suppl 4B):43-7. https://pubmed.ncbi.nlm.nih.gov/3518432
80. Zuckner J. International experience with diclofenac in rheumatoid arthritis. Am J Med. 1986; 80(Suppl 4B):39-42. https://pubmed.ncbi.nlm.nih.gov/3518431
81. Ward JR. Efficacy of diclofenac in osteoarthritis. Am J Med. 1986; 80(Suppl 4B):53-7. https://pubmed.ncbi.nlm.nih.gov/3518434
82. Altman R. International experiences with diclofenac in osteoarthritis. Am J Med. 1986; 80(Suppl 4B):48-52. https://pubmed.ncbi.nlm.nih.gov/3518433
83. Amundsen T, Bleken L, Borkje B et al. Variation in response to naproxen and diclofenac in patients with osteoarthritis. Curr Ther Res. 1983; 33:793-801.
84. Germain BF. A placebo-controlled study of diclofenac sodium for the treatment of osteoarthritis of the hip and knee. Curr Ther Res. 1985; 37:259-68.
85. Schubiger BI, Ciccolunghi SN, Tanner K. Once daily dose treatment with a non-steroidal anti- rheumatic drug (diclofenac) in osteoarthrosis. J Int Med Res. 1980; 8:167-74. https://pubmed.ncbi.nlm.nih.gov/6989687
86. Vetter G. A comparison of naproxen and diclofenac sodium in the treatment of osteoarthritis in elderly patients. Br J Clin Pract. 1985; 39:276-281. https://pubmed.ncbi.nlm.nih.gov/3896286
87. Eidsaunet W, Borkje B, Larsen S et al. Response to two NSAIDs: diclofenac and naproxen in rheumatoid arthritis. Curr Ther Res. 1983; 33:966-75.
88. Lizarazo PH, Cortes MP. Single-blind parallel study comparing naproxen with sulindac and with diclofenac in rheumatoid arthritis. Curr Ther Res. 1983; 34:701-7.
89. Siraux P. Diclofenac (Voltaren) for the treatment of osteo-arthrosis: a double-blind comparison with naproxen. J Int Med Res. 1977; 5:169-74. https://pubmed.ncbi.nlm.nih.gov/330288
90. Crook PR, Fowler PD, Hothersall TE et al. A study of the efficacy and tolerability of diclofenac and ibuprofen in osteoarthritis of the hip. Br J Clin Pract. 1981; 35:309-12. https://pubmed.ncbi.nlm.nih.gov/7034760
91. Calabro JJ. Efficacy of diclofenac in ankylosing spondylitis. Am J Med. 1986; 80(Suppl 4B):58-63. https://pubmed.ncbi.nlm.nih.gov/3518435
92. Kantor TG. Use of diclofenac in analgesia. Am J Med. 1986; 80(Suppl 4B):64-9. https://pubmed.ncbi.nlm.nih.gov/2939715
104. Ingemanson CA, Sikstrom B, Bjorkman R. Comparison between diclofenac and naproxen in the treatment of primary dysmenorrhoea. Curr Ther Res. 1984; 36:1203-09.
105. Ingemanson CA, Carrington B, Sikstrom B et al. Diclofenac in the treatment of primary dysmenorrhoea. Curr Ther Res. 1981; 30:632-9.
108. Berry H, Bloom B, Hamilton EBD. A comparative study of piroxicam (Feldene) diclofenac and placebo in osteoarthritis. Clin Trials J. 1982; 19:349-58.
109. Marcolongo R, Giordano N, Bassi GP et al. Double-blind preference and compliance multicentre study in osteoarthritis: once-a-day treatment. Clin Rheumatol. 1985; 4:267-77. https://pubmed.ncbi.nlm.nih.gov/3905218
110. Scharf Y, Nahir M, Schapira D et al. A comparative study of naproxen with diclofenac sodium in osteoarthrosis of the knees. Rheumatol Rehabil. 1982; 21:167-70. https://pubmed.ncbi.nlm.nih.gov/7048497
111. Car A, Jajic I, Krampac I et al. A double- blind multicentre comparison of diclofenac sodium and naproxen in osteoarthrosis of the hip. Scand J Rheumatol. 1978; Suppl 22:63-8.
112. Chiswell RJ, Grieve AP, MacDonald IR. An interim report on a multicentre general practice study of Voltarol: 2. Osteoarthritis. Br J Clin Pract. 1984; 34:207-10.
113. Aylward M, Maddock J, Lewis PA et al. Mefenamic acid and diclofenac sodium in osteoarthritis of the weight bearing joints: a double blind comparison. Br J Clin Pract. 1985; 39:135-9. https://pubmed.ncbi.nlm.nih.gov/3893502
114. Joubert PH, Kushlick AR, McNeill WG et al. South African multicentre trial with Voltaren in osteo- arthritis of the knee. S Afr Med J. 1974; 48:1973-8. https://pubmed.ncbi.nlm.nih.gov/4608209
115. Huskisson EC, Dieppe PA, Scott J et al. Diclofenac sodium, diflunisal and naproxen: patient preferences for anti-inflammatory drugs in rheumatoid arthritis. Rheumatol Rehabil. 1982; 21:238-42. https://pubmed.ncbi.nlm.nih.gov/7134745
116. Kirchheiner B, Trang L, Wollheim FA. Diclophenac sodium (Voltaren) in rheumatoid arthritis: a double-blind comparison with indomethacin and placebo. Int J Clin Pharmacol. 1976; 13:292-7.
117. Weisman MH. Double-blind randomized trial of diclofenac sodium versus placebo in patients with rheumatoid arthritis. Clin Ther. 1986; 8:427-38. https://pubmed.ncbi.nlm.nih.gov/3524843
118. Dürrigl T, Vitaus M, Pucar I et al. Diclofenac sodium (Voltaren): results of a multi-centre comparative trial in adult-onset rheumatoid arthritis. J Int Med Res. 1975; 3:139-44. https://pubmed.ncbi.nlm.nih.gov/162669
119. Tannenbaum H, Esdaile J, Topp JR et al. A double-blind, multicenter, controlled study on diclofenac (Voltaren) and naproxen in patients with rheumatoid arthritis (R.A.). Curr Ther Res. 1984; 35:357-62.
120. Nahir AM, Scharf Y. A comparative study of diclofenac and sulindac in ankylosing spondylitis. Rheumatol Rehabil. 1980; 19:193-8. https://pubmed.ncbi.nlm.nih.gov/6997973
125. Ciccolunghi SN, Chaudri HA, Schubiger BI et al. Report on a long-term tolerability study of up to two years with diclofenac sodium (voltaren). Scand J Rheumatol. 1978; 22(Suppl):86-96.
126. Caldwell JR. Diclofenac sodium in the treatment of rheumatoid arthritis and osteoarthritis. Semin Arthritis Rheum. 1985; 15:73-9. https://pubmed.ncbi.nlm.nih.gov/4081794
127. Khan MA. A double blind comparison of diclofenac and indomethacin in the treatment of ankylosing spondylitis. J Rheumatol. 1987; 14:118-23. https://pubmed.ncbi.nlm.nih.gov/3553586
128. Haapasaari J, Wuolijoki E, Ylijoki H. Treatment of juvenile rheumatoid arthritis with diclofenac sodium. Scand J Rheumatol. 1983; 12:325- 30. https://pubmed.ncbi.nlm.nih.gov/6361986
129. Bijlsma A. The long-term efficacy and tolerability of Voltaren (diclofenac sodium) and indomethacin in rheumatoid arthritis. Scand J Rheumatol. 1978; 22:74-80.
133. Machtey I. Diclofenac in the treatment of painful joints and traumatic tendinitis (including strains and sprains): a brief review. Semin Arthritis Rheum. 1985; 15:87-92. https://pubmed.ncbi.nlm.nih.gov/4081796
134. Huskisson EC, Bryans R. Diclofenac sodium in the treatment of painful stiff shoulder. Curr Med Res Opin. 1983; 8:350-3. https://pubmed.ncbi.nlm.nih.gov/6340976
136. Famaey JP, Ginsberg F. Treatment of periarthritis of the shoulder: a comparison of ibuprofen and diclofenac. J Int Med Res. 1984; 12:238-43. https://pubmed.ncbi.nlm.nih.gov/6381167
140. Riihiluoma P, Wuolijoki E, Pulkkinen MO. Treatment of primary dysmenorrhea with diclofenac sodium. Eur J Obstet Gynecol Reprod Biol. 1981; 12:189-194. https://pubmed.ncbi.nlm.nih.gov/7028529
154. Valtonen EJ. A comparative short-term trial with Voltaren (diclofenac sodium) and naproxen in soft-tissue rheumatism. Scand J Rheumatol. 1978; 22:69-73.
210. Leak AM, Richter MR, Clemens LE et al. A crossover study of naproxen, diclofenac and tolmetin in seronegative juvenile chronic arthritis. Clin Exp Rheumatol. 1988; 6:157-60. https://pubmed.ncbi.nlm.nih.gov/3052965
222. Flygare U, Seuri M, Hurme J et al. Relief of spasm with diclofenac. Clin Rheum. 1988; 7:124-5.
227. Alembic Pharmaceuticals, Inc. Diclofenac sodium 3% topical gel prescribing information. Bedminster, NJ: 2025 Jan.
264. Bausch & Lomb Inc. Diclofenac sodium 0.1% ophthalmic solution prescribing information. Tampa, FL; 2022 Jun.
277. Morán M. Double-blind comparison of diclofenac potassium, ibuprofen and placebo in the treatment of ankle sprains. J Int Med Res. 1991; 19:121-30. https://pubmed.ncbi.nlm.nih.gov/1864448
278. Morán M. An observer-blind comparison of diclofenac potassium, piroxicam and placebo in the treatment of ankle sprains. Curr Med Res Opin. 1990; 12:268-74. https://pubmed.ncbi.nlm.nih.gov/2127562
279. Bahamonde LA, Saavedra H. Comparison of the analgesic and anti-inflammatory effects of diclofenac potassium versus piroxicam versus placebo in ankle sprain patients. J Int Med Res. 1990; 18:104-11. https://pubmed.ncbi.nlm.nih.gov/2111251
284. Pfizer. Arthrotec (diclofenac sodium and misoprostol tablets) prescribing information. New York, NY; 2024 Nov.
302. Oceanside Pharmaceuticals. Diclofenac sodium extended-release tablets prescribing information. Bridgewater, NJ; 2024 Nov.
303. Zydus Pharmaceuticals. Diclofenac potassium film-coated tablets prescribing information. Pennington, NJ; 2024 Jul.
317. IBSA Pharma. Flector (diclofenac epolamine) topical patch prescribing information. Parsippany, NJ; 2024 Nov.
318. Haleon US Holdings LLC. Voltaren Arthritis Pain (diclofenac sodium 1%) topical gel drug facts. Warren, NJ; 2024 Mar.
320. Galer BS, Rowbotham M, Perander J et al. Topical diclofenac patch relieves minor sports injury pain: results of a multicenter controlled clinical trial. J Pain Symptom Manage. 2000; 19:287-94. https://pubmed.ncbi.nlm.nih.gov/10799795
321. Anon. Diclofenac gel for osteoarthritis. Med Lett Drugs Ther. 2008; 50:31-2.
324. IBSA Pharma. Licart (diclofenac epolamine) transdermal system prescribing information. Parsippany, NJ; 2024 Nov.
326. Amneal Pharmaceuticals. Diclofenac sodium 1.5% topical solution prescribing information. Bridgewater, NJ; 2024 Jul.
327. Horizon Medicines. Pennsaid (diclofenac sodium) 2% topical solution prescribing information. Deerfield, IL; 2024 Mar.
328. Assertio Therapeutics. Cambia (diclofenac potassium) for oral solution prescribing information. Lake Forest, IL; 2024 Nov.
329. Lipton RB, Grosberg B, Singer RP et al. Efficacy and tolerability of a new powdered formulation of diclofenac potassium for oral solution for the acute treatment of migraine: results from the International Migraine Pain Assessment Clinical Trial (IMPACT). Cephalalgia. 2010; 30:1336-45. https://pubmed.ncbi.nlm.nih.gov/20959428
330. Kolasinski SL, Neogi T, Hochberg MC et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020; 72:220-233. https://pubmed.ncbi.nlm.nih.gov/31908163
331. Assertio Therapeutics. Zipsor (diclofenac potassium) liquid-filled capsules prescribing information. Lake Forest, IL; 2024 Nov.
333. Daniels SE, Baum DR, Clark F et al. Diclofenac potassium liquid-filled soft gelatin capsules for the treatment of postbunionectomy pain. Curr Med Res Opin. 2010; 26:2375-84. https://pubmed.ncbi.nlm.nih.gov/20804444
334. Riff DS, Duckor S, Gottlieb I et al. Diclofenac potassium liquid-filled soft gelatin capsules in the management of patients with postbunionectomy pain: a Phase III, multicenter, randomized, double-blind, placebo-controlled study conducted over 5 days. Clin Ther. 2009; 31:2072-85. https://pubmed.ncbi.nlm.nih.gov/19922878
336. Carwin Pharmaceuticals Assoc. Lofena (diclofenac potassium) film-coated tablets prescribing information. Hazlet, NJ; 2021 Jul.
337. Wadsworth LT, Kent JD, Holt RJ. Efficacy and safety of diclofenac sodium 2% topical solution for osteoarthritis of the knee: a randomized, double-blind, vehicle-controlled, 4 week study. Curr Med Res Opin. 2016;32(2):241-50.
338. Walker C, Essex MN, Li C, Park PW. Celecoxib versus diclofenac for the treatment of ankylosing spondylitis: 12-week randomized study in Norwegian patients. J Int Med Res. 2016 Jun;44(3):483-95.
339. Verkleij SP, Luijsterburg PA, Willemsen SP, Koes BW, Bohnen AM, Bierma-Zeinstra SM. Effectiveness of diclofenac versus paracetamol in knee osteoarthritis: a randomised controlled trial in primary care. Br J Gen Pract. 2015 Aug;65(637):e530-7.
340. Barthel HR, Haselwood D, Longley S 3rd, Gold MS, Altman RD. Randomized controlled trial of diclofenac sodium gel in knee osteoarthritis. Semin Arthritis Rheum. 2009 Dec;39(3):203-12.
341. Altman RD, Dreiser RL, Fisher CL, Chase WF, Dreher DS, Zacher J. Diclofenac sodium gel in patients with primary hand osteoarthritis: a randomized, double-blind, placebo-controlled trial. J Rheumatol. 2009 Sep;36(9):1991-9.
342. Simon LS, Grierson LM, Naseer Z, Bookman AAM, Shainhouse ZJ. Efficacy and safety of topical diclofenac containing dimethyl sulfoxide (DMSO) compared with those of topical placebo, DMSO vehicle and oral diclofenac for knee osteoarthritis. Pain. 2009 Jun;143(3):238-245.
343. Roth SH, Shainhouse JZ. Efficacy and safety of a topical diclofenac solution (pennsaid) in the treatment of primary osteoarthritis of the knee: a randomized, double-blind, vehicle-controlled clinical trial. Arch Intern Med. 2004 Oct 11;164(18):2017-23.
344. Baer PA, Thomas LM, Shainhouse Z. Treatment of osteoarthritis of the knee with a topical diclofenac solution: a randomised controlled, 6-week trial [ISRCTN53366886]. BMC Musculoskelet Disord. 2005 Aug 8;6:44.
345. Tugwell PS, Wells GA, Shainhouse JZ. Equivalence study of a topical diclofenac solution (pennsaid) compared with oral diclofenac in symptomatic treatment of osteoarthritis of the knee: a randomized controlled trial. J Rheumatol. 2004 Oct;31(10):2002-12.
346. Heller B, Tarricone R. Oxaprozin versus diclofenac in NSAID-refractory periarthritis pain of the shoulder. Curr Med Res Opin. 2004 Aug;20(8):1279-90.
347. Liang TH, Hsu PN. Double-blind, randomised, comparative trial of etodolac SR versus diclofenac in the treatment of osteoarthritis of the knee. Curr Med Res Opin. 2003;19(4):336-41.
348. McKenna F, Borenstein D, Wendt H, Wallemark C, Lefkowith JB, Geis GS. Celecoxib versus diclofenac in the management of osteoarthritis of the knee. Scand J Rheumatol. 2001;30(1):11-8.
349. Goei Thè HS, Lund B, Distel MR, Bluhmki E. A double-blind, randomized trial to compare meloxicam 15 mg with diclofenac 100 mg in the treatment of osteoarthritis of the knee. Osteoarthritis Cartilage. 1997 Jul;5(4):283-8.
350. Hosie J, Distel M, Bluhmki E. Meloxicam in osteoarthritis: a 6-month, double-blind comparison with diclofenac sodium. Br J Rheumatol. 1996 Apr;35 Suppl 1:39-43.
351. Gerecz-Simon E, Soper WY, Kean WF, Rooney PJ, Tugwell P, Buchanan WW. A controlled comparison of piroxicam and diclofenac in patients with osteoarthritis. Clin Rheumatol. 1990 Jun;9(2):229-34.
352. Esteller-Martínez V, Paredes-García J, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Analgesic efficacy of diclofenac sodium versus ibuprofen following surgical extraction of impacted lower third molars. Med Oral Patol Oral Cir Bucal. 2004 Nov-Dec;9(5):448-53; 444-8.
353. Baraf HS, Gold MS, Clark MB, Altman RD. Safety and efficacy of topical diclofenac sodium 1% gel in knee osteoarthritis: a randomized controlled trial. Phys Sportsmed. 2010 Jun;38(2):19-28.
354. Lonauer G, Tisscher JR, Lim HG, Bijlsma JW. Double-blind comparison of etodolac and diclofenac in patients with rheumatoid arthritis. Curr Med Res Opin. 1993;13(2):70-7.
355. Grisanti AM, Vaz AA, Samara AM. Comparison of etodolac and diclofenac in osteoarthritis of the knee. Clin Ther. 1992 Nov-Dec;14(6):791-800.
356. Crowley B, Hamill JJ, Lyndon S, McKellican JF, Williams P, Miller AJ. Controlled-release indomethacin and sustained-release diclofenac sodium in the treatment of rheumatoid arthritis: a comparative controlled clinical trial. Curr Med Res Opin. 1990;12(3):143-50.
357. Gostick N, James IG, Khong TK, Roy P, Shepherd PR, Miller AJ. Controlled-release indomethacin and sustained-release diclofenac sodium in the treatment of osteoarthritis: a comparative controlled clinical trial in general practice. Curr Med Res Opin. 1990;12(3):135-42.
358. Derry S, Wiffen PJ, Moore RA. Single dose oral diclofenac for acute postoperative pain in adults. Cochrane Database Syst Rev. 2015 Jul 7;2015(7):CD004768.
359. Moore RA, Derry S. Diclofenac Potassium in Acute Postoperative Pain and Dysmenorrhoea: Results from Comprehensive Clinical Trial Reports. Pain Res Manag. 2018 Jan 17;2018:9493413.
360. Iacovides S, Baker FC, Avidon I. The 24-h progression of menstrual pain in women with primary dysmenorrhea when given diclofenac potassium: a randomized, double-blinded, placebo-controlled crossover study. Arch Gynecol Obstet. 2014 May;289(5):993-1002.
361. Huskisson EC, Scott DL. A clinical comparison of two leading non-steroidal anti-inflammatory drugs. Eur J Rheumatol Inflamm. 1991;11(2):4-7.
999. By the 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023 Jul;71(7):2052-2081. doi: 10.1111/jgs.18372. Epub 2023 May 4. PMID: 37139824.
1223. Ailani J, Burch RC, Robbins MS; Board of Directors of the American Headache Society. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache. 2021 Jul;61(7):1021-1039.
2001. Fraenkel L, Bathon J, England B, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res. 2021;73(7):924-939.
2003. Ringold S, Angeles-Han ST, Beukelman T et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Care Res (Hoboken). 2019; 71:717-734.
2006. FitzGerald JD, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles AM, Gelber AC, Harrold LR, Khanna D, King C, Levy G, Libbey C, Mount D, Pillinger MH, Rosenthal A, Singh JA, Sims JE, Smith BJ, Wenger NS, Bae SS, Danve A, Khanna PP, Kim SC, Lenert A, Poon S, Qasim A, Sehra ST, Sharma TSK, Toprover M, Turgunbaev M, Zeng L, Zhang MA, Turner AS, Neogi T. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res (Hoboken). 2020 Jun;72(6):744-760.
2008. Ward MM, Deodhar A, Gensler LS et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019; 71:1599-1613.
2009. Onel KB, Horton DB, Lovell DJ, Shenoi S, Cuello CA, Angeles-Han ST, Becker ML, Cron RQ, Feldman BM, Ferguson PJ, Gewanter H, Guzman J, Kimura Y, Lee T, Murphy K, Nigrovic PA, Ombrello MJ, Rabinovich CE, Tesher M, Twilt M, Klein-Gitelman M, Barbar-Smiley F, Cooper AM, Edelheit B, Gillispie-Taylor M, Hays K, Mannion ML, Peterson R, Flanagan E, Saad N, Sullivan N, Szymanski AM, Trachtman R, Turgunbaev M, Veiga K, Turner AS, Reston JT. 2021 American College of Rheumatology Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Oligoarthritis, Temporomandibular Joint Arthritis, and Systemic Juvenile Idiopathic Arthritis. Arthritis Rheumatol. 2022 Apr;74(4):553-569.
2010. Qaseem A, McLean RM, O'Gurek D, Batur P, Lin K, Kansagara DL; Clinical Guidelines Committee of the American College of Physicians; Commission on Health of the Public and Science of the American Academy of Family Physicians; Cooney TG, Forciea MA, Crandall CJ, Fitterman N, Hicks LA, Horwitch C, Maroto M, McLean RM, Mustafa RA, Tufte J, Vijan S, Williams JW Jr. Nonpharmacologic and Pharmacologic Management of Acute Pain From Non-Low Back, Musculoskeletal Injuries in Adults: A Clinical Guideline From the American College of Physicians and American Academy of Family Physicians. Ann Intern Med. 2020 Nov 3;173(9):739-748.
2012. ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. Obstet Gynecol. 2018;132(6):e249-e258.
2013. Chou R, Gordon D, de Leon-Casaola O, et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
2015. Ferries-Rowe E, Corey E, Archer J. Primary dysmenorrhea. Diagnosis and Therapy. Obstet Gynecol. 2020;136(5):1047-1058.
Related/similar drugs
Frequently asked questions
- Can I take ibuprofen with blood pressure medications?
- Which painkiller should you use?
- Can you Double up on Pain Medications? Safe Painkiller Combinations
- Why is diclofenac prescription only but ibuprofen is OTC?
- Can NSAIDs be used to treat a COVID-19 fever?
- Does diclofenac contain narcotics or affect a drug test?
More about diclofenac
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (701)
- Drug images
- Latest FDA alerts (11)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
- En español
Patient resources
- Diclofenac drug information
- Diclofenac (Intravenous) (Advanced Reading)
- Diclofenac (Oral) (Advanced Reading)
Professional resources
- Diclofenac prescribing information
- Diclofenac Capsule (FDA)
- Diclofenac Delayed Release Tablets (FDA)
- Diclofenac Extended Release Tablets 100mg (FDA)
- Diclofenac Oral Solution (FDA)
Other brands
Voltaren, Cataflam, Cambia, Voltaren-XR, ... +3 more