Azithromycin Dosage
Medically reviewed by Drugs.com. Last updated on May 5, 2025.
Applies to the following strengths: 500 mg; 250 mg; 1 g; 600 mg; 100 mg/5 mL; 200 mg/5 mL; 2 g; 2.5 g
Usual Adult Dose for:
- Legionella Pneumonia
- Mycoplasma Pneumonia
- Pneumonia
- Tonsillitis/Pharyngitis
- Sinusitis
- Skin and Structure Infection
- Bartonellosis
- Gonococcal Infection - Uncomplicated
- Nongonococcal Urethritis
- Chlamydia Infection
- Cervicitis
- Chancroid
- Pelvic Inflammatory Disease
- Bronchitis
- Mycobacterium avium-intracellulare - Prophylaxis
- Mycobacterium avium-intracellulare - Treatment
- Mycobacterium kansasii
- Granuloma Inguinale
- Pertussis Prophylaxis
- Pertussis
- Lyme Disease - Erythema Chronicum Migrans
- Babesiosis
- Bacterial Endocarditis Prophylaxis
- Campylobacter Gastroenteritis
- Shigellosis
- Bacterial Infection
- Syphilis - Early
Usual Pediatric Dose for:
- Otitis Media
- Legionella Pneumonia
- Mycoplasma Pneumonia
- Pneumonia
- Tonsillitis/Pharyngitis
- Sinusitis
- Pelvic Inflammatory Disease
- Skin and Structure Infection
- Bartonellosis
- Gonococcal Infection - Uncomplicated
- Chlamydia Infection
- Mycobacterium avium-intracellulare - Prophylaxis
- Mycobacterium avium-intracellulare - Treatment
- Pertussis Prophylaxis
- Pertussis
- Lyme Disease - Erythema Chronicum Migrans
- Babesiosis
- Bacterial Endocarditis Prophylaxis
- Campylobacter Gastroenteritis
- Shigellosis
- Syphilis - Early
Additional dosage information:
Usual Adult Dose for Legionella Pneumonia
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Patients appropriate for oral therapy: 500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, significant underlying health problems that may compromise ability to respond to illness (including immunodeficiency or functional asplenia), elderly, debilitated, or require hospitalization.
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
Uses:
- IV: For the treatment of community-acquired pneumonia due to Chlamydophila pneumoniae, Haemophilus influenzae, Legionella pneumophila, Moraxella catarrhalis, Mycoplasma pneumoniae, Staphylococcus aureus, or Streptococcus pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
Usual Adult Dose for Mycoplasma Pneumonia
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Patients appropriate for oral therapy: 500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, significant underlying health problems that may compromise ability to respond to illness (including immunodeficiency or functional asplenia), elderly, debilitated, or require hospitalization.
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
Uses:
- IV: For the treatment of community-acquired pneumonia due to Chlamydophila pneumoniae, Haemophilus influenzae, Legionella pneumophila, Moraxella catarrhalis, Mycoplasma pneumoniae, Staphylococcus aureus, or Streptococcus pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
Usual Adult Dose for Pneumonia
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Patients appropriate for oral therapy: 500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, significant underlying health problems that may compromise ability to respond to illness (including immunodeficiency or functional asplenia), elderly, debilitated, or require hospitalization.
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
Uses:
- IV: For the treatment of community-acquired pneumonia due to Chlamydophila pneumoniae, Haemophilus influenzae, Legionella pneumophila, Moraxella catarrhalis, Mycoplasma pneumoniae, Staphylococcus aureus, or Streptococcus pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
Usual Adult Dose for Tonsillitis/Pharyngitis
500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Use: For the treatment of mild to moderate pharyngitis/tonsillitis due to S pyogenes as an alternative to first-line therapy in patients who cannot use first-line therapy
Infectious Diseases Society of America (IDSA) Recommendations: 12 mg/kg orally once a day for 5 days
- Maximum dose: 500 mg/dose
Comments:
- Recommended for the treatment of group A streptococcal pharyngitis in patients with penicillin allergy
- Resistance of group A Streptococcus to this drug is well-known and varies geographically and temporally.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Sinusitis
500 mg orally once a day for 3 days
Use: For the treatment of mild to moderate acute bacterial sinusitis due to H influenzae, M catarrhalis, or S pneumoniae
Usual Adult Dose for Skin and Structure Infection
500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Use: For the treatment of mild to moderate uncomplicated skin and skin structure infections due to S aureus, S pyogenes, or S agalactiae
IDSA Recommendations:
- Cat scratch disease:
- Weight less than 45 kg: 10 mg/kg orally on day 1, then 5 mg/kg orally once a day for 4 additional days
- Weight at least 45 kg: 500 mg orally on day 1, then 250 mg orally once a day for 4 additional days
The Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV (the Panel) Recommendations:
- Bartonella infections: 500 mg orally once a day for at least 3 months
Comments:
- Recommended for cat scratch disease
- Recommended as an alternative regimen for Bartonella infections (not for endocarditis or CNS infections) in patients with HIV
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Bartonellosis
500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Use: For the treatment of mild to moderate uncomplicated skin and skin structure infections due to S aureus, S pyogenes, or S agalactiae
IDSA Recommendations:
- Cat scratch disease:
- Weight less than 45 kg: 10 mg/kg orally on day 1, then 5 mg/kg orally once a day for 4 additional days
- Weight at least 45 kg: 500 mg orally on day 1, then 250 mg orally once a day for 4 additional days
The Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV (the Panel) Recommendations:
- Bartonella infections: 500 mg orally once a day for at least 3 months
Comments:
- Recommended for cat scratch disease
- Recommended as an alternative regimen for Bartonella infections (not for endocarditis or CNS infections) in patients with HIV
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Gonococcal Infection - Uncomplicated
2 g orally as a single dose
Comments:
- No oral formulation (at the recommended dose) should be relied upon to treat syphilis.
- All patients with sexually transmitted urethritis or cervicitis should have a serologic test for syphilis and appropriate testing/cultures for gonorrhea at time of diagnosis; if infection is confirmed, appropriate antibacterial therapy and follow-up tests for these diseases should be started.
Use: For the treatment of mild to moderate urethritis and cervicitis due to Neisseria gonorrhoeae
US CDC Recommendations: 2 g orally as a single dose
Comments:
- With gentamicin, recommended as an alternative regimen for uncomplicated gonococcal infections of the cervix, urethra, or rectum if ceftriaxone is not available
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Nongonococcal Urethritis
1 g orally as a single dose
Comments:
- Antibacterial agents used in high doses for short periods of time to treat nongonococcal urethritis may mask or delay symptoms of incubating syphilis or gonorrhea.
- No oral formulation (at the recommended dose) should be relied upon to treat syphilis; in addition, the oral suspension in the single dose packet (1 g) should not be relied upon to treat gonorrhea.
- All patients with sexually transmitted urethritis or cervicitis should have a serologic test for syphilis and appropriate testing/cultures for gonorrhea at time of diagnosis; if infection is confirmed, appropriate antibacterial therapy and follow-up tests for these diseases should be started.
Use: For the treatment of mild to moderate urethritis and cervicitis due to Chlamydia trachomatis
US CDC Recommendations:
- Cervicitis and chlamydial infection: 1 g orally as a single dose
- Lymphogranuloma venereum: 1 g orally once a week for 3 weeks
- M genitalium cervicitis or urethritis: 1 g orally as initial dose, followed by 500 mg orally once a day for 3 additional days
- Nongonococcal urethritis: 1 g orally as a single dose OR 500 mg orally as a single dose on the first day, followed by 250 mg orally once a day for 4 days
Comments:
- Recommended as an alternative regimen for cervicitis
- Concurrent therapy for gonococcal infection should be considered if the patient is at risk for gonorrhea or lives in an area with high gonorrhea prevalence.
- Recommended as an alternative regimen for chlamydial infection among adults; recommended regimen for chlamydial infection during pregnancy
- Recommended as an alternative regimen for lymphogranuloma venereum due to C trachomatis
- This regimen has not been validated; a test of cure with C trachomatis nucleic acid amplification test 4 weeks after therapy completion can be considered.
- Recommended regimen after doxycycline if M genitalium resistance testing is available and M genitalium is macrolide sensitive
- Recommended as alternative regimens for nongonococcal urethritis
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Chlamydia Infection
1 g orally as a single dose
Comments:
- Antibacterial agents used in high doses for short periods of time to treat nongonococcal urethritis may mask or delay symptoms of incubating syphilis or gonorrhea.
- No oral formulation (at the recommended dose) should be relied upon to treat syphilis; in addition, the oral suspension in the single dose packet (1 g) should not be relied upon to treat gonorrhea.
- All patients with sexually transmitted urethritis or cervicitis should have a serologic test for syphilis and appropriate testing/cultures for gonorrhea at time of diagnosis; if infection is confirmed, appropriate antibacterial therapy and follow-up tests for these diseases should be started.
Use: For the treatment of mild to moderate urethritis and cervicitis due to Chlamydia trachomatis
US CDC Recommendations:
- Cervicitis and chlamydial infection: 1 g orally as a single dose
- Lymphogranuloma venereum: 1 g orally once a week for 3 weeks
- M genitalium cervicitis or urethritis: 1 g orally as initial dose, followed by 500 mg orally once a day for 3 additional days
- Nongonococcal urethritis: 1 g orally as a single dose OR 500 mg orally as a single dose on the first day, followed by 250 mg orally once a day for 4 days
Comments:
- Recommended as an alternative regimen for cervicitis
- Concurrent therapy for gonococcal infection should be considered if the patient is at risk for gonorrhea or lives in an area with high gonorrhea prevalence.
- Recommended as an alternative regimen for chlamydial infection among adults; recommended regimen for chlamydial infection during pregnancy
- Recommended as an alternative regimen for lymphogranuloma venereum due to C trachomatis
- This regimen has not been validated; a test of cure with C trachomatis nucleic acid amplification test 4 weeks after therapy completion can be considered.
- Recommended regimen after doxycycline if M genitalium resistance testing is available and M genitalium is macrolide sensitive
- Recommended as alternative regimens for nongonococcal urethritis
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Cervicitis
1 g orally as a single dose
Comments:
- Antibacterial agents used in high doses for short periods of time to treat nongonococcal urethritis may mask or delay symptoms of incubating syphilis or gonorrhea.
- No oral formulation (at the recommended dose) should be relied upon to treat syphilis; in addition, the oral suspension in the single dose packet (1 g) should not be relied upon to treat gonorrhea.
- All patients with sexually transmitted urethritis or cervicitis should have a serologic test for syphilis and appropriate testing/cultures for gonorrhea at time of diagnosis; if infection is confirmed, appropriate antibacterial therapy and follow-up tests for these diseases should be started.
Use: For the treatment of mild to moderate urethritis and cervicitis due to Chlamydia trachomatis
US CDC Recommendations:
- Cervicitis and chlamydial infection: 1 g orally as a single dose
- Lymphogranuloma venereum: 1 g orally once a week for 3 weeks
- M genitalium cervicitis or urethritis: 1 g orally as initial dose, followed by 500 mg orally once a day for 3 additional days
- Nongonococcal urethritis: 1 g orally as a single dose OR 500 mg orally as a single dose on the first day, followed by 250 mg orally once a day for 4 days
Comments:
- Recommended as an alternative regimen for cervicitis
- Concurrent therapy for gonococcal infection should be considered if the patient is at risk for gonorrhea or lives in an area with high gonorrhea prevalence.
- Recommended as an alternative regimen for chlamydial infection among adults; recommended regimen for chlamydial infection during pregnancy
- Recommended as an alternative regimen for lymphogranuloma venereum due to C trachomatis
- This regimen has not been validated; a test of cure with C trachomatis nucleic acid amplification test 4 weeks after therapy completion can be considered.
- Recommended regimen after doxycycline if M genitalium resistance testing is available and M genitalium is macrolide sensitive
- Recommended as alternative regimens for nongonococcal urethritis
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Chancroid
1 g orally as a single dose
Comments:
- Due to the low number of women included in clinical trials, the efficacy of this drug in the treatment of chancroid in female patients has not been established.
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Use: For the treatment of genital ulcer disease in men due to Haemophilus ducreyi (chancroid)
Usual Adult Dose for Pelvic Inflammatory Disease
IV: 500 mg IV once a day for 1 or 2 days
Oral: After IV therapy, 250 mg orally once a day to complete a 7-day course of therapy
Comments:
- Antimicrobial drugs with anaerobic activity should be used concurrently if anaerobic microorganisms are suspected of contributing to the infection.
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
Use: For the treatment of pelvic inflammatory disease due to C trachomatis, N gonorrhoeae, or M hominis in patients who require initial IV therapy
Usual Adult Dose for Bronchitis
For 3-day regimen: 500 mg orally once a day for 3 days
For 5-day regimen: 500 mg orally as a single dose on day 1, followed by 250 mg orally once a day on days 2 through 5
Use: For the treatment of mild to moderate acute bacterial exacerbations of chronic bronchitis due to H influenzae, M catarrhalis, or S pneumoniae
Usual Adult Dose for Mycobacterium avium-intracellulare - Prophylaxis
1200 mg orally once a week
Use: Alone or in combination with rifabutin (at its approved dose), for the prevention of disseminated Mycobacterium avium complex (MAC) disease in patients with advanced HIV infection
The Panel Recommendations:
- Primary prophylaxis: 1200 mg orally once a week OR 600 mg orally twice a week
- Chronic maintenance therapy: 500 to 600 mg orally once a day
Comments:
- Recommended as preferred regimen for preventing the first episode of disseminated MAC disease (primary prophylaxis) in patients not on fully suppressive antiretroviral therapy (ART) and CD4 count less than 50 cells/mm3 after ruling out disseminated MAC disease based on clinical assessment
- Primary prophylaxis may be discontinued with the initiation of effective ART.
- With ethambutol, recommended as a preferred regimen for chronic maintenance therapy (secondary prophylaxis) of MAC disease when drug interactions/intolerance preclude use of clarithromycin
- Chronic maintenance therapy may be discontinued after completion of at least 12 months of therapy, no signs/symptoms of MAC disease, and CD4 count greater than 100 cells/mm3 sustained (more than 6 months) in response to ART; secondary prophylaxis should be restarted if CD4 drops below 100 cells/mm3.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Mycobacterium avium-intracellulare - Treatment
600 mg orally once a day
Comments:
- Other antimycobacterial drugs with in vitro activity against MAC may be added to this regimen at the health care provider's discretion.
Use: In combination with ethambutol, for the treatment of disseminated MAC infections in patients with advanced HIV infection
American Thoracic Society (ATS), European Respiratory Society (ERS), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and IDSA Recommendations:
- MAC:
- Cavitary and refractory: 250 to 500 mg orally once a day
- Nodular-bronchiectatic: 500 mg orally 3 times a week
- M kansasii: 250 to 500 mg orally once a day OR 500 mg orally 3 times a week
- M xenopi and M abscessus: 250 to 500 mg orally once a day
The Panel Recommendations: 500 to 600 mg orally once a day
Comments:
- ATS, ERS, ESCMID, and IDSA: In combination with 2 or more drugs, recommended as part of preferred regimens for MAC, M kansasii, M xenopi, and M abscessus pulmonary disease
- The Panel: With ethambutol, recommended as a preferred regimen to treat disseminated MAC disease when drug interactions/intolerance preclude use of clarithromycin
- Testing of drug susceptibility is recommended.
- At least 2 drugs are recommended as initial therapy to prevent/delay emergence of resistance.
- Chronic suppressive therapy (secondary prophylaxis) is recommended after initial therapy.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Mycobacterium kansasii
600 mg orally once a day
Comments:
- Other antimycobacterial drugs with in vitro activity against MAC may be added to this regimen at the health care provider's discretion.
Use: In combination with ethambutol, for the treatment of disseminated MAC infections in patients with advanced HIV infection
American Thoracic Society (ATS), European Respiratory Society (ERS), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and IDSA Recommendations:
- MAC:
- Cavitary and refractory: 250 to 500 mg orally once a day
- Nodular-bronchiectatic: 500 mg orally 3 times a week
- M kansasii: 250 to 500 mg orally once a day OR 500 mg orally 3 times a week
- M xenopi and M abscessus: 250 to 500 mg orally once a day
The Panel Recommendations: 500 to 600 mg orally once a day
Comments:
- ATS, ERS, ESCMID, and IDSA: In combination with 2 or more drugs, recommended as part of preferred regimens for MAC, M kansasii, M xenopi, and M abscessus pulmonary disease
- The Panel: With ethambutol, recommended as a preferred regimen to treat disseminated MAC disease when drug interactions/intolerance preclude use of clarithromycin
- Testing of drug susceptibility is recommended.
- At least 2 drugs are recommended as initial therapy to prevent/delay emergence of resistance.
- Chronic suppressive therapy (secondary prophylaxis) is recommended after initial therapy.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Granuloma Inguinale
US CDC Recommendations: 1 g orally once a week OR 500 mg orally once a day for greater than 3 weeks and until all lesions have completely healed
Comments:
- Recommended regimen for granuloma inguinale (donovanosis) due to Klebsiella granulomatis
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Pertussis Prophylaxis
American Society for Blood and Marrow Transplantation (ASBMT) Recommendations:
- Immunization against pertussis: 250 mg orally once a day
- Postexposure prophylaxis: 500 mg orally for 1 day, then 250 mg orally once a day for 4 days
Comments:
- Recommended as an alternative for immunization against pertussis for hematopoietic cell transplantation (HCT) recipients with an incomplete vaccination series
- Recommended as the first choice for postexposure prophylaxis for HCT recipients, regardless of vaccination status
- Patients should receive the acellular pertussis vaccine after HCT.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Pertussis
American Society for Blood and Marrow Transplantation (ASBMT) Recommendations:
- Immunization against pertussis: 250 mg orally once a day
- Postexposure prophylaxis: 500 mg orally for 1 day, then 250 mg orally once a day for 4 days
Comments:
- Recommended as an alternative for immunization against pertussis for hematopoietic cell transplantation (HCT) recipients with an incomplete vaccination series
- Recommended as the first choice for postexposure prophylaxis for HCT recipients, regardless of vaccination status
- Patients should receive the acellular pertussis vaccine after HCT.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Lyme Disease - Erythema Chronicum Migrans
IDSA, American Academy of Neurology (AAN), and American College of Rheumatology (ACR) Recommendations: 500 mg orally once a day
Duration of therapy: 7 days (range: 5 to 10 days)
Comments:
- Recommended as an alternative agent for solitary and multiple erythema migrans
- Due to concerns for lower efficacy, macrolide antibiotics (including this drug) are considered second-line agents, and should be reserved for patients in whom other antibiotic classes are contraindicated.
- This drug has not been adequately studied for manifestations of Lyme disease other than erythema migrans.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Babesiosis
IDSA Recommendations:
Ambulatory patients (mild to moderate disease): 500 mg orally on day 1, followed by 250 mg orally every 24 hours
Duration of therapy: 7 to 10 days in immunocompetent patients; often extended in immunocompromised patients
Hospitalized patients:
- Acute severe disease: 500 mg IV every 24 hours until symptoms abate, then should switch to all oral therapy (step-down therapy)
- For immunocompromised patients: 1000 mg orally (with other antibiotics) OR 1000 mg IV once followed by 500 mg IV once a day
- Step-down therapy (switch to oral therapy): 250 to 500 mg orally every 24 hours
- For immunocompromised patients: 500 to 1000 mg orally every 24 hours should be considered
- For immunocompromised patients: At least 6 consecutive weeks (including 2 final weeks with no parasites detected on peripheral blood smear)
Refractory infections: 500 to 1000 mg orally once a day should be considered
Comments:
- With atovaquone, recommended as preferred treatment regimens for babesiosis patients
- With atovaquone plus clindamycin (with or without quinine), recommended for refractory Babesia infections (limited evidence of efficacy)
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Bacterial Endocarditis Prophylaxis
American Heart Association (AHA) Recommendations: 500 mg orally as a single dose 30 to 60 minutes before procedure
Comments:
- Recommended regimen for a dental procedure in patients allergic to penicillins or ampicillin
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Campylobacter Gastroenteritis
The Panel Recommendations: 500 mg orally once a day for 5 days
Comments:
- Recommended as an alternative regimen (depending on susceptibility results) to treat gastroenteritis due to Shigella infection
- Recommended as a preferred regimen to treat mild to moderate gastroenteritis due to Campylobacter infection
- This drug is not recommended for Shigella or Campylobacter bacteremia.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Shigellosis
The Panel Recommendations: 500 mg orally once a day for 5 days
Comments:
- Recommended as an alternative regimen (depending on susceptibility results) to treat gastroenteritis due to Shigella infection
- Recommended as a preferred regimen to treat mild to moderate gastroenteritis due to Campylobacter infection
- This drug is not recommended for Shigella or Campylobacter bacteremia.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Bacterial Infection
ASBMT Recommendations: 250 mg orally once a day
Comments:
- Recommended as an alternative for prevention of bacterial infections during the first 100 days after HCT for patients with anticipated neutropenic periods of at least 7 days
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Syphilis - Early
The Panel Recommendations: 2 g orally as a single dose
Comments:
- Recommended as an alternative regimen for penicillin-allergic patients for the treatment of early stage syphilis (primary, secondary, and early latent syphilis)
- Chromosomal mutations associated with resistance and treatment failures have been reported with this drug, most commonly in men who have sex with men (MSM); this drug should be used with caution and only when penicillin, doxycycline, or ceftriaxone therapy is not feasible.
- This drug is not recommended for MSM or pregnant patients.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Otitis Media
6 months or older:
- For 1-day regimen: 30 mg/kg orally as a single dose
- Maximum dose: 1500 mg/dose
- For 3-day regimen: 10 mg/kg orally once a day for 3 days
- Maximum dose: 500 mg/dose
- For 5-day regimen: 10 mg/kg orally as a single dose on day 1, followed by 5 mg/kg orally once a day on days 2 through 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 through 5)
Comments:
- The safety of a redosing this drug in a patient who vomits after receiving 30 mg/kg as a single dose has not been established.
Use: For the treatment of mild to moderate acute otitis media due to H influenza, M catarrhalis, or S pneumoniae
Usual Pediatric Dose for Legionella Pneumonia
6 months or older: 10 mg/kg orally as a single dose on day 1, followed by 5 mg/kg orally once a day on days 2 through 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 through 5)
16 years or older:
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, require hospitalization, elderly, debilitated, or significant underlying health problem that may compromise ability to respond to illness (including immunodeficiency or functional asplenia).
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
- Efficacy of the 3-day or 1-day oral regimen has not been established in pediatric patients with community-acquired pneumonia.
Uses:
- IV: For the treatment of community-acquired pneumonia due to C pneumoniae, H influenzae, L pneumophila, M catarrhalis, M pneumoniae, S aureus, or S pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
IDSA and Pediatric Infectious Diseases Society (PIDS) Recommendations for Infants and Children Older Than 3 Months:
Inpatient (all ages) and for specific pathogens:
- IV: 10 mg/kg IV on days 1 and 2 of therapy, then should transition to oral therapy if possible
- Oral (step-down therapy or mild infection): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
Outpatient:
- Younger than 5 years (preschool): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- At least 5 years of age: 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 to 5)
Comments:
- Recommended as preferred therapy for community-acquired pneumonia due to M pneumoniae, C trachomatis, or C pneumoniae
- Recommended as empiric therapy for presumed atypical pneumonia in outpatient and inpatient settings
- Beta-lactam antibiotics may be added for inpatients with presumed atypical pneumonia if diagnosis is in doubt.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Mycoplasma Pneumonia
6 months or older: 10 mg/kg orally as a single dose on day 1, followed by 5 mg/kg orally once a day on days 2 through 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 through 5)
16 years or older:
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, require hospitalization, elderly, debilitated, or significant underlying health problem that may compromise ability to respond to illness (including immunodeficiency or functional asplenia).
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
- Efficacy of the 3-day or 1-day oral regimen has not been established in pediatric patients with community-acquired pneumonia.
Uses:
- IV: For the treatment of community-acquired pneumonia due to C pneumoniae, H influenzae, L pneumophila, M catarrhalis, M pneumoniae, S aureus, or S pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
IDSA and Pediatric Infectious Diseases Society (PIDS) Recommendations for Infants and Children Older Than 3 Months:
Inpatient (all ages) and for specific pathogens:
- IV: 10 mg/kg IV on days 1 and 2 of therapy, then should transition to oral therapy if possible
- Oral (step-down therapy or mild infection): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
Outpatient:
- Younger than 5 years (preschool): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- At least 5 years of age: 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 to 5)
Comments:
- Recommended as preferred therapy for community-acquired pneumonia due to M pneumoniae, C trachomatis, or C pneumoniae
- Recommended as empiric therapy for presumed atypical pneumonia in outpatient and inpatient settings
- Beta-lactam antibiotics may be added for inpatients with presumed atypical pneumonia if diagnosis is in doubt.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Pneumonia
6 months or older: 10 mg/kg orally as a single dose on day 1, followed by 5 mg/kg orally once a day on days 2 through 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 through 5)
16 years or older:
Patients who require initial IV therapy:
- IV: 500 mg IV once a day for at least 2 days
- Oral: After IV therapy, 500 mg orally once a day to complete a 7- to 10-day course of therapy
Comments:
- Limitations of Use: Oral formulations of this drug should not be used in patients with pneumonia who are considered inappropriate for oral therapy due to moderate to severe illness or risk factors such as: cystic fibrosis, nosocomial infections, known/suspected bacteremia, require hospitalization, elderly, debilitated, or significant underlying health problem that may compromise ability to respond to illness (including immunodeficiency or functional asplenia).
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
- Efficacy of the 3-day or 1-day oral regimen has not been established in pediatric patients with community-acquired pneumonia.
Uses:
- IV: For the treatment of community-acquired pneumonia due to C pneumoniae, H influenzae, L pneumophila, M catarrhalis, M pneumoniae, S aureus, or S pneumoniae in patients who require initial IV therapy
- Oral: For the treatment of mild to moderate community-acquired pneumonia due to C pneumoniae, H influenzae, M pneumoniae, or S pneumoniae in patients appropriate for oral therapy
IDSA and Pediatric Infectious Diseases Society (PIDS) Recommendations for Infants and Children Older Than 3 Months:
Inpatient (all ages) and for specific pathogens:
- IV: 10 mg/kg IV on days 1 and 2 of therapy, then should transition to oral therapy if possible
- Oral (step-down therapy or mild infection): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
Outpatient:
- Younger than 5 years (preschool): 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- At least 5 years of age: 10 mg/kg orally on day 1, followed by 5 mg/kg orally once a day on days 2 to 5
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (days 2 to 5)
Comments:
- Recommended as preferred therapy for community-acquired pneumonia due to M pneumoniae, C trachomatis, or C pneumoniae
- Recommended as empiric therapy for presumed atypical pneumonia in outpatient and inpatient settings
- Beta-lactam antibiotics may be added for inpatients with presumed atypical pneumonia if diagnosis is in doubt.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Tonsillitis/Pharyngitis
2 years or older: 12 mg/kg orally once a day for 5 days
- Maximum dose: 500 mg/dose
Use: For the treatment of mild to moderate pharyngitis/tonsillitis due to S pyogenes as an alternative to first-line therapy in patients who cannot use first-line therapy
Usual Pediatric Dose for Sinusitis
6 months or older: 10 mg/kg once a day for 3 days
- Maximum dose: 500 mg/dose
Comments:
- Efficacy of the 1-day or 5-day oral regimen has not been established in pediatric patients with acute bacterial sinusitis.
Use: Treatment of mild to moderate acute bacterial sinusitis due to H influenza, M catarrhalis, or S pneumoniae
Usual Pediatric Dose for Pelvic Inflammatory Disease
16 years or older:
- IV: 500 mg IV once a day for 1 or 2 days
- Oral: After IV therapy, 250 mg orally once a day to complete a 7-day course of therapy
Comments:
- Antimicrobial drugs with anaerobic activity should be used concurrently if anaerobic microorganisms are suspected of contributing to the infection.
- The IV formulation should be followed by the oral formulation as required.
- Patients should be switched from IV to oral therapy at the physician's discretion and according to clinical response.
Use: For the treatment of pelvic inflammatory disease due to C trachomatis, N gonorrhoeae, or M hominis in patients who require initial IV therapy
Usual Pediatric Dose for Skin and Structure Infection
IDSA Recommendations:
- Cat scratch disease:
- Weight less than 45 kg: 10 mg/kg orally on day 1, then 5 mg/kg orally once a day for 4 additional days
- Weight at least 45 kg: 500 mg orally on day 1, then 250 mg orally once a day for 4 additional days
The Panel Recommendations for Adolescents:
- Bartonella infections: 500 mg orally once a day for at least 3 months
Comments:
- Recommended for cat scratch disease
- Recommended as an alternative regimen for Bartonella infections (not for endocarditis or CNS infections) in adolescents with HIV
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Bartonellosis
IDSA Recommendations:
- Cat scratch disease:
- Weight less than 45 kg: 10 mg/kg orally on day 1, then 5 mg/kg orally once a day for 4 additional days
- Weight at least 45 kg: 500 mg orally on day 1, then 250 mg orally once a day for 4 additional days
The Panel Recommendations for Adolescents:
- Bartonella infections: 500 mg orally once a day for at least 3 months
Comments:
- Recommended for cat scratch disease
- Recommended as an alternative regimen for Bartonella infections (not for endocarditis or CNS infections) in adolescents with HIV
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Gonococcal Infection - Uncomplicated
US CDC Recommendations for Adolescents: 2 g orally as a single dose
Comments:
- With gentamicin, recommended as an alternative regimen for uncomplicated gonococcal infections of the cervix, urethra, or rectum if ceftriaxone is not available
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Chlamydia Infection
US CDC Recommendations:
- Infants 1 to 3 months:
- Oral suspension: 20 mg/kg orally once a day for 3 days
- Children younger than 8 years weighing at least 45 kg and children 8 years or older: 1 g orally as a single dose
- Adolescents: 1 g orally as a single dose
Comments:
- Recommended as an alternative regimen for chlamydial pneumonia among infants
- Recommended regimen for chlamydial infection among children
- Limited data available regarding efficacy and optimal dose for treating chlamydial infection among infants and children weighing less than 45 kg.
- Recommended as an alternative regimen for chlamydial infection among adolescents
- The patient's sexual partner(s) should also be evaluated/treated.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Mycobacterium avium-intracellulare - Prophylaxis
The Panel on Opportunistic Infections in HIV-Exposed and HIV-Infected Children Recommendations:
Primary prophylaxis:
- First choice: 20 mg/kg orally once a week
- Maximum dose: 1200 mg/dose
- Alternative: 5 mg/kg orally once a day
- Maximum dose: 250 mg/dose
Secondary prophylaxis: 5 mg/kg orally once a day
- Maximum dose: 250 mg/dose
The Panel Recommendations for Adolescents:
- Primary prophylaxis: 1200 mg orally once a week OR 600 mg orally twice a week
- Chronic maintenance therapy: 500 to 600 mg orally once a day
Comments:
- Children: Recommended as a first choice and an alternative regimen for primary prophylaxis of MAC disease in patients with advanced immunosuppression (younger than 1 year with CD4 count less than 750 cells/mm3; 1 to less than 2 years with CD4 count less than 500 cells/mm3; 2 to less than 6 years with CD4 count less than 75 cells/mm3; at least 6 years with CD4 count less than 50 cells/mm3)
- Primary prophylaxis should not be discontinued in children younger than 2 years.
- After at least 6 months of ART, primary prophylaxis may be discontinued if CD4 count is greater than 200 and 100 cells/mm3 for more than 3 consecutive months in children 2 to less than 6 years and children at least 6 years, respectively; if CD4 count drops below 200 and 100 cells/mm3 in the respective age ranges, primary prophylaxis should be restarted.
- Children: With ethambutol, recommended as an alternative regimen for secondary prophylaxis (chronic suppressive therapy) of MAC disease in patients with prior disease
- After at least 6 months of ART, at least 12 months of MAC therapy, and asymptomatic for signs/symptoms of MAC, secondary prophylaxis may be discontinued if CD4 count is greater than 200 and 100 cells/mm3 for at least 6 consecutive months in children 2 to less than 6 years and children at least 6 years, respectively; if CD4 count drops below 200 and 100 cells/mm3 in the respective age ranges, secondary prophylaxis should be restarted.
- Adolescents: Recommended as a preferred regimen for preventing the first episode of disseminated MAC disease (primary prophylaxis) in patients not on fully suppressive ART and CD4 count less than 50 cells/mm3 after ruling out disseminated MAC disease based on clinical assessment
- Primary prophylaxis may be discontinued with the initiation of effective ART.
- Adolescents: With ethambutol, recommended as a preferred regimen for chronic maintenance therapy (secondary prophylaxis) of MAC disease when drug interactions/intolerance preclude use of clarithromycin
- Chronic maintenance therapy may be discontinued after completion of at least 12 months of therapy, no signs/symptoms of MAC disease, and CD4 count greater than 100 cells/mm3 sustained (more than 6 months) in response to ART; secondary prophylaxis should be restarted if CD4 drops below 100 cells/mm3.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Mycobacterium avium-intracellulare - Treatment
The Panel on Opportunistic Infections in HIV-Exposed and HIV-Infected Children Recommendations: 10 to 12 mg/kg orally once a day for at least 12 months
- Maximum dose: 500 mg/dose
The Panel Recommendations for Adolescents: 500 to 600 mg orally once a day
Comments:
- Children: With ethambutol, recommended as an alternative initial regimen for the treatment of MAC disease if intolerant to clarithromycin
- Adolescents: With ethambutol, recommended as a preferred regimen to treat disseminated MAC disease when drug interactions/intolerance preclude use of clarithromycin
- Testing of drug susceptibility is recommended.
- At least 2 drugs are recommended as initial therapy to prevent/delay emergence of resistance.
- Chronic suppressive therapy (secondary prophylaxis) is recommended after initial therapy.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Pertussis Prophylaxis
ASBMT Recommendations:
- Immunization against pertussis: 5 mg/kg orally once a day
- Maximum dose: 250 mg/dose
- Postexposure prophylaxis: 10 mg/kg orally as a loading dose, then 5 mg/kg orally once a day for 4 days
- Maximum dose: 500 mg/dose (loading dose); 250 mg/dose (following doses)
Comments:
- Recommended as an alternative for immunization against pertussis for HCT recipients with an incomplete vaccination series
- Recommended as the first choice for postexposure prophylaxis for HCT recipients, regardless of vaccination status
- Patients should receive the acellular pertussis vaccine after HCT.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Pertussis
ASBMT Recommendations:
- Immunization against pertussis: 5 mg/kg orally once a day
- Maximum dose: 250 mg/dose
- Postexposure prophylaxis: 10 mg/kg orally as a loading dose, then 5 mg/kg orally once a day for 4 days
- Maximum dose: 500 mg/dose (loading dose); 250 mg/dose (following doses)
Comments:
- Recommended as an alternative for immunization against pertussis for HCT recipients with an incomplete vaccination series
- Recommended as the first choice for postexposure prophylaxis for HCT recipients, regardless of vaccination status
- Patients should receive the acellular pertussis vaccine after HCT.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Lyme Disease - Erythema Chronicum Migrans
IDSA, AAN, and ACR Recommendations for Children: 10 mg/kg orally once a day
- Maximum dose: 500 mg/dose
Comments:
- Recommended as an alternative agent for solitary and multiple erythema migrans
- Due to concerns for lower efficacy, macrolide antibiotics (including this drug) are considered second-line agents, and should be reserved for patients in whom other antibiotic classes are contraindicated.
- This drug has not been adequately studied for manifestations of Lyme disease other than erythema migrans.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Babesiosis
IDSA Recommendations:
Ambulatory patients (mild to moderate disease): 10 mg/kg orally on day 1, followed by 5 mg/kg orally every 24 hours
- Maximum dose: 500 mg/dose (day 1); 250 mg/dose (the following days)
Hospitalized patients:
- Acute severe disease: 10 mg/kg IV every 24 hours until symptoms abate, then should switch to all oral therapy (step-down therapy)
- Maximum dose: 500 mg/dose
- Step-down therapy (switch to oral therapy): 5 to 10 mg/kg orally every 24 hours
- Maximum dose: 500 mg/dose
Comments:
- With atovaquone, recommended as preferred treatment regimens for babesiosis patients
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Bacterial Endocarditis Prophylaxis
AHA Recommendations for Children: 15 mg/kg orally as a single dose 30 to 60 minutes before procedure
Maximum dose: 500 mg/dose
Comments:
- Recommended regimen for a dental procedure in patients allergic to penicillins or ampicillin
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Campylobacter Gastroenteritis
The Panel Recommendations for Adolescents: 500 mg orally once a day for 5 days
Comments:
- Recommended as an alternative regimen (depending on susceptibility results) to treat gastroenteritis due to Shigella infection
- Recommended as a preferred regimen to treat mild to moderate gastroenteritis due to Campylobacter infection
- This drug is not recommended for Shigella or Campylobacter bacteremia.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Shigellosis
The Panel Recommendations for Adolescents: 500 mg orally once a day for 5 days
Comments:
- Recommended as an alternative regimen (depending on susceptibility results) to treat gastroenteritis due to Shigella infection
- Recommended as a preferred regimen to treat mild to moderate gastroenteritis due to Campylobacter infection
- This drug is not recommended for Shigella or Campylobacter bacteremia.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Syphilis - Early
The Panel Recommendations for Adolescents: 2 g orally as a single dose
Comments:
- Recommended as an alternative regimen for penicillin-allergic patients for the treatment of early stage syphilis (primary, secondary, and early latent syphilis)
- Chromosomal mutations associated with resistance and treatment failures have been reported with this drug, most commonly in MSM; this drug should be used with caution and only when penicillin, doxycycline, or ceftriaxone therapy is not feasible.
- This drug is not recommended for MSM or pregnant patients.
- Current guidelines should be consulted for additional information.
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Data not available
Comments:
- This drug should be discontinued immediately if signs/symptoms of hepatitis occur.
Precautions
CONTRAINDICATIONS:
- Known hypersensitivity to the active component, erythromycin, any macrolide, or ketolide drug
- History of cholestatic jaundice/hepatic dysfunction associated with prior use of this drug
IV therapy: Safety and efficacy have not been established in patients younger than 16 years.
Oral therapy:
- Otitis media, acute bacterial sinusitis, and community-acquired pneumonia: Safety and efficacy have not been established in patients younger than 6 months.
- Tonsillitis/pharyngitis: Safety and efficacy have not been established in patients younger than 2 years.
- Prevention or treatment of MAC: Safety and efficacy have not been established in HIV-infected patients younger than 18 years.
- Oral suspension in the single dose packet (1 g): Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
IV Administration:
- Administer by IV infusion only, over at least 60 minutes; do not administer as an IM injection or an IV bolus.
- The concentration and infusion rate should be 1 mg/mL over 3 hours or 2 mg/mL over 1 hour.
- Other IV substances, additives, or medications should not be added to this product, or infused simultaneously through the same IV line.
- The oral suspensions and most tablets: Administer with or without food.
- The 600 mg tablets: For increased tolerability, administer with food.
- Oral suspension in bottle: Shake well before each use; use within 10 days. Discard after full dosing is completed.
- Oral suspension in the single dose packet (1 g): After mixing the entire contents of the packet with water (2 ounces [about 60 mL]), mix thoroughly and drink the entire contents immediately; add an additional 2 ounces of water, mix, and drink to ensure complete consumption of dosage.
- Do not administer this drug concurrently with antacids containing aluminum or magnesium.
Storage requirements:
- IV formulation: Before reconstitution, store vials at or below 30C (86F); when diluted according to the instructions, the solution is stable for 24 hours at or below room temperature 30C (86F), or for 7 days if stored under refrigeration 5C (41F).
- Oral formulations:
- Oral suspension in bottle: Store dry powder below 30C (86F); store constituted suspension between 5C to 30C (41F to 86F) and keep tightly closed. Discard when full dosing is completed.
- Oral suspension in the single dose packet (1 g): Stored below 30C (86F).
- Tablets: Store between 15C to 30C (59F to 86F).
Reconstitution/preparation techniques:
- Injection: After reconstitution, the solution must be further diluted before administration.
- Oral suspensions: These products require constitution before use.
- The manufacturer product information should be consulted.
IV compatibility:
- Compatible: Sterile Water for Injection, Normal Saline (0.9% sodium chloride), 1/2 Normal Saline (0.45% sodium chloride), 5% Dextrose in Water, Lactated Ringer's Solution, 5% Dextrose in 1/2 Normal Saline (0.45% sodium chloride) with 20 mEq potassium chloride, 5% Dextrose in Lactated Ringer's Solution, 5% Dextrose in 1/3 Normal Saline (0.3% sodium chloride), 5% Dextrose in 1/2 Normal Saline (0.45% sodium chloride), Normosol-M in 5% Dextrose, Normosol-R in 5% Dextrose
General:
- The IV formulation is indicted for the treatment of patients with infections due to susceptible strains of the designated microorganisms in the specified conditions; the oral formulations are indicated similarly, but limited to mild to moderate infections.
- To reduce the development of drug-resistant organisms and maintain effective therapy, this drug should be used only to treat infections proven or strongly suspected to be caused by susceptible bacteria.
- Culture and susceptibility information should be considered when selecting/modifying antibacterial therapy or, if no data are available, local epidemiology and susceptibility patterns may be considered when selecting empiric therapy.
Patient advice:
- Read the US FDA-approved patient labeling (Patient Information).
- Avoid missing doses and complete the entire course of therapy.
- Discontinue this drug immediately and contact physician if any signs of an allergic reaction occur.
- Contact physician if vomiting and irritability with feeding occur in an infant administered this drug.
- Contact health care provider at once if watery and bloody stools (with or without stomach cramps and fever) develop.
Frequently asked questions
- What are the best antibiotics for a tooth infection?
- What antibiotics kill Covid-19 (coronavirus)?
- What is the Best Antibiotic for Strep Throat?
- Does azithromycin cure chlamydia: How much / how long?
- How long does azithromycin stay in your system?
- What are the best antibiotics for pneumonia?
- What antibiotics are used to treat chlamydia and gonorrhea?
- Can you drink alcohol with Z-Pak (Azithromycin)?
- Was azithromycin in my system long enough to treat chlamydia after throwing up?
More about azithromycin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,311)
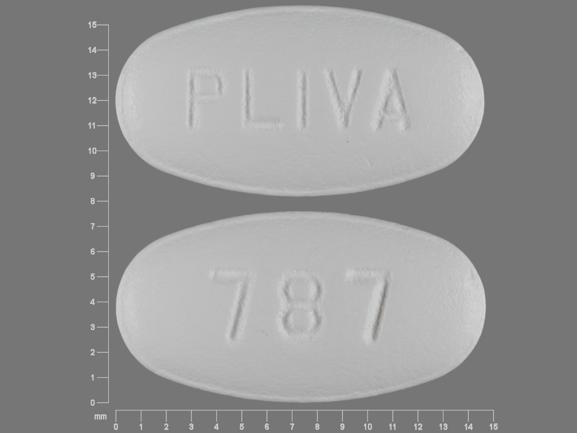
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: macrolides
- Breastfeeding
- En español
Patient resources
Other brands
Zithromax, Azithromycin Dose Pack, Zmax
Professional resources
- Azithromycin Dihydrate monograph
- Azithromycin Dihydrate (FDA)
- Azithromycin Injection (FDA)
- Azithromycin Oral Suspension (FDA)
- Azithromycin Tablets (FDA)
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.