Stelara
Pronunciation: stel-ar’-a
Generic name: ustekinumab [ YOO-sti-KIN-ue-mab ]
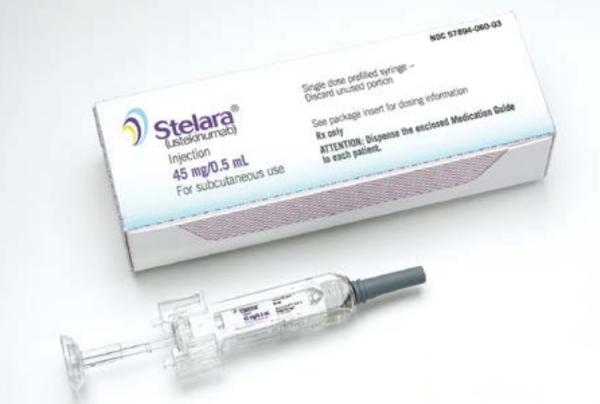
Dosage form: subcutaneous injection (prefilled syringe, vial), intravenous Infusion (vial)
Drug class: Interleukin inhibitors
What is Stelara?
Stelara (ustekinumab) is a prescription medicine used to treat Crohn’s disease, plaque psoriasis, psoriatic arthritis, and ulcerative colitis in eligible adults and children. Stelara works by blocking immune system proteins called IL-12 (interleukin-12) and IL-23 (interleukin-23), which help reduce inflammation, ease pain, swelling, and improve skin symptoms. Stelara is a biologic medication from the drug class interleukin inhibitors.
Stelara is usually administered as an injection under the skin (subcutaneous injection), and Stelara infusion is used for the first dose (induction) for Crohn’s disease and ulcerative colitis. Stelara is given 4 weekly initially, then every 8 to 12 weeks for maintenance treatment, depending on the condition being treated.
Stelara injection was first FDA-approved on September 25, 2009, for adults with moderate to severe psoriasis, and since then, approval has been extended to include other conditions. Stelara's Crohn's disease FDA approval was on Sept. 26, 2016. Crohn’s disease is often written as Crohns disease.
What is Stelara used for?
Stelara is FDA-approved to treat:
- Crohn’s disease (moderately to severely active) in adults.
- Plaque psoriasis (moderate to severe) in patients 6 years and older who are candidates for phototherapy or systemic therapy.
- Psoriatic arthritis (active) in patients 6 years and older.
- Ulcerative colitis (moderately to severely active ) in adults.
Stelara's mechanism of action
Stelara's mechanism of action (MOA) is as an interleukin inhibitor (interleukin-12 and interleukin-23 agonist). Stelara works by targeting immune system proteins called interleukin (IL)-12 and IL-23, which are thought to contribute to long-lasting inflammation in conditions like Crohn’s disease, plaque psoriasis, psoriatic arthritis, and ulcerative colitis. By blocking interleukin, Stelara injection helps reduce inflammation and relieve symptoms of these conditions.
Stelara side effects
Common Stelara side effects
Common Stelara side effects in plaque psoriasis
- Itching (2%)
- Muscle pain (1%)
- Tiredness - fatigue (3%)
- Headache (5%)
- Back pain (1%)
- Dizziness (1%)
- Pharyngolaryngeal pain (1%)
- Injection site redness (1%)
- Flu or cold-like symptoms - nasopharyngitis (8%)
- Upper respiratory tract infection URTI (5%).
The common side effects listed above were experienced by 1% or more of patients treated with Stelara injection (45 mg every 12 weeks) for plaque psoriasis during clinical trials PS STUDY 1 and PS STUDY 2.
Common Stelara side effects in Crohn’s disease
- Flu or cold-like symptoms - nasopharyngitis 11%
- Injection site redness (5%)
- Vaginal yeast infections (5%)
- Bronchitis (5%)
- Itchy skin (4%)
- Urinary tract infection - UTI (4%)
- Sinusitis (3%).
The side effects of Stelara injection for Crohn’s disease occurred in 3% or more of patients receiving a maintenance dose of 90 mg (given as a subcutaneous injection every 8 weeks) during clinical trial CD-3.
Common Stelara side effects in ulcerative colitis
- Flu or cold-like symptoms - nasopharyngitis (24%)
- Headache (10%)
- Stomach pain (7%)
- Influenza (6%)
- Fever (5%)
- Diarrhea (4%)
- Sinusitis (4%)
- Tiredness - fatigue (4%)
- Nausea (3%).
Side effects of Stelara for ulcerative colitis occurred in 3% or more of patients receiving a weight-based maintenance dose during clinical trial UC-2.
Stelara side effects vary according to the condition being treated.
Serious Stelara side effects
Serious side effects of Stelara injection include allergic reactions, serious infections, cancers, and posterior reversible encephalopathy syndrome (PRES).
Allergic reactions. Get emergency medical help if you have signs of an allergic reaction to Stelara: hives, chest pain, difficulty breathing, feeling light-headed, swelling of your face, lips, tongue, or throat.
Serious infections. Serious infections may occur during treatment with Stelara. Call your doctor right away if you have signs of infection, such as fever, chills, muscle pain, shortness of breath, weight loss, diarrhea or stomach pain, burning when you urinate, feeling very tired, skin warmth or redness, painful skin sores, or coughing up blood.
Also, call your doctor at once if you have symptoms of serious side effects, including:
- a mole that has changed in size or color;
- swelling, pain, warmth, or redness anywhere on your body;
- stomach pain that is sudden and severe or comes on slowly, changes in bowel habits (diarrhea or constipation);
- new or worsening cough, sudden chest pain, feeling short of breath;
- pain or burning when you urinate; or
- severe headache, confusion, change in mental status, vision problems, and/or seizure (convulsions).
Also, see the Warnings section.
This is not a complete list of side effects, and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
Serious infections may occur during treatment with Stelara. Call your doctor right away if you have signs of infection, such as fever, chills, muscle pain, shortness of breath, weight loss, diarrhea or stomach pain, burning when you urinate, feeling very tired, skin warmth or redness, painful skin sores, or coughing up blood.
Posterior Reversible Encephalopathy Syndrome (PRES). Ustekinumab may also cause a rare but serious condition affecting the brain called Posterior Reversible Encephalopathy Syndrome (PRES). Tell your doctor right away if you have a headache, confusion, vision problems, or a seizure.
Cancers. Stelara injection may decrease the activity of your immune system, and there may be an increase in your risk for certain types of cancers. Tell your doctor if you have ever had any type of cancer. Some people who are receiving this medicine and have risk factors for skin cancer have developed certain types of skin cancers. During your treatment with this medicine, tell your doctor if you develop any new skin growths.
Noninfectious Pneumonia. Cases of interstitial pneumonia, eosinophilic pneumonia, and cryptogenic organizing pneumonia have been reported during post-approval use of this medicine. If diagnosis is confirmed, discontinue Stelara and treat as appropriate.
Live immunizations should not be used in patients being treated with this medicine.
BCG (Bacillus Calmette and Guérin) vaccine. You should not use this medicine if you have received a BCG within 1 year before, during, or 1 year following treatment.
Tuberculosis (TB) Before you start treatment with this injection, your doctor may perform tests to make sure you do not have tuberculosis.
Before taking this medicine
You should not use Stelara injection or infusion if you:
- are allergic to the active ingredient ustekinumab or any of the inactive ingredients contained in the medicine. See the full list of Stelara ingredients at the bottom of this page.
- have active tuberculosis; or
- have received a BCG (Bacillus Calmette and Guérin) vaccine within the past 12 months.
Tell your doctor if you have ever had tuberculosis, if anyone in your household has tuberculosis, or if you have recently traveled to an area where tuberculosis is common.
To make sure Stelara injection or infusion is safe for you, tell your doctor if you have:
- signs of infection (fever, chills, cough, muscle aches, painful skin sores, diarrhea, pain when you urinate, feeling very tired)
- chronic infections
- new or changing skin lesions
- a latex allergy as the needle cover on the prefilled syringe contains latex
- phototherapy (light therapy)
- allergy shots
- if you recently received or are scheduled to receive any vaccine, people who take this medicine should not receive live vaccines. Tell your doctor if anyone in your house needs a live vaccine. The viruses used in some types of live vaccines can spread to people with a weakened immune system and can cause serious problems.
Some people using this medicine have developed skin cancer (non-melanoma). However, these people may have had a higher risk of skin cancer. Talk to your doctor about this risk and what skin symptoms to watch for. You may need to have regular skin exams.
Pregnancy
It is not known whether this medicine will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant. If you are pregnant, your name may be listed on a pregnancy registry to track the effects of ustekinumab on the baby.
Breastfeeding
It may not be safe to breastfeed while using this medicine. It is thought that Stelara passes into your breast milk in small amounts. Talk to your doctor about the best way to feed your baby if you receive this medicine.
How should I use Stelara?
Before you start treatment with this medicine, your doctor may perform tests to make sure you do not have tuberculosis or other infections.
Follow all directions on your prescription label and read all medication guides or instruction sheets. Use the medicine exactly as directed. Stelara is intended for use under the guidance and supervision of your doctor. Prepare your injection only when you are ready to give it. Do not use if the medicine looks cloudy, has changed colors, or has particles in it. Call your pharmacist for new medicine.
Stelara for Crohn’s disease and ulcerative colitis. The first dose is given through a vein in the arm (intravenous infusion) in a healthcare facility by your healthcare provider. It takes at least 1 hour to receive the infusion. Your next doses will be given as an injection under the skin (subcutaneous injection).
Stelara for psoriasis or psoriatic arthritis. Stelara is given as an injection under the skin (subcutaneous injection) as described below.
Stelara injection instructions (subcutaneous)
- In children 6 years and older, it is recommended that this medicine be administered by a healthcare provider.
- If your doctor decides that you or a caregiver may give your Stelara injections at home, you should receive training on the right way to prepare and inject this medicine.
- Your doctor will determine the right dose for you, the amount for each Stelara injection, and how often you should receive it. Your dose needs may change if you gain or lose weight.
- Do not try to inject yourself unless you or your caregiver has been shown how to use it by your doctor or nurse.
- Inject Stelara under the skin in your upper arms, buttocks, upper legs (thighs) or stomach area (abdomen).
- Do not give a Stelara injection in an area of the skin that is tender, bruised, red or hard.
- Use a different injection site each time you use this medicine.
- Use a needle and syringe only once and then place them in a puncture-proof "sharps" container. Follow state or local laws about how to dispose of this container. Keep it out of the reach of children and pets.
- Be sure to keep all of your scheduled follow-up appointments.
Stelara dosing information
Stelara psoriasis and psoriatic arthritis dose: Given as a subcutaneous injection initially, then 4 weeks later, and then a maintenance dose every 12 weeks.
Stelara Crohn’s disease and ulcerative colitis dose. The first dose is given as an infusion, then it is given as a subcutaneous injection every 8 weeks thereafter.
The dose is dependent on the patient's weight.
Stelara Dosage Forms and Strengths
Subcutaneous Injection
- single-dose prefilled syringe 45 mg/0.5 mL or 90 mg/mL
- single-dose vial 45 mg/0.5 mL
Intravenous Infusion
- single-dose vial 130 mg/26 mL (5 mg/mL)
What happens if I miss a dose?
Call your doctor for instructions if you miss a dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using this medicine?
Avoid being near people who are sick or have infections. Tell your doctor at once if you develop signs of infection.
Do not receive a "live" vaccine while using this medicine, and avoid coming into contact with anyone who has recently received a live vaccine. There is a chance that the virus could be passed on to you. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), zoster (shingles), and nasal flu (influenza) vaccine.
BCG vaccine should not be given for at least 1 year after you receive your last dose of Stelara.
Non-live vaccines (including flu shots) may not work as well during your treatment, and may not fully protect you from disease. Make sure you are current on all vaccines before you begin treatment with this medicine.
Stelara biosimilar
Stelara is a biologic medicine and was the first brand of ustekinumab to be FDA-approved, so it is called the reference product. There are 8 Stelara biosimilars:
- Pyzchiva, Selarsdi, Otulfi , Yesintek, and Steqeyma and Starjemza are interchangeable, which means they may be dispensed when the prescription has been written for Stelara without consulting the prescriber, subject to state laws.
- Wezlana has some presentations that are interchangeable with Stelara and others that are not.
- Imuldosa, is a Stelara biosimilar that is not interchangeable. A non-interchangeable biosimilar can only be dispensed in place of the reference product if the healthcare provider specifically prescribes the biosimilar product by name.
What other drugs will affect this medicine?
Other drugs may interact with Stelara, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all your current medicines and any medicine you start or stop using.
It is important to tell your doctor if you are taking any of the following:
- anticoagulants (blood thinners) such as warfarin (Coumadin, Jantoven)
- medications that suppress the immune system, such as azathioprine (Azasan, Imuran), cyclosporine (Gengraf, Neoral, Sandimmune), methotrexate (Otrexup, Rasuvo, Trexall, Xatmep), sirolimus (Rapamune), and tacrolimus (Astagraf, Envarsus, Prograf)
- oral steroids such as dexamethasone (Hemady), methylprednisolone (Medrol), and prednisone (Rayos).
Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Not all possible interactions are listed here.
Stelara Package Insert
The Stelara Package Insert contains more detailed information about this medicine, including Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Pharmacology, Clinical Studies, Drug Interactions, and more. Discuss any medical questions you have with your doctor or other health care provider. This is not all the information you need to know about this medicine for safe and effective use, and it does not take the place of talking to your doctor about your treatment.
The Package Insert is sometimes called Stelara Prescribing Information (PI) or the FDA label.
Storage
Stelara vials and prefilled syringes
- Store vials and prefilled syringes in a refrigerator between 36°F to 46°F (2°C to 8°C)
- Vials should be stored standing up straight.
- This medicine should be stored in the original carton to protect it from light until time to use it.
- Do not freeze.
- Do not shake.
- If needed, individual Stelara prefilled syringes may also be stored at room temperature up to 30°C (86ºF) for a maximum single period of up to 30 days in the original carton to protect from light. Record the date when the prefilled syringe is first removed from the refrigerator on the carton in the space provided. Once a syringe has been stored at room temperature, it should not be returned to the refrigerator. Discard the syringe if not used within 30 days at room temperature storage.
- Do not use this medicine after the expiration date on the carton or on the prefilled syringe.
Diluted Stelara infusion
- If necessary, the diluted infusion solution may be kept at room temperature up to 25°C (77°F) for up to 7 hours.
- Storage time at room temperature begins once the diluted solution has been prepared.
- The infusion should be completed within 8 hours after the dilution in the infusion bag (cumulative time after preparation including the storage and the infusion period).
- Do not freeze.
- Discard any unused portion of the infusion solution.
Ingredients
Active ingredient: ustekinumab
Inactive ingredients:
Single-dose prefilled syringe for subcutaneous use: contains L-histidine, L-histidine monohydrochloride monohydrate, Polysorbate 80, and sucrose.
Single-dose vial for subcutaneous use: L-histidine, L-histidine hydrochloride monohydrate, Polysorbate 80 and sucrose.
Single-dose vial for intravenous infusion: EDTA disodium salt dihydrate, L-histidine, L-histidine hydrochloride monohydrate, L-methionine, Polysorbate 80, and sucrose.
Stelara Manufacturer
Stelara manufacturer Janssen Biotech, Inc., Horsham, PA 19044, US License No. 1864
Stelara Biosimilars
Biosimilar and interchangeable products are biological products that are highly similar to and have no clinically meaningful differences from the reference product.
Reference products
These are biological products that have already been approved by the FDA, against which biosimilar products are compared. There is 1 for Stelara.
Stelara (ustekinumab) - Janssen Biotech, Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
| Single-Dose Vial | 90 mg/mL Discontinued |
Stelara interchangeable products
Interchangeable biosimilar products can be dispensed by a pharmacist without the intervention of the prescriber of the reference product.
Pharmacy laws for biosimilar prescribing may vary by state.
Otulfi (ustekinumab-aauz) - Fresenius Kabi USA, LLC
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Otulfi information in detail.
Pyzchiva (ustekinumab-ttwe) - Samsung Bioepis Co., Ltd.
| Formulation type | Strength |
|---|---|
| Autoinjector | 45 mg/0.5 mL |
| Autoinjector | 90 mg/mL |
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Pyzchiva information in detail.
Selarsdi (ustekinumab-aekn) - Alvotech USA Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Selarsdi information in detail.
Starjemza (ustekinumab-hmny) - Bio-Thera Solutions, Ltd.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
Steqeyma (ustekinumab-stba) - CELLTRION, Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Steqeyma information in detail.
Wezlana (ustekinumab-auub) - Amgen Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Wezlana information in detail.
Yesintek (ustekinumab-kfce) - Biocon Biologics Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
| Single-Dose Vial | 45 mg/0.5 mL |
View Yesintek information in detail.
Stelara biosimilar products
Biosimilar products can only be dispensed in place of the reference product if the healthcare provider specifically prescribes the biosimilar product by name.
Pharmacy laws for biosimilar prescribing may vary by state
Imuldosa (ustekinumab-srlf) - Accord BioPharma Inc.
| Formulation type | Strength |
|---|---|
| Pre-Filled Syringe | 45 mg/0.5 mL |
| Pre-Filled Syringe | 90 mg/mL |
| Single-Dose Vial | 130 mg/26 mL (5 mg/mL) |
View Imuldosa information in detail.
Wezlana (ustekinumab-auub) - Amgen Inc.
| Formulation type | Strength |
|---|---|
| Autoinjector | 45 mg/0.5 mL |
| Autoinjector | 90 mg/mL |
View Wezlana information in detail.
Popular FAQ
What are 7 key Stelara side effects to watch out for?
Common side effects of Stelara include nasopharyngitis, infections, nausea, and injection site reactions. More serious but rare side effects of Stelara are severe allergic reactions, posterior reversible encephalopathy syndrome (PRES), and a potentially higher risk of cancer.
Continue readingWhat food should I avoid while on Stelara?
There are no known food interactions with Stelara (ustekinumab). However, potential interactions have not been fully studied, so consult your doctor about any necessary dietary adjustments. Stelara is a biologic medication that suppresses parts of the immune system, increasing the risk of infections. For this reason, food safety is critical. Continue reading
Stelara and the Covid Vaccine: What should I know?
While there is limited data on how Stelara specifically affects the COVID-19 vaccine, all non-live vaccines, including COVID-19 vaccines, are generally considered safe for Stelara patients. Continue reading
Does Stelara treat ulcerative colitis?
Yes, Stelara was approved by the FDA on October 21, 2019 for the treatment of adult patients with moderately to severely active ulcerative colitis (UC). UC is a serious and long-term inflammatory disease that affects the large intestine (colon) and rectum. Stelara works by targeting proteins called interleukins (IL)-12 and IL-23 to lower inflammation, a main feature of ulcerative colitis. Continue reading
Is Stelara an immunosuppressant?
Yes, Stelara (ustekinumab) is an immunosuppressant. It is approved to treat certain forms of psoriasis, psoriatic arthritis and moderate to severe Crohn's disease and ulcerative colitis. Continue reading
Does Stelara cause weight gain?
Weight gain was not reported by people taking Stelara (ustekinumab) in clinical trials. Other studies on Stelara and weight changes show mixed results. Continue reading
Does Stelara cause hair loss?
No, Stelara (ustekinumab) has not been shown to commonly cause hair loss in clinical studies. Continue reading
Do I qualify for the Stelara copay card & how can I save?
To qualify for the Stelara copay card you must have commercial or private insurance for Stelara, enroll in the Stelara with Me Savings Program, be at least 6 years of age and not use government-funded insurance programs like Medicare or Medicaid. If you are eligible, you pay $5 per dose with a maximum of $9,450 savings per calendar year. Continue reading
Is Stelara a biologic?
Yes, Stelara (ustekinumab) is a biologic. This biologic drug blocks proteins that lead to inflammation. Continue reading
References
More about Stelara (ustekinumab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (253)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- FDA approval history
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Yesintek, Steqeyma, Wezlana, Selarsdi, ... +3 more
Professional resources
Other brands
Yesintek, Steqeyma, Wezlana, Selarsdi, ... +3 more
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.