Methotrexate (injection)
Generic name: methotrexate (injection) [ meth-oh-TREX-ate ]
Brand names: Methotrexate Sodium, Preservative Free, Otrexup, Rasuvo, RediTrex
Dosage forms: injectable powder for injection (1 g), injectable solution (25 mg/mL; 25 mg/mL preservative-free),
... show all 3 dosage forms
Drug classes: Antimetabolites, Antipsoriatics, Antirheumatics, Other immunosuppressants
What is methotrexate injection?
Methotrexate injection is used in combination with other cancer treatments to treat acute lymphoblastic leukemia and osteosarcoma in adults and children.
Methotrexate injection may also be used alone or in combination to prevent and treat meningeal leukemia, and treat non-Hodgkin lymphoma in adults and children.
Methotrexate injection is used in combination with other cancer treatments to treat gestational trophoblastic neoplasia and breast cancer in adults.
Methotrexate injection is also used alone to treat squamous cell carcinoma of the head and neck in adults.
Methotrexate injection is also used to treat severe psoriasis and rheumatoid arthritis in adults, and to treat active polyarticular juvenile idiopathic arthritis in children.
Methotrexate injection may also be used for purposes not listed in this medication guide.
Methotrexate injection side effects
Get emergency medical help if you have signs of an allergic reaction (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Methotrexate injection can cause serious or fatal side effects. Call your doctor at once if you have:
-
sudden chest pain, wheezing, dry cough, feeling short of breath;
-
swollen lymph glands, night sweats, weight loss;
-
blisters or ulcers in your mouth, red or swollen gums, trouble swallowing, feeling very thirsty;
-
blood in your urine or stools, skin changes such as redness, warmth, swelling, or oozing;
-
unusual bruising or bleeding, new signs of infection (fever, weakness, cough, diarrhea, burning when you urinate);
-
signs of metabolic acidosis--confusion, vomiting, lack of energy, irregular heartbeats;
-
low blood cell counts--fever, chills, bruising or bleeding, pale skin, cold hands and feet, feeling light-headed or short of breath;
-
kidney problems--swelling, urinating less, feeling tired or short of breath;
-
liver problems--loss of appetite, stomach pain (upper right side), tiredness, itching, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
nerve problems--confusion, weakness, drowsiness, coordination problems, feeling irritable, headache, neck stiffness, back pain, vision problems, loss of movement in any part of your body, seizure; or
-
signs of tumor cell breakdown--tiredness, weakness, muscle cramps, nausea, vomiting, diarrhea, fast or slow heart rate, tingling in your hands and feet or around your mouth.
Common side effects of methotrexate may include:
-
low blood cell counts, fever, chills, tiredness, not feeling well;
-
headache, dizziness, cough, chest tightness, trouble breathing;
-
mouth sores, nausea, vomiting, stomach pain, diarrhea, runny or stuffy nose, sneezing, sore throat;
-
abnormal liver function tests; or
-
rash, hair loss, skin lesions, eyes being more sensitive to light.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
Methotrexate injection should not be used during pregnancy to treat arthritis or psoriasis. Methotrexate injection is sometimes used to treat cancer during pregnancy. Tell your doctor if you are pregnant or plan to become pregnant.
Methotrexate injection can cause serious or fatal side effects. Tell your doctor if you have diarrhea, mouth sores, shortness of breath, upper stomach pain, dark urine, numbness or tingling, muscle weakness, confusion, seizures, or skin rash that spreads and causes blistering and peeling.
Before taking this medicine
You should not use methotrexate injection if you are allergic to it.
Methotrexate injection should not be used to treat psoriasis or arthritis if you have:
-
alcoholism, cirrhosis, or liver disease;
-
a blood cell disorder, weak immune system; or
-
if you are pregnant or breastfeeding.
Methotrexate injection is sometimes used to treat cancer in people who have a condition listed above. Your doctor will decide if this treatment is right for you.
Tell your doctor if you have ever had:
-
kidney disease (or if you are on dialysis);
-
breathing problems, fluid build-up around the stomach (ascites), a buildup of fluid around your lungs (also called pleural effusion);
-
history of neurologic problems such as seizures;
-
any type of infection;
-
radiation treatment;
-
alcoholism; or
-
if you plan to have any surgeries with general anesthesia, including dental surgery.
Make sure you are current on all vaccines before you start using methotrexate injection. Tell your doctor if you recently received a vaccine or are scheduled for a booster dose.
Methotrexate injection can harm an unborn baby if the mother or the father is using methotrexate. Methotrexate injection may affect fertility in men or women. Pregnancy could be harder to achieve while either parent is using this medicine. Tell your doctor if you are pregnant.
-
If you are a woman, you may need a pregnancy test to make sure you are not pregnant. Use birth control while using this medicine and for at least 6 months after your last dose.
-
If you are a man, use birth control if your sex partner is able to get pregnant. Keep using birth control for at least 3 months after your last dose.
Do not breastfeed while using this medicine, and for at least 1 week after your last dose.
How is methotrexate injection given?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
Methotrexate injection is usually given once per week. Do not use this medicine more often than prescribed. Follow your doctor's dosing instructions very carefully.
Doses are based on body surface area (height and weight). Your dose may change if you gain or lose weight or if you are still growing.
Methotrexate injection is injected into a muscle, under the skin, or as an infusion into a vein. A healthcare provider will give you this injection and may teach you how to properly use the medication by yourself.
Methotrexate injection is injected in the stomach or thigh when used for psoriasis or arthritis. Do not inject within 2 inches of your navel (belly button), arms or other areas of the body, or areas where the skin is tender, bruised, red, hard, or has scars or stretch marks.
Prepare an injection only when you are ready to give it. Call your pharmacist if the medicine looks cloudy, has changed colors or has particles in it.
Do not reuse a needle or syringe, especially a single-use vial (bottle) or auto-injector. Place them in a puncture-proof "sharps" container and dispose of it following state or local laws.
You will need frequent medical tests, and your next dose may be delayed based on the results.
Using methotrexate injection may increase your risk of developing other cancers. Ask your doctor about this risk.
Follow all storage instructions provided with methotrexate injection. Your pharmacist can provide more information about how to store this medicine.
What happens if I miss a dose?
Call your doctor for instructions if you miss an appointment for your methotrexate injection, or if you forget to use the medicine at home.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose of methotrexate injection can be fatal.
What should I avoid while receiving methotrexate injection?
Methotrexate injection could make you sunburn more easily. Avoid sunlight or tanning beds. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Avoid drinking alcohol. It may increase your risk of liver damage.
Avoid receiving a "live" vaccine, or you could develop a serious infection. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), and zoster (shingles).
Avoid driving or hazardous activity until you know how methotrexate will affect you. Your reactions could be impaired.
What other drugs will affect methotrexate injection?
Tell your doctor about all your other medicines, especially:
-
an antibiotic or sulfa drug, folic acid, mercaptopurine, nitrous oxide, phenytoin, probenecid, dapsone, pyrimethamine;
-
NSAIDs (nonsteroidal anti-inflammatory drugs)--aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac, indomethacin, meloxicam, and others; or
-
stomach acid reducers--esomeprazole, lansoprazole, omeprazole, pantoprazole, Nexium, Prilosec, Protonix, and others.
This list is not complete and many other drugs may affect methotrexate injection. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Popular FAQ
How long does chemo take? Sessions and recovery time?
The duration of chemotherapy varies significantly based on cancer type, treatment goals, and individual patient health. Some patients may complete treatment in a few months, while others require therapy for a year or longer.
Continue readingHow soon can you start chemo after port placement?
Chemotherapy can typically begin within a few days to 2 weeks after port placement, depending on factors like healing progress and treatment urgency.
Continue readingWhy should I take folic acid with methotrexate?
You should take folic acid with methotrexate to help prevent a folate deficiency. Taking methotrexate can lower folate levels in your body and cause symptoms like extreme tiredness, mouth sores, confusion, pale color and weakness. Continue reading
How long does it take for methotrexate to work?
Methotrexate can start working for rheumatoid arthritis within 3 to 6 weeks and symptoms continue to improve over 3 months. For other people it might take a few months before they notice any improvement in their rheumatoid arthritis symptoms. Continue reading
Does methotrexate cause weight gain?
Methotrexate was shown to cause a modest amount of weight gain over 6 months, in a study measuring weight changes in people with rheumatoid arthritis. Continue reading
How do I know if methotrexate is working for rheumatoid arthritis?
To tell if methotrexate treatment is working for your rheumatoid arthritis your doctor will conduct regular blood tests and check-ups. You can also keep a track of your symptoms and looks for signs of improvement. Imaging tests, such as x-rays and musculoskeletal ultrasound (MSUS), may be used. Continue reading
Radiation vs. Chemo: Which cancer treatment is right for you?
Chemotherapy treats cancer throughout the body, while radiation targets specific areas. Each approach has unique benefits depending on the type and stage of cancer, as well as your overall health.
Continue readingWhat is chemo brain and how long does it last?
Chemo brain, also known as chemotherapy-induced cognitive impairment (CICI), chemo fog, or cancer-related cognitive impairment, refers to the cognitive difficulties experienced by many cancer patients during and after chemotherapy treatment. This condition is characterized by a noticeable decline in mental abilities, including memory, learning, attention, and executive functions such as planning and multitasking.
Continue readingWhat are the different brands of methotrexate?
The different brands of methotrexate are Jylamvo, Otrexup, Rasuvo, Trexall, and Xatmep. Continue reading
More about methotrexate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (339)
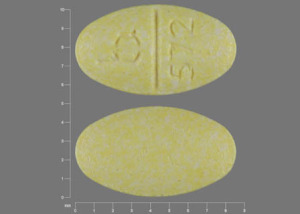
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antimetabolites
- Breastfeeding
Patient resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Professional resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 8.01.