Dyspnea
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
What is dyspnea?
Dyspnea is breathing difficulty or discomfort. You may have labored, painful, or shallow breathing. You may feel breathless or short of breath. Dyspnea can occur during rest or with activity. You may have dyspnea for a short time, or it might become chronic. Dyspnea is often a symptom of a disease or condition.
What signs and symptoms can occur with dyspnea?
- Chest tightness or pain
- A cough, or a coarse or high-pitched noise when you breathe
- Pale and sweaty, cool skin
- Confusion and tiredness
- Bluish-gray lips or nails
What increases my risk for dyspnea?
- Swelling in the throat from an infection or allergic reaction
- Lung conditions such as asthma, COPD, cancer, infection, or a blood clot
- Heart conditions such as abnormal heartbeats, heart failure, or coronary artery disease
- Smoking, exposure to chemicals such as carbon monoxide, or too much aspirin
- A condition that affects your central nervous system, such as a spinal cord injury or nerve damage
- Enlarged abdomen because you are overweight, pregnant, or have ascites (fluid in the abdomen) from liver disease
- Anemia (low red blood cell count), anxiety, panic, or going to a high altitude
How is the cause of dyspnea diagnosed?
Your healthcare provider may ask when your dyspnea began and what you were doing. Tell him or her how often you have dyspnea and what makes it worse or better. Tell your healthcare provider about medicines you take. Describe any other symptoms, such as pain or a fever. Your healthcare provider will listen to you breathe and watch for irregular breathing. You may also need the following:
- A pulse oximeter is a device that measures the amount of oxygen in your blood. A cord with a clip or sticky strip is placed on your finger, ear, or toe. The other end of the cord is hooked to a machine.
- Blood tests may show your healthcare provider if you are at risk for blood clots or heart failure. Blood tests can also show if you have anemia or an infection.
- X-ray pictures may show signs of infection or fluid around your heart or lungs.
- Exercise tests help your healthcare provider learn if you have symptoms, along with dyspnea, that limit activity. Symptoms include leg pain, fatigue, and weakness. Exercise tests can also show if your dyspnea is caused by heart problems.
- CT scan pictures may show blood clots or an area of disease in your lungs. You may be given contract liquid to help your lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart.
- An EKG is a test that measures the electrical activity of your heart.
How is dyspnea treated?
You may need treatment if your symptoms prevent you from doing your daily activities. The condition causing your dyspnea may need to be treated. You may also need the following to improve your symptoms:
- Oxygen therapy may be used to help you breathe easier. You may need oxygen if your blood oxygen level is lower than it should be.
- Medicines may be used to treat the cause of your dyspnea. Medicines may reduce swelling in your airway or decrease extra fluid from around your heart or lungs. Other medicines may be used to decrease anxiety and help you feel calm and relaxed.
- Pulmonary rehabilitation is used to reduce your symptoms while keeping you active. You may learn breathing techniques, muscle strengthening, and how to pace yourself when you are active.
How can I manage long-term dyspnea?
- Create an action plan. You and your healthcare provider can work together to create a plan for how to handle episodes of dyspnea. The plan can include daily activities, treatment changes, and what to do if you have severe breathing problems.
- Lean forward on your elbows when you sit. This helps your lungs expand and may make it easier to breathe.
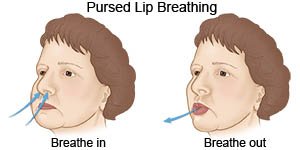
- Use pursed-lip breathing any time you feel short of breath. Breathe in through your nose and then slowly breathe out through your mouth with your lips slightly puckered. It should take you twice as long to breathe out as it did to breathe in.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage and make it harder to breathe. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Reach or maintain a healthy weight. Your healthcare provider can help you create a safe weight loss plan if you are overweight.
- Exercise as directed. Exercise can help your lungs work more easily. Exercise can also help you lose weight if needed. Try to get at least 30 minutes of exercise most days of the week. Your healthcare provider can help you create an exercise plan that is safe for you.
When should I seek immediate care?
- Your signs and symptoms are the same or worse within 24 hours of treatment.
- You have shaking chills or a fever over 102°F.
- You have new pain, pressure, or tightness in your chest.
- You have a new or worse cough or wheezing, or you cough up blood.
- You feel like you cannot get enough air.
- The skin over your ribs or on your neck sinks in when you breathe.
- You have a severe headache with vomiting and abdominal pain.
- You feel confused or dizzy.
When should I call my doctor or specialist?
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Dyspnea
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
