Pain Management: Types of Pain and Treatment Options
We have all experienced pain. But despite it being one of the most common symptoms people seek medical help for, it is also one of the most misunderstood and ineffectively treated.
Part of the reason is that one person’s experience of the same painful event can be significantly different from another’s. In this article, we identify the most common types of pain and offer some suggestions on the best type of treatment. Because there is no one-size-fits-all approach.
Types of Pain
Pain is a general term that describes any kind of unpleasant or uncomfortable sensation in the body.
There are many different types and causes of pain, and these can be grouped into eight different categories to help with pain management:
- Acute pain
- Chronic pain
- Breakthrough pain
- Bone pain
- Nerve pain
- Phantom pain
- Soft tissue pain
- Referred pain.
Acute pain
This starts suddenly and only lasts for a short period (ie, minutes, hours, a couple of days, occasionally a month or two).
It is usually caused by a specific event or injury, such as:
- A broken bone
- A car crash or other type of accident
- A fall
- Burns or cuts
- Dental work
- Labor and childbirth
- Surgery.
Chronic Pain
Chronic pain is pain that has persisted for longer than six months and is experienced most days. It may have originally started as acute pain, but the pain has continued long after the original injury or event has healed or resolved. Chronic pain can range from mild to severe and is associated with conditions such as:
- Arthritis
- Back pain
- Cancer
- Circulation problems
- Diabetes
- Fibromyalgia
- Headache.
Chronic pain can severely affect a person's quality of life and prevent them from returning to work or participating in physical activity. In some people, it may lead to depression or social isolation.
Breakthrough Pain
Breakthrough pain is a sudden, short, sharp increase in pain that occurs in people who are already taking medications to relieve chronic pain caused by conditions such as arthritis, cancer, or fibromyalgia.
Breakthrough pain may also be called a pain flare and it may occur with exercise or physical activity, coughing, illness, stress, or during the period between pain medication doses. The pain level is often severe, but the location of the pain is usually the same as the person’s chronic pain.
Bone Pain
This is a tenderness, aching or discomfort in one or more bones that is present during both exercise and rest.
Bone pain is commonly associated with conditions or diseases that affect the structure or function of bone, such as cancer, a fracture (broken bone), infection, leukemia, mineral deficiency, sickle cell anemia, or osteoporosis. Many pregnant women experience pelvic girdle pain.
Nerve Pain
Nerve pain is caused by nerve damage or inflammation. It is usually described as a sharp, shooting, burning or stabbing pain and may also be called neuralgia or neuropathic pain. Some people describe it as being like an electric shock and it is often worse at night.
Nerve pain can severely interfere with a person's life and affect their sleep, work, and physical activity levels. They are often very sensitive to cold and may experience pain with even the slightest touch. Many people with chronic nerve pain also develop anxiety or depression.
People with neuropathic pain are often very sensitive to touch or cold and can experience pain as a result of stimuli that would not normally be painful, such as brushing the skin.
Common causes of nerve pain include:
- Alcoholism
- An injury to the brain, a nerve, or the spinal cord
- Cancer
- Circulation problems
- Diabetes
- Herpes zoster (shingles)
- Limb amputation
- Multiple sclerosis
- Stroke
- Vitamin B12 deficiency.
Phantom Pain
Phantom pain is pain that feels like it is coming from a body part that is no longer there. It is common in people who have had a limb amputated, but is different from phantom limb sensation, which is usually painless.
Historically, Doctors believed phantom pain was a psychological problem but they now realize these are real pain sensations that originate in the spinal cord and brain. It often gets better with time, but managing phantom pain can be challenging in some people.
Soft Tissue Pain
This is pain or discomfort that results from damage or inflammation of the muscles, tissues, or ligaments. It may be associated with swelling or bruising and common causes include:
- Back or neck pain
- Bursitis
- Fibromyalgia
- Rotator cuff injury
- Sciatic pain
- Sports injuries, such as sprains or strains
- Temporomandibular joint (TMJ) syndrome.
Referred pain
This is pain that feels like it is coming from one particular location, but is the result of an injury or inflammation in another structure or organ. For example, during a heart attack, pain is often felt in the neck, left shoulder, and down the right arm. An injury or inflammation of the pancreas is often felt as constant pain in the upper stomach area that radiates to the back. A ruptured spleen can cause pain in the shoulder blade.
Referred pain happens because there is a network of interconnecting sensory nerves, that supply many different tissues. An injury in one area of the network can be mistakenly interpreted by the brain as being in a different part of the network.
What Type of Pain do I Have?
Sometimes it can be hard to identify exactly what type of pain you are experiencing. The checklist below can help you to identify your pain type and other contributing factors. Fill it in before you see your doctor. 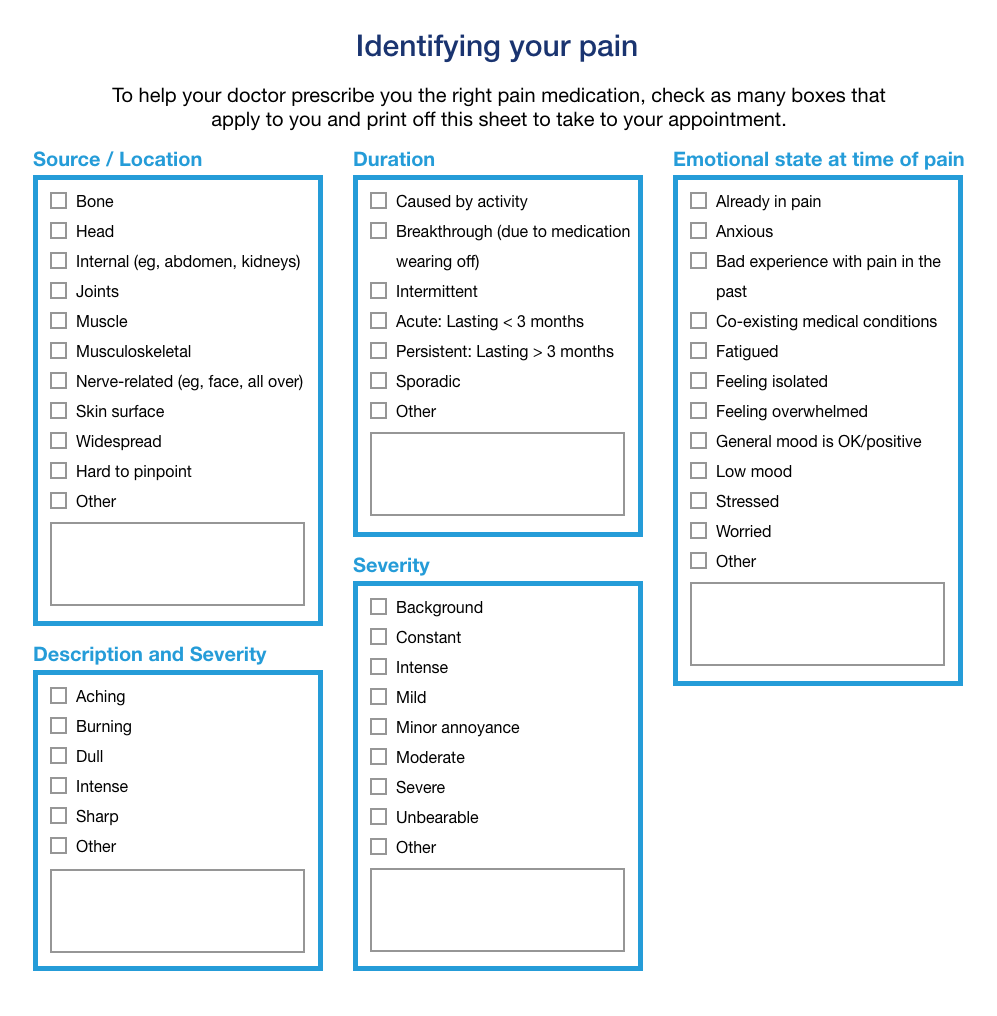
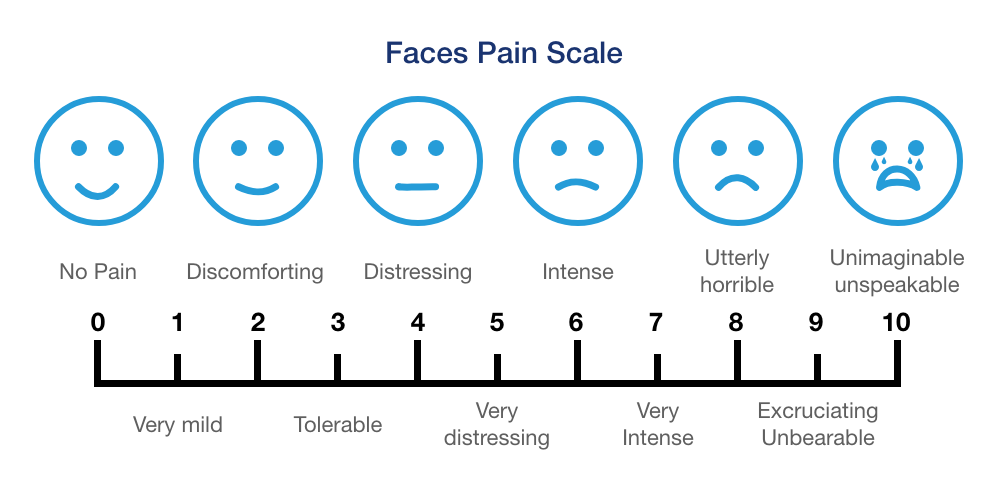
If you have a child that is experiencing pain, The Faces Pain Scale may help. This uses a series of diagrams depicting a face with no pain (0) to intense pain (10).
How Do I Manage My Pain?
There are many different types of pain-relieving medications and each class works in a slightly different way. Most medications can be grouped under one of the following:
- Nonopioids: a medicine that is not similar to morphine (an opioid) but is not addictive (eg, acetaminophen, aspirin, NSAIDs)
- Sodium channel blockers (nonopioid), such as Journavx
- Weak opioids: a medicine that is similar to morphine (an opioid) but not considered as strong (eg, codeine, tramadol)
- Combination opioids: these contain a nonopioid and either a weak opioid or a strong opioid (eg, acetaminophen and hydrocodone)
- Strong opioids: a medicine such as morphine or similar to morphine that has the potential to cause addiction (eg, fentanyl, morphine, oxycodone)
- Other (eg, ketamine)
- Adjuvant treatments: a medicine that can help relieve pain by relieving inflammation or by improving the functioning of other systems (eg, cannabis [Marijuana], capsaicin, gabapentin)
- Nonpharmacological treatments (drug-free treatments), such as psychotherapy or counseling.
The choice of pain-relieving medication comes down to how effective it is for that type of pain and the likelihood of side effects in that particular person.
- Once a pain medication is started, it should be monitored for effectiveness and side effects and the dosage or choice of treatment modified if the pain changes or the choice is deemed unsuitable or ineffective.
- Some types of pain (such as cancer-related pain) have an unpredictable course that can vary dramatically in severity and duration, depending on the type of treatment and disease progression. Pain management needs to have some flexibility to account for this.
- Some people will have more than one type of pain.
- Changing the method of delivery of pain medication may improve its effectiveness; for example, changing from an oral treatment to a patch or a subcutaneous pain pump.
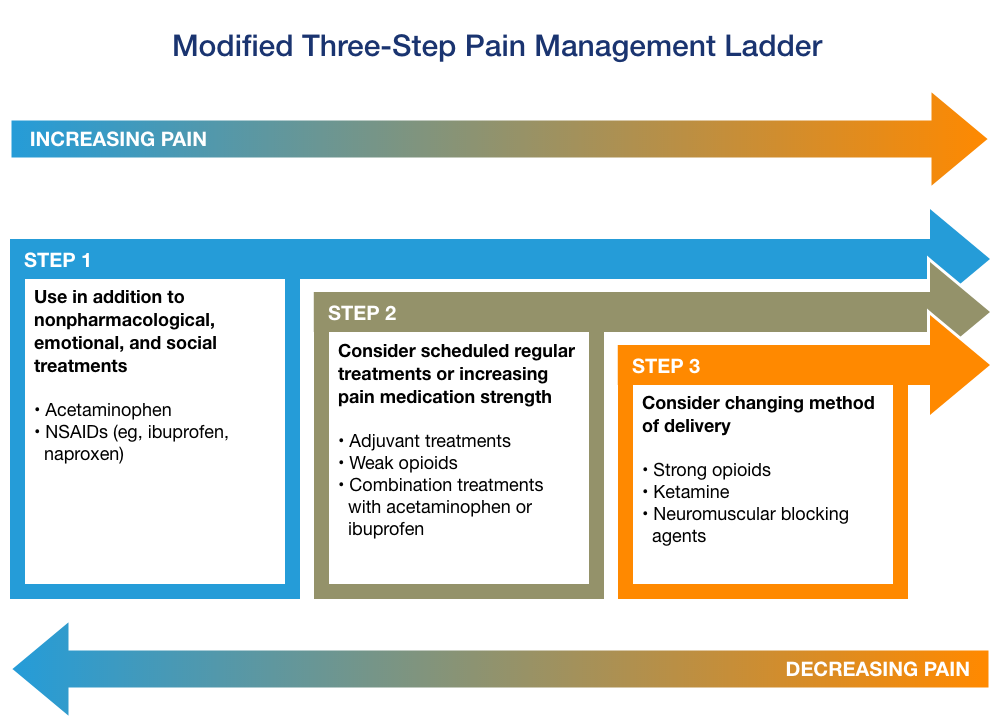
Traditionally, most experts have recommended a stepwise approach to pain management, starting with acetaminophen or NSAIDs, then progressing to a weak opioid (such as codeine, dihydrocodeine, or tramadol), before changing to a strong opioid (such as fentanyl, morphine, oxycodone).
However, this “Pain Ladder” was developed in 1986, and other medications that are not analgesics can also be effective at relieving pain. In addition, opioids should only be used for certain types of pain, because of their risk of addiction. Nowadays, a modified three-step pain management ladder may be used, which should always take into account the type of pain.
Pain Management for Specific Types of Pain
Some medications are considered better for some types of pain compared with others, although factors such as the cause of the pain, genetics, interacting medications or supplements, as well as coexisting conditions, can all impact on how effective a medicine is. Possible treatment options for different types of pain are:
- Acute pain: nonopioids, weak opioids, opioids, nonpharmacological treatments such as ice or bioelectric therapy
- Chronic pain: nonopioids, weak opioids, opioids, antidepressants, capsaicin cream, nonpharmacological treatments such as bioelectric therapy, radiation therapy
- Breakthrough pain: short-acting opioid, nonpharmacological treatments such as acupuncture or relaxation techniques
- Bone pain: nonopioids, bisphosphonates, opioids, nutritional supplements, surgery
- Nerve pain: antidepressants, anticonvulsants, capsaicin cream, nonpharmacological treatments such as cognitive-behavioral therapy
- Phantom pain: nonopioids, antidepressants, anticonvulsants, ketamine, nonpharmacological treatments such as acupuncture or repetitive transcranial magnetic stimulation (rTMS)
- Soft tissue pain: nonopioids, corticosteroids, nonpharmacological treatments such as ice, physiotherapy, or ultrasonography
- Referred pain: nonopioids, cold/warm compresses, nonpharmacological treatments such as massage or transcutaneous electrical nerve stimulation (TENS).
Always talk to your doctor about which pain medication is right for you.
Below is a summary of all the different types of pain medications available as well as a list of nonpharmacological treatments.
Nonopioids
Weak opioids
Combination opioids
- Acetaminophen + codeine
- Acetaminophen + hydrocodone
- Acetaminophen + oxycodone
- Acetaminophen + tramadol
- Codeine + acetaminophen + butalbital + caffeine
- Codeine + aspirin + butalbital + caffeine
- Dihydrocodeine + acetaminophen + caffeine
- Hydrocodone + ibuprofen
Strong Opioids
- Alfentanil
- Fentanyl
- Hydrocodone
- Hydromorphone
- Methadone
- Morphine
- Oxycodone
- Oxymorphone
- Sufentanil
Other
Adjuvant treatments
Anxiety
Bone pain
Bowel-related pain
Muscle or joint pain/spasm
Nerve Pain
- Antidepressants (eg, duloxetine, TCAs, SSRIs)
- Anticonvulsants (eg, gabapentin, lamotrigine, pregabalin)
- Cannabidiol
- Capsaicin cream
- Mexiletine
Widespread pain
- Cannabidiol
- Corticosteroids
- Lidocaine/prilocaine
- CNS stimulants
Nonpharmacological treatments
- Acupressure
- Acupuncture
- Alexander technique
- Bioelectric therapy
- Biofeedback
- Braces and supports
- Chiropractic therapy
- Cognitive-behavioral therapy
- Comfort therapy
- Diathermy
- Distraction
- Electromuscular stimulation
- Functional restoration training
- Guided imagery
- Hot/cold packs
- Hypnosis
- Interferential therapy
- Low-level laser therapy
- Magnetic therapy
- Massage
- Mindfulness
- Mirror box
- Multidisciplinary rehabilitation
- Osteopathy
- Physical and occupational therapy
- Psychosocial therapy/counseling
- Qigong
- Radiofrequency ablation
- Repetitive transcranial magnetic stimulation (rTMS)
- Relaxation techniques
- Spinal cord stimulation
- Surgery
- Tai Chi
- Transcutaneous electrical nerve stimulation (TENS)
- Ultrasound
- Yoga
Learn more
- Dosage Charts for Infants and Children
- Should you mix muscle relaxants with alcohol?
- Top 9 Things You Must Know About Naproxen
- Tramadol - Top 8 Things You Need to Know
- What are the risks of mixing pain medications and alcohol?
Treatment options
- Medications for Back Pain
- Medications for Breakthrough Pain
- Medications for Chronic Pain
- Medications for Muscle Pain
- Medications for Neck Pain
- Medications for Neuralgia
- Medications for Neuropathic Pain
Care guides
- Ankle Sprain
- Back Pain
- Chronic Back Pain
- Chronic Pain
- Degenerative Disc Disease
- Dysmenorrhea
- Neck Pain
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.

