Loratadine (Monograph)
Brand names: Alavert, Claritin
Drug class: Second Generation Antihistamines
Introduction
Second generation antihistamine; derivative of azatadine.
Uses for Loratadine
Allergic Rhinitis
Self-medication for symptomatic relief (alone or in fixed combination with pseudoephedrine sulfate) of seasonal allergic rhinitis (e.g., hay fever); use fixed combination preparations only when both antihistamine and nasal decongestant activity are desired.
As effective as astemizole (no longer commercially available in the US), azatadine, chlorpheniramine, clemastine, or terfenadine (no longer commercially available in the US).
Has been used for the symptomatic treatment of perennial allergic rhinitis† [off-label].
Chronic Idiopathic Urticaria
Self-medication for symptomatic relief of pruritus, erythema, and urticaria associated with chronic idiopathic urticaria (e.g., hives); not for prevention of chronic idiopathic urticaria or allergic skin reactions.
Loratadine Dosage and Administration
Administration
Oral Administration
Administer conventional tablets, orally disintegrating tablets, and fixed-combination tablets orally without regard to meals.
Orally disintegrating tablets: Place tablet on the tongue, allow it to disintegrate (within a few seconds), then swallow with or without water.
Fixed-combination loratadine/pseudoephedrine tablets: Swallow whole; do not break, crush, chew, or dissolve. Administer Claritin-D 24 Hour tablets with a full glass of water.
Dosage
Fixed-combination tablets formulated for 12-hour dosing contain 5 mg of loratadine and 60 mg of pseudoephedrine sulfate in an immediate-release outer shell and 60 mg of pseudoephedrine sulfate in an extended-release matrix core that slowly releases the drug.
Fixed-combination tablets formulated for 24-hour dosing contain 10 mg of loratadine in an immediate-release outer shell and 240 mg of pseudoephedrine sulfate in an extended-release matrix core that slowly releases the drug.
Pediatric Patients
Allergic Rhinitis
Oral
Self-medication in children 2 to <6 years of age: 5 mg once daily (as oral solution).
Self-medication in children ≥6 years of age: 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).
Self-medication in children ≥12 years of age: 5 mg every 12 hours (in fixed combination with 120 mg pseudoephedrine sulfate as the 12-hour formulation [e.g., Alavert Allergy & Sinus, Claritin-D 12 Hour]) or 10 mg once daily (in fixed combination with 240 mg pseudoephedrine sulfate as the 24-hour formulation [Claritin-D 24 Hour]).
Chronic Idiopathic Urticaria
Oral
Children 2–5 years of age: Not recommended for self-medication; a dosage of 5 mg once daily (as oral solution) has been recommended when clinicians prescribe the drug in children 2–5 years of age.
Self-medication in children ≥6 years of age: 10 mg once daily.
Adults
Allergic Rhinitis
Oral
Self-medication: 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).
Self-medication: 5 mg every 12 hours (in fixed combination with 120 mg pseudoephedrine sulfate as the 12-hour formulation) or 10 mg once daily (in fixed combination with 240 mg pseudoephedrine sulfate as the 24-hour formulation).
Chronic Idiopathic Urticaria
Oral
Self-medication: 10 mg once daily.
Prescribing Limits
Pediatric Patients
Allergic Rhinitis
Oral
Self-medication in children 2 to <6 years of age: Maximum 5 mg once daily (as oral solution).
Self-medication in children ≥6 years of age: Maximum 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).
Self-medication in children ≥12 years of age: Maximum 10 mg daily (in fixed combination with pseudoephedrine sulfate as the 12-hour or 24-hour formulations).
Adults
Allergic Rhinitis
Oral
Self-medication : Maximum 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).
Self-medication: Maximum 10 mg daily (in fixed combination with pseudoephedrine sulfate as the 12-hour or 24-hour formulations).
Special Populations
Hepatic Impairment
Self-medication: Consult a clinician.
Children 2–5 years of age with hepatic failure: 5 mg every other day (as oral solution).
Adults and children ≥6 years of age with hepatic failure: 10 mg every other day (as conventional or orally disintegrating tablets or oral solution).
Fixed-combination loratadine/pseudoephedrine sulfate preparations generally should not be used in patients with hepatic impairment.
Renal Impairment
Self-medication: Consult a clinician.
Children 2–5 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 5 mg every other day (as oral solution).
Adults and children ≥6 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 10 mg every other day (as conventional or orally disintegrating tablets or oral solution).
Fixed-combination loratadine/pseudoephedrine sulfate preparations in adults and children ≥12 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 5 mg of loratadine once daily (when the 12-hour formulation is used) or 10 mg of loratadine every other day (when the 24-hour formulation is used).
Cautions for Loratadine
Contraindications
-
Known hypersensitivity to loratadine or any ingredient in the formulation.
Warnings/Precautions
Warnings
Phenylketonuria
Alavert orally disintegrating tablets contain aspartame (NutraSweet), which is metabolized in the GI tract to provide 8.4 mg of phenylalanine per tablet.
Sensitivity Reactions
Possible rash. Urticaria, pruritus, purpura, photosensitivity reaction, erythema multiforme, and anaphylaxis reported rarely.
General Precautions
Use of Fixed Combinations
When using fixed-combination preparation containing pseudoephedrine sulfate, consider the cautions, precautions, and contraindications associated with pseudoephedrine.
GI Obstruction and Esophageal Perforation
Mechanical upper GI obstruction and esophageal perforation reported rarely with a previously marketed formulation of Claritin-D 24 Hour tablets; individuals with a history of difficulty in swallowing tablets, a known upper GI narrowing, or abnormal esophageal peristalsis should not use the Claritin-D 24 Hour preparation since it is not known whether the currently commercially available formulation has potential for this effect.
Specific Populations
Pregnancy
Category B.
Lactation
Loratadine and its active metabolite desloratadine distribute readily into milk; pseudoephedrine (a component of fixed combination preparations) also distributes into milk. Caution advised; discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of loratadine alone or in fixed combination with pseudoephedrine sulfate not established in children <2 or <12 years of age, respectively.
Risk of overdosage and toxicity (including death) in children <2 years of age receiving OTC preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection. Limited evidence of efficacy for these preparations in this age group; appropriate dosages not established. Therefore, FDA recommended not to use such preparations in children <2 years of age; safety and efficacy in older children under evaluation. FDA recommends that parents and caregivers adhere to dosage instructions and warnings on the product labeling that accompanies the preparation and consult a clinician about any concerns. Clinicians should ask caregivers about use of OTC cough/cold preparations to avoid overdosage.
Geriatric Use
Conventional or orally disintegrating tablets or oral solution: Risk of somnolence. Because geriatric patients frequently have decreased renal function, evaluate renal function prior to initiation and subsequently thereafter in this age group; adjust dosage if renal impairment exists or develops.
Fixed-combination loratadine/pseudoephedrine sulfate preparations: Safety and efficacy not studied in patients ≥60 years of age. Geriatric patients are more likely to have adverse effects from sympathomimetic amines than younger patients.
Hepatic Impairment
Conventional or orally disintegrating tablets or oral solution: Dosage adjustment recommended. (See Hepatic Impairment under Dosage and Administration.)
Fixed-combination loratadine/pseudoephedrine sulfate preparations: Use not recommended.
Renal Impairment
Conventional or orally disintegrating tablets or oral solution: Dosage adjustment recommended. (See Renal Impairment under Dosage and Administration.)
Fixed-combination loratadine/pseudoephedrine preparations: Dosage adjustment recommended. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Children 2–5 years of age receiving oral solution: Diarrhea, epistaxis, pharyngitis, flu-like symptoms, fatigue, stomatitis, tooth disorder, earache, viral infection, rash.
Children 6–12 years of age receiving oral solution: Nervousness, wheezing, fatigue, hyperkinesia, abdominal pain, conjunctivitis, dysphonia, upper respiratory tract infection.
Adults and children ≥12 years of age receiving conventional or orally disintegrating tablets: Headache, somnolence, fatigue, dry mouth.
Fixed combination loratadine/pseudoephedrine sulfate preparations: Insomnia, dry mouth, headache, somnolence, nervousness, dizziness, fatigue.
Drug Interactions
Metabolized principally by CYP3A4 and to lesser extent by CYP2D6.
No formal drug interaction studies conducted with fixed combination loratadine/pseudoephedrine preparations. When using these preparations, consider drug interactions associated with pseudoephedrine.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP3A4 or CYP2D6: Potential pharmacokinetic interaction (increased plasma concentrations of loratadine and desloratadine). (See Specific Drugs under Interactions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cimetidine |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported |
|
|
Ketoconazole |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported |
|
|
Macrolide antibiotics (e.g., clarithromycin, erythromycin) |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported |
Loratadine Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract following oral administration; in animal studies, 85% of an oral dose was absorbed. Peak plasma concentrations are attained in about 1.5–3.7 hours.
Onset
Antihistaminic effect is apparent within 1–4 hours.
Duration
Antihistaminic effect persists for 12–24 hours.
Food
Food increases the extent of loratadine absorption and delays time to peak plasma concentration by about 1 hour.
Special Populations
In patients with hepatic impairment, increased peak plasma loratadine concentrations and AUC secondary to impaired drug metabolism can occur.
In patients with chronic renal impairment (Clcr ≤30 mL/minute), peak plasma concentrations and AUC of loratadine and desloratadine are increased compared with those in adults with normal renal function.
In geriatric patients, peak plasma concentrations and AUC of loratadine and desloratadine are increased compared to those in younger adults.
Distribution
Extent
Distribution has not been determined. Neither the drug nor its metabolites appear to cross the blood-brain barrier. Loratadine and its metabolites are distributed into breast milk in concentrations that are equivalent to plasma concentrations.
Plasma Protein Binding
97–99% (loratadine); 73–77% (desloratadine).
Elimination
Metabolism
Extensive first-pass metabolism by CYP enzymes in the liver to the active desloratadine metabolite. Metabolized principally by CYP3A4 and to lesser extent by CYP2D6.
Elimination Route
Excreted equally in urine and feces as metabolic products.
Half-life
The mean distribution half-life of loratadine is about 1–2 hours; the mean elimination half-life is 8–15 hours. The mean distribution half-life of desloratadine is about 2–4 hours; the mean elimination half-life is 17–28 hours.
Special Populations
In patients with hepatic impairment, elimination half-life of loratadine and desloratadine is increased with increasing severity of hepatic disease.
In patients with renal impairment (Clcr ≤30 mL/minute), mean elimination half-lives of loratadine and desloratadine appear to be similar to those in patients with normal renal function.
In a limited number of geriatric patients (66–78 years of age), half-lives of loratadine and desloratadine were increased compared to those in younger adults.
Stability
Storage
Oral
Tablets
2–30°C. Protect from excessive moisture.
Orally Disintegrating Tablets
2–25°C. Use tablet immediately after opening individual blister; use within 6 months of opening foil pouch.
Solution
2–25°C.
Fixed-Combination Tablets
15–25°C.
Actions
-
Exhibits specific, selective peripheral H1-receptor antagonistic activity.
-
No appreciable anticholinergic or α-adrenergic blocking activity in vitro.
-
In clinical studies, incidence of CNS effects (e.g., sedation, impaired psychomotor performance) associated with loratadine is similar to that with placebo or terfenadine (no longer commercially in the US) and less than that with first generation antihistamines (e.g., azatadine, chlorpheniramine, clemastine).
Advice to Patients
-
For self-medication, importance of taking only as needed and not exceeding recommended dosage; taking more than recommended dosage may cause drowsiness.
-
For self-medication with loratadine in fixed combination with pseudoephedrine, importance of discontinuing therapy and contacting a clinician if symptoms do not improve within 7 days or are accompanied by fever, or if nervousness, dizziness, or sleeplessness occurs.
-
For self-medication for management of chronic idiopathic urticaria (e.g., hives), importance of understanding that loratadine does not prevent hives. Importance of consulting a clinician before initiating therapy if hives are unusual in color, look bruised or blistered, or do not itch. Importance of discontinuing therapy and contacting a clinician if symptoms do not improve within 3 days or if hives have persisted for >6 weeks.
-
Importance of understanding that chronic idiopathic urticaria may present with other severe allergic reactions, including anaphylactic shock (e.g., trouble swallowing, swelling of the tongue, trouble speaking, wheezing or trouble breathing, dizziness or loss of consciousness, swelling in or around the mouth, drooling). These manifestations may occur when hives first appear or up to several hours later and can be life-threatening if not treated immediately. Importance of immediately seeking emergency help if anaphylactic shock occurs. If an epinephrine auto-injector has been prescribed, importance of carrying this device at all times; never use loratadine as a substitute for the epinephrine auto-injector.
-
Importance of discontinuing the drug immediately and informing a clinician if an allergic or hypersensitivity reaction occurs.
-
Importance of informing patients with phenylketonuria that some orally disintegrating tablet preparations (e.g. Alavert) contain aspartame.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of patients with renal or hepatic impairment, heart disease, hypertension, thyroid disease, diabetes mellitus, or difficulty in urination resulting from prostate enlargement not undertaking self-medication without first consulting a clinician. (See Cautions.)
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
5 mg/5 mL |
Children's Claritin Fruit Flavored Syrup 24 Hour |
Schering-Plough |
|
Children’s Claritin Allergy, Grape Flavor |
Schering-Plough |
|||
|
Tablets |
10 mg* |
Alavert Non-Drowsy Allergy Relief 24 Hour |
Wyeth |
|
|
Claritin Hives Relief |
Schering-Plough |
|||
|
Claritin 24 Hour |
Schering-Plough |
|||
|
Tablets, orally disintegrating |
10 mg |
Alavert Non-Drowsy Allergy Relief 24 Hour |
Wyeth |
|
|
Claritin Reditabs 24 Hour |
Schering-Plough |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release core (containing pseudoephedrine 60 mg) |
5 mg with Pseudoephedrine Sulfate 120 mg |
Alavert Allergy & Sinus D-12 Hour |
Wyeth |
|
Claritin-D 12 Hour |
Schering-Plough |
|||
|
Tablets, extended-release core (pseudoephedrine sulfate only), film-coated |
10 mg with Pseudoephedrine Sulfate 240 mg |
Claritin-D 24 Hour |
Schering-Plough |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 13, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Can you give loratadine to dogs?
- What are the most common skin conditions? (with photos)
- Is it OK to take antihistamines every day?
- Why do you take Claritin with Neulasta?
- Can you take 10mg of loratadine twice a day?
- Can you take antihistamines when pregnant?
More about loratadine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (142)
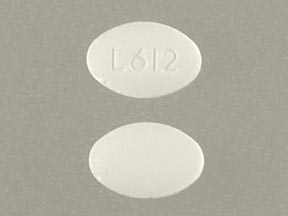
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antihistamines
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Claritin, Alavert, Allergy Relief Tablets, Allergy Relief 24 Hour, Dimetapp Children's ND Non-Drowsy Allergy