Medroxyprogesterone
Generic name: medroxyprogesterone (oral) [ me-DROX-ee-proe-JES-ter-one ]
Brand name: Provera
Dosage form: oral tablet (10 mg; 2.5 mg; 5 mg)
Drug classes: Contraceptives, Hormones / antineoplastics, Progestogens
What is medroxyprogesterone?
Medroxyprogesterone tablets are used to treat abnormal menstrual bleeding, absent or irregular menstrual periods (amenorrhea) and to prevent thickening of the lining of the uterus (endometrial hyperplasia) in postmenopausal women who are taking estrogen hormone replacement therapy. Medroxyprogesterone is a progestin hormone.
Warnings
You should not use medroxyprogesterone if you are pregnant, or if you have liver disease, a hormone-related cancer such as breast or uterine cancer, a history of stroke or blood clot, or abnormal vaginal bleeding that has not been checked by a doctor.
Medroxyprogesterone should not be used to prevent heart disease, stroke, or dementia. This medicine may actually increase your risk of developing these conditions. Long-term use of medroxyprogesterone may increase your risk of breast cancer, heart attack, stroke, or blood clot. Talk with your doctor about your individual risk.
Before taking this medicine
You should not use this medicine if you are allergic to medroxyprogesterone, or if you have:
-
abnormal vaginal bleeding that has not been checked by a doctor;
-
liver disease;
-
a history of heart attack, stroke, or blood clot; or
-
a history of hormone-related cancer, or cancer of the breast, uterus/cervix, or vagina.
Medroxyprogesterone may cause birth defects. Do not use if you are pregnant. Tell your doctor right away if you become pregnant.
Medroxyprogesterone should not be used to prevent heart disease, stroke, or dementia. This medicine may actually increase your risk of developing these conditions.
To make sure medroxyprogesterone is safe for you, tell your doctor if you have:
-
heart problems;
-
liver problems;
-
migraine headaches;
-
a thyroid disorder;
-
endometriosis (severe pelvic pain);
-
jaundice caused by pregnancy or birth control pills;
-
kidney disease;
-
high or low blood levels of calcium;
-
a seizure;
-
diabetes; or
Using this medicine can increase your risk of blood clots, stroke, or heart attack, especially if you have high blood pressure, diabetes, high cholesterol, if you are overweight, or if you smoke.
Long-term use of medroxyprogesterone may increase your risk of cancer of the breast, uterus, or ovaries. Talk with your doctor about this risk.
Do not breastfeed.
How should I take medroxyprogesterone?
Take medroxyprogesterone exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Medroxyprogesterone is usually given for only a few days in a row each month.
Have regular physical exams and self-examine your breasts for lumps on a monthly basis while using this medicine.
If you need major surgery or will be on long-term bed rest, you may need to stop using medroxyprogesterone for a short time. This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using medroxyprogesterone.
Store at room temperature away from moisture and heat.
Dosing information
Usual Adult Dose for Endometrial Hyperplasia -- Prophylaxis:
Oral tablets:
5 or 10 mg daily for 12 to 14 consecutive days per month, in postmenopausal women receiving daily 0.625 mg conjugated estrogens, either beginning on the 1st day of the cycle or the 16 th day of the cycle
Comments:
-Postmenopausal woman with a uterus taking estrogens should also initiate progestin therapy to reduce the risk of endometrial cancer.
-Use of estrogen, alone or in combination with a progestin, should be with the lowest effective dose and for the shortest duration. Starting dose should be the lowest.
-Periodically re-evaluation (e.g., 3 to 6 month intervals) to determine if treatment is still necessary is recommended.
-In women with uterus, endometrial sampling should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding.
Use: Prevention of endometrial hyperplasia in non-hysterectomized postmenopausal women who are receiving daily oral conjugated estrogens 0.625 mg tablets
Usual Adult Dose for Abnormal Uterine Bleeding:
Oral tablets:
-5 or 10 mg daily for 5 to 10 days, beginning on the 16 th or 21 st day of the menstrual cycle
-Dose to produce an optimum secretory transformation of an endometrium that has been adequately primed with either endogenous or exogenous estrogen: 10 mg daily for 10 days beginning on the 16 th day of the cycle
Comments:
-Withdrawal bleeding usually occurs within 3 to 7 days after discontinuing therapy with the oral tablets.
-Patients with a past history of recurrent episodes of abnormal uterine bleeding may benefit from planned menstrual cycling with the oral tablets.
Use: Abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology, such as fibroids or uterine cancer
Usual Adult Dose for Amenorrhea:
Oral tablets:
-5 or 10 mg daily for 5 to 10 days
Dose for inducing an optimum secretory transformation of an endometrium that has been adequately primed with either endogenous or exogenous estrogen:
-10 mg daily for 10 day
Comments:
-Therapy may be started at any time.
-Withdrawal bleeding usually occurs within 3 to 7 days after discontinuing therapy with this drug.
Use: Treatment of secondary amenorrhea due to hormonal imbalance in the absence of organic pathology, such as fibroids or uterine cancer
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking medroxyprogesterone?
Avoid smoking while you are taking medroxyprogesterone. Smoking greatly increases your risk of blood clots.
Medroxyprogesterone side effects
Get emergency medical help if you have signs of an allergic reaction to medroxyprogesterone: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Stop using this medicine and call your doctor at once if you have:
-
signs of a stroke - sudden numbness or weakness (especially on one side of the body), sudden severe headache, slurred speech, problems with vision or balance;
-
signs of a blood clot - sudden vision loss, stabbing chest pain, feeling short of breath, coughing up blood, pain or warmth in one or both legs;
-
heart attack symptoms - chest pain or pressure, pain spreading to your jaw or shoulder, nausea, sweating;
-
liver problems - loss of appetite, upper stomach pain, tiredness, fever, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
unusual vaginal bleeding;
-
confusion, memory problems;
-
a breast lump; or
-
symptoms of depression - sleep problems, weakness, tired feeling, mood changes.
Common medroxyprogesterone side effects may include:
-
spotting or breakthrough bleeding;
-
changes in your menstrual periods;
-
vaginal itching or discharge;
-
headache, dizziness, feeling nervous or depressed;
-
breast tenderness or discharge;
-
premenstrual type symptoms (bloating, fluid retention, mood changes);
-
weight gain;
-
bruising or swelling of your veins;
-
tiredness, trouble sleeping; or
-
vision changes and difficulty wearing contact lenses.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect medroxyprogesterone?
Other drugs may interact with medroxyprogesterone, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all other medicines you use.
Frequently asked questions
More about medroxyprogesterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,476)
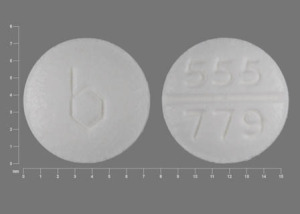
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: contraceptives
- Breastfeeding
Patient resources
Other brands
Depo Provera, depo-subQ provera 104
Professional resources
- MedroxyPROGESTERone monograph
- Medroxyprogesterone (FDA)
- Medroxyprogesterone Injection (FDA)
- Medroxyprogesterone Injection ER (FDA)
Other brands
Provera, Depo Provera, depo-subQ provera 104
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use medroxyprogesterone only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 8.01.