Methotrexate
Generic name: methotrexate (oral) [ meth-oh-TREX-ate ]
Brand names: Trexall, Xatmep Jylamvo
Drug classes: Antimetabolites, Antipsoriatics, Antirheumatics, Other immunosuppressants
What is methotrexate?
Methotrexate interferes with the growth of certain cells of the body, especially cells that reproduce quickly, such as cancer cells, bone marrow cells, and skin cells.
Methotrexate is used to treat leukemia and certain types of cancer of the breast, skin, head and neck, lung, or uterus.
Methotrexate is also used to treat severe psoriasis and rheumatoid arthritis in adults. It is also used to treat active polyarticular-course juvenile rheumatoid arthritis in children.
Methotrexate is sometimes given when other medicines have not been effective.
Methotrexate side effects
Common side effects of methotrexate
Common methotrexate side effects may include:
-
fever, chills, tiredness, not feeling well;
-
low blood cell counts;
-
mouth sores;
-
nausea, stomach pain;
-
abnormal liver function tests;
-
burning skin lesions; or
-
being more sensitive to light.
Serious methotrexate side effects
Get emergency medical help if you have signs of an allergic reaction to methotrexate: (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning in your eyes, skin pain, red or purple skin rash that spreads and causes blistering and peeling).
Methotrexate can cause serious or fatal side effects. Call your doctor at once if you have:
-
sudden chest pain, wheezing, dry cough, cough with mucus, chest pain, feeling short of breath;
-
fever, chills, swollen lymph glands, night sweats, weight loss;
-
blisters or ulcers in your mouth, red or swollen gums, trouble swallowing;
-
vomiting, diarrhea, blood in your urine or stools;
-
skin changes such as redness, warmth, swelling, or oozing;
-
low blood cell counts - fever, chills, tiredness, mouth sores, skin sores, easy bruising, unusual bleeding, pale skin, cold hands and feet, feeling light-headed or short of breath;
-
kidney problems - little or no urination, swelling in your feet or ankles;
-
liver problems - swelling around your midsection, right-sided upper stomach pain, nausea, loss of appetite, dark urine, jaundice (yellowing of the skin or eyes);
-
nerve problems - confusion, weakness, drowsiness, coordination problems, feeling irritable, headache, neck stiffness, vision problems, loss of movement in any part of your body, seizure; or
-
signs of tumor cell breakdown - tiredness, weakness, muscle cramps, nausea, vomiting, diarrhea, fast or slow heart rate, tingling in your hands and feet or around your mouth.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
Methotrexate may cause injury or death to an unborn baby and should not be used during pregnancy to treat arthritis or psoriasis. Methotrexate is sometimes used to treat cancer during pregnancy. Tell your doctor if you are pregnant or plan to become pregnant.
Do not use this medicine to treat psoriasis or rheumatoid arthritis if you have low blood cell counts, a weak immune system, alcoholism or chronic liver disease, or if you are breastfeeding.
YOU MAY NOT NEED TO TAKE METHOTREXATE EVERY DAY. Some people have died after incorrectly taking methotrexate every day. You must use the correct dose for your condition.
Methotrexate can cause serious or fatal side effects. Tell your doctor if you have diarrhea, mouth sores, cough, shortness of breath, upper stomach pain, dark urine, numbness or tingling, muscle weakness, confusion, seizure, or skin rash that spreads and causes blistering and peeling.
Before taking this medicine
You should not use methotrexate if you are allergic to it. You may not be able to take this medicine if you have:
-
alcoholism, cirrhosis, or chronic liver disease;
-
low blood cell counts;
-
a weak immune system or bone marrow disorder; or
-
if you are pregnant or breastfeeding.
Methotrexate is sometimes used to treat cancer in people who have a condition listed above. Your doctor will decide if this treatment is right for you.
To make sure this medicine is safe for you, tell your doctor if you have ever had:
-
liver problems, especially fluid in your stomach (ascites);
-
kidney disease;
-
lung problems, especially fluid in the lungs (pleural effusion);
-
radiation treatments; or
Tell your doctor if you are pregnant or plan to become pregnant. Methotrexate may cause injury or death to an unborn baby and should not be used during pregnancy to treat arthritis or psoriasis. However, methotrexate is sometimes used to treat cancer during pregnancy.
Methotrexate can harm an unborn baby if the mother or the father is using this medicine.
-
If you are a woman, you may need to have a negative pregnancy test before starting this treatment. Use effective birth control to prevent pregnancy while you are using methotrexate and for at least 6 months after your last dose.
-
If you are a man, use effective birth control if your sex partner is able to get pregnant. Keep using birth control for at least 3 months after your last dose.
-
Tell your doctor right away if a pregnancy occurs while either the mother or the father is using methotrexate.
This medicine may affect fertility (ability to have children) in both men and women. However, it is important to use birth control to prevent pregnancy because methotrexate may harm the baby if a pregnancy does occur.
Do not breastfeed while using this medicine, and for at least 1 week after your last dose.
Do not give this medicine to a child without the advice of a doctor.
How should I take methotrexate?
YOU MAY NOT NEED TO TAKE METHOTREXATE EVERY DAY. This medicine is sometimes taken only once per week, or 2 to 4 times per week. Some conditions are treated daily for just a few days followed by a rest period of 1 week or longer before taking the medicine again.
You must use the correct dose. Some people have died after incorrectly taking methotrexate every day.
Take methotrexate exactly as it was prescribed for you. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Measure liquid medicine carefully. Use the dosing syringe provided, or use a medicine dose-measuring device (not a kitchen spoon).
Methotrexate can be toxic to your organs, and may lower your blood cell counts. You will need frequent medical tests, and you may need an occasional liver biopsy or chest X-ray. Your cancer treatments may be delayed based on the results.
If you need to be sedated for dental work, tell your dentist you currently use methotrexate.
Store methotrexate at room temperature away from moisture, heat, and light.
You may store Xatmep in a refrigerator or at room temperature. Avoid freezing or high heat. Throw away any unused Xatmep after 60 days if kept at room temperature.
What happens if I miss a dose?
Call your doctor for instructions if you miss a dose of methotrexate.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose of methotrexate can be fatal.
Overdose symptoms may include bruising or unusual bleeding, mouth sores, vomiting, little or no urination, bloody or tarry stools, or coughing up blood or vomit that looks like coffee grounds.
What to avoid
Avoid drinking alcohol. It may increase your risk of liver damage.
Do not receive a "live" vaccine while using methotrexate, or you could develop a serious infection. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), zoster (shingles), and nasal flu (influenza) vaccine.
Methotrexate could make you sunburn more easily. Avoid sunlight or tanning beds. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
What other drugs will affect methotrexate?
Tell your doctor about all your other medicines, especially:
-
an antibiotic or sulfa drug;
-
NSAIDs (nonsteroidal anti-inflammatory drugs) - aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac, indomethacin, meloxicam, and others;
-
stomach acid reducers - esomeprazole, lansoprazole, omeprazole, pantoprazole, Nexium, Prilosec, Protonix, and others.
Many drugs can interact with methotrexate. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here. Tell your doctor about all your current medicines and any medicine you start or stop using.
Popular FAQ
How long does chemo take? Sessions and recovery time?
The duration of chemotherapy varies significantly based on cancer type, treatment goals, and individual patient health. Some patients may complete treatment in a few months, while others require therapy for a year or longer.
Continue readingHow soon can you start chemo after port placement?
Chemotherapy can typically begin within a few days to 2 weeks after port placement, depending on factors like healing progress and treatment urgency.
Continue readingWhy should I take folic acid with methotrexate?
You should take folic acid with methotrexate to help prevent a folate deficiency. Taking methotrexate can lower folate levels in your body and cause symptoms like extreme tiredness, mouth sores, confusion, pale color and weakness. Continue reading
How long does it take for methotrexate to work?
Methotrexate can start working for rheumatoid arthritis within 3 to 6 weeks and symptoms continue to improve over 3 months. For other people it might take a few months before they notice any improvement in their rheumatoid arthritis symptoms. Continue reading
Does methotrexate cause weight gain?
Methotrexate was shown to cause a modest amount of weight gain over 6 months, in a study measuring weight changes in people with rheumatoid arthritis. Continue reading
How do I know if methotrexate is working for rheumatoid arthritis?
To tell if methotrexate treatment is working for your rheumatoid arthritis your doctor will conduct regular blood tests and check-ups. You can also keep a track of your symptoms and looks for signs of improvement. Imaging tests, such as x-rays and musculoskeletal ultrasound (MSUS), may be used. Continue reading
Radiation vs. Chemo: Which cancer treatment is right for you?
Chemotherapy treats cancer throughout the body, while radiation targets specific areas. Each approach has unique benefits depending on the type and stage of cancer, as well as your overall health.
Continue readingWhat is chemo brain and how long does it last?
Chemo brain, also known as chemotherapy-induced cognitive impairment (CICI), chemo fog, or cancer-related cognitive impairment, refers to the cognitive difficulties experienced by many cancer patients during and after chemotherapy treatment. This condition is characterized by a noticeable decline in mental abilities, including memory, learning, attention, and executive functions such as planning and multitasking.
Continue readingWhat are the different brands of methotrexate?
The different brands of methotrexate are Jylamvo, Otrexup, Rasuvo, Trexall, and Xatmep. Continue reading
More about methotrexate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (339)
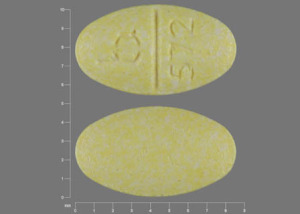
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antimetabolites
- Breastfeeding
Patient resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Professional resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use methotrexate only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 16.01.