Hydralazine
Generic name: hydralazine [ hye-DRAL-a-zeen ]
Brand name: Apresoline
Dosage form: oral tablet (10 mg; 100 mg; 25 mg; 50 mg)
Drug class: Vasodilators
What is hydralazine?
Hydralazine is a vasodilator that works by relaxing the muscles in your blood vessels to help them dilate (widen). This lowers blood pressure and allows blood to flow more easily through your veins and arteries.
Hydralazine is used to treat high blood pressure (hypertension).
Hydralazine may also be used for purposes not listed in this medication guide.
Hydralazine side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Hydralazine may cause serious side effects. Call your doctor at once if you have:
-
chest pain or pressure, pain spreading to your jaw or shoulder;
-
fast or pounding heartbeats;
-
a light-headed feeling, like you might pass out;
-
numbness, tingling, or burning pain in your hands or feet;
-
painful or difficult urination;
-
little or no urination; or
-
lupus-like syndrome--joint pain or swelling with fever, swollen glands, muscle aches, chest pain, vomiting, unusual thoughts or behavior, and patchy skin color.
Common side effects of hydralazine may include:
-
chest pain, fast heart rate;
-
headache; or
-
nausea, vomiting, diarrhea, loss of appetite.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
You should not use hydralazine if you have coronary artery disease, or rheumatic heart disease affecting the mitral valve.
Before taking this medicine
You should not use hydralazine if you are allergic to it, or if you have:
-
coronary artery disease; or
-
rheumatic heart disease affecting the mitral valve.
To make sure hydralazine is safe for you, tell your doctor if you have ever had:
-
kidney disease;
-
angina (chest pain); or
-
a stroke.
It is not known whether this medicine will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
Hydralazine can pass into breast milk, but effects on the nursing baby are not known. Tell your doctor if you are breast-feeding.
Hydralazine is not approved for use by anyone younger than 18 years old.
How should I take hydralazine?
Follow all directions on your prescription label. Do not take hydralazine in larger or smaller amounts or for longer than recommended.
Your blood pressure will need to be checked often. You may also need frequent blood tests.
Keep using this medicine as directed, even if you feel well. High blood pressure often has no symptoms. You may need to use blood pressure medicine for the rest of your life.
Store at room temperature away from moisture and heat.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include rapid heartbeats, warmth or tingling under your skin, chest pain, or fainting.
What should I avoid while taking hydralazine?
Avoid getting up too fast from a sitting or lying position, or you may feel dizzy. Get up slowly and steady yourself to prevent a fall.
What other drugs will affect hydralazine?
Tell your doctor about all your current medicines and any you start or stop using, especially:
-
diazoxide (an injectable blood pressure medication); or
-
an MAO inhibitor--isocarboxazid, linezolid, methylene blue injection, phenelzine, rasagiline, selegiline, tranylcypromine, and others.
This list is not complete. Other drugs may interact with hydralazine, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
More about hydralazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (93)
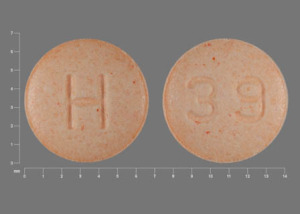
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: vasodilators
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 7.01.