Hydralazine Hydrochloride (Monograph)
Drug class: Direct Vasodilators
Introduction
Vasodilating agent.
Uses for Hydralazine Hydrochloride
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents).
Not considered a preferred agent for initial management of hypertension according to current guidelines for the management of hypertension in adults, but may be used as add-on therapy if BP not adequately controlled with the recommended antihypertensive drug classes (i.e., ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, thiazide diuretics).
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Other hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk, and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Consider initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Severe Hypertension and Hypertensive Crises
One of several recommended parenteral agents for use in the hospital setting to urgently lower BP in severely hypertensive pregnant women, including those with preeclampsia† [off-label].
Historically considered the agent of choice for management of hypertensive emergencies associated with pregnancy (e.g., preeclampsia, eclampsia); however, some clinicians prefer IV labetalol for its more rapid onset, shorter duration of action, and more predictable hypotensive effect.
Parenteral management of severe hypertension when the drug cannot be given orally or when BP must be lowered immediately; other parenteral antihypertensive agents (e.g., labetalol, esmolol, fenoldopam, nicardipine, sodium nitroprusside) usually are preferred for these indications.
Not recommended for the management of severe hypertension or hypertensive emergencies associated with cerebrovascular accidents or in patients with cerebral edema and encephalopathy.
Heart Failure
Used in fixed combination with isosorbide dinitrate as adjunct to standard therapy for the treatment of heart failure in self-identified black patients to improve survival, decrease rate of hospitalization for worsened heart failure, and improve patient-reported functional status.
Current guidelines recommend a combination of drug therapies (e.g., ACE inhibitors, angiotensin II receptor antagonists, angiotensin receptor-neprilysin inhibitors [ARNIs], β-adrenergic blocking agents [β-blockers], aldosterone receptor antagonists) in adults with heart failure to reduce morbidity and mortality.
Combination of hydralazine and isosorbide dinitrate recommended by ACCF and AHA for self-identified black patients with NYHA class III or IV heart failure and reduced ejection fraction who are receiving optimal therapy with ACE inhibitors and β-blockers, unless contraindicated.
ACCF and AHA state that combined therapy with hydralazine and isosorbide dinitrate also can be useful in patients with current or prior symptomatic heart failure with reduced ejection fraction who cannot receive an ACE inhibitor or angiotensin II receptor antagonist† [off-label] because of drug intolerance, hypotension, or renal insufficiency.
Hydralazine Hydrochloride Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker, thiazide diuretic). Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.
Hypertensive Crises
-
Monitor BP closely when parenteral hydralazine is used.
-
Avoid abrupt discontinuance in patients with a marked reduction in BP. To minimize risk for sudden BP increase, reduce dosage gradually.
-
Adults with a hypertensive emergency and a compelling indication—pheochromocytoma crisis, severe preeclampsia or eclampsia: Reduce SBP to <140 mm Hg within the first hour.
-
Adults with a hypertensive emergency and a compelling indication—acute aortic dissection: Reduce SBP to <120 mm Hg within the first 20 minutes.
-
Children and adolescents: Some experts suggest reducing BP by ≤25% of the planned reduction over the first 8 hours, with remainder of planned reduction over next 12–24 hours.
-
Initial goal of IV therapy in adults without a compelling indication is to reduce systolic BP by ≤25% within the first hour, followed by further reduction if stable to 160/110 or 160/100 mm Hg within the next 2–6 hours, avoiding excessive declines in pressure that could precipitate renal, cerebral, or coronary ischemia. If this BP is well tolerated and the patient is clinically stable, further gradual reductions toward normal BP can be implemented in the next 24–48 hours.
Administration
Administer orally or by IM or IV injection. Usually administer orally; may be administered IM or IV if patient unable to take drug orally or if a rapid decrease in BP is required.
Oral Administration
Administer orally 2–4 times daily.
Extemporaneously Compounded Oral Liquid
An extemporaneously compounded oral liquid formulation of hydralazine has been prepared using the commercially available tablets and a commercially available vehicle.
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral liquid formulation of hydralazine have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web] .
|
Concentration Standards |
|---|
|
4 mg/mL |
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by rapid IV injection directly into the vein.
Replace parenteral therapy with oral therapy as soon as possible.
Dosage
Available as hydralazine hydrochloride; dosage expressed in terms of the salt.
20–25 mg of IV hydralazine hydrochloride was approximately equal to 75–100 mg of oral hydralazine hydrochloride in one study.
Pediatric Patients
Hypertension† [off-label]
Oral
Some clinicians recommend an initial dosage of 0.75 mg/kg daily given in 4 divided doses.
Dosages may be increased gradually (over 3–4 weeks) up to a maximum of 7.5 mg/kg (or 200 mg) daily.
Severe Hypertension† [off-label]
IM or IV
Usual dosage: Manufacturer states that 1.7–3.5 mg/kg daily given in 4–6 divided doses has been used.
Severe Hypertension with Life-Threatening Symptoms
IV or IMSome experts recommend initial dosage of 0.1–0.2 mg/kg per dose. May increase dosage up to 0.4 mg/kg per dose. May administer every 4 hours when given by direct IV (“bolus”) injection.
Severe Hypertension with Non-Life-Threatening Symptoms
Oral0.25 mg/kg per dose up to 25 mg per dose; administer every 6–8 hours.
Adults
Hypertension
Oral
Initially, 10 mg 4 times daily for 2–4 days. Dosage then can be increased to 25 mg 4 times daily for the remainder of the week. If necessary, dosage can be increased for the second and subsequent weeks to 50 mg 4 times daily.
Some experts recommend usual dosage of 100–200 mg daily, administered in 2 or 3 divided doses.
Severe Hypertension/Hypertensive Crises
IV
Usual dose: Manufacturer states 20–40 mg, repeated as necessary; can transfer most patients to oral therapy within 24–28 hours.
Alternatively, some experts recommend 10–20 mg repeated every 4–6 hours as needed.
IM
Usual dose: Manufacturer states 20–40 mg, repeated as necessary; can transfer most patients to oral therapy within 24–28 hours.
Urgent Reduction of BP during Pregnancy
IVUsual initial dose is 5 mg, followed by 5–10 mg every 20–40 minutes as necessary to achieve an adequate BP reduction. Maximum total dose of 20 mg has been recommended.
Heart Failure
Fixed-combination Therapy with Isosorbide Dinitrate in Self-identified Black Patients
OralInitially, hydralazine hydrochloride 37.5 mg and isosorbide dinitrate 20 mg (1 tablet of BiDil) 3 times daily. May titrate dosage to a maximum tolerated dosage not to exceed 2 tablets (a total of 75 mg of hydralazine hydrochloride and 40 mg of isosorbide dinitrate) 3 times daily. Rapid titration (over 3–5 days) may be possible; however, slower titration may be needed due to adverse effects. May decrease dosage to as little as one-half of the fixed-combination tablet 3 times daily in patients who experience intolerable effects, but attempt to titrate dosage up once adverse effects subside.
Hydralazine Therapy† [off-label]
OralACCF and AHA recommend initial dosage of hydralazine hydrochloride 25–50 mg 3 or 4 times daily; give concomitantly with isosorbide dinitrate 20–30 mg 3 or 4 times daily. Titrate dosages to levels similar to those recommended for the fixed-combination preparation and administer both drugs at least 3 times daily.
Prescribing Limits
Pediatric Patients
Hypertension
Oral
Maximum 7.5 mg/kg daily (or 200 mg daily).
Adults
Heart Failure
Fixed-combination Therapy with Isosorbide Dinitrate in Self-identified Black Patients
OralMaximum 75 mg of hydralazine hydrochloride and 40 mg of isosorbide dinitrate (2 tablets of BiDil) 3 times daily.
Hydralazine Therapy†
OralMaximum 300 mg daily administered concomitantly with isosorbide dinitrate (maximum 120 mg daily).
Special Populations
Renal Impairment
Lower dosage may be required in severe renal failure.
Geriatric Patients
The manufacturer of the fixed combination of hydralazine hydrochloride and isosorbide dinitrate states that dosage should be selected with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Cautions for Hydralazine Hydrochloride
Contraindications
-
CAD.
-
Mitral valvular rheumatic heart disease.
-
Hypersensitivity to hydralazine hydrochloride or any ingredient in the formulation.
Warnings/Precautions
Warnings
Systemic Lupus Erythematosus (SLE)
May cause SLE (e.g., glomerulonephritis) or rheumatoid arthritis, particularly in patients receiving >200 mg daily dosage for prolonged periods, in slow acetylators of hydralazine, or in those with decreased renal function.
If unexplained signs and symptoms (e.g., arthralgia, fever, chest pain, continued malaise) occur, perform appropriate laboratory studies (e.g., CBCs, ANA titer determinations).
If test results confirm SLE, discontinue hydralazine unless benefit outweighs risk. Signs and symptoms usually regress with hydralazine discontinuance, but residual effects may be detected after many years. Long-term corticosteroid treatment may be necessary if symptoms do not regress.
Sensitivity Reactions
Sulfite Sensitivity
Some formulations contain sulfites that may cause allergic-type reactions (including anaphylaxis and life-threatening or less severe asthmatic episodes) in certain susceptible individuals.
General Precautions
Cardiovascular Effects
Possible precipitation of angina attacks and/or MI; use with caution in patients with suspected coronary artery disease.
May increase pulmonary artery pressure in patients with mitral valvular disease. (See Contraindications.)
Possible orthostatic hypotension; use with caution in patients with cerebrovascular accidents, those who may be volume-depleted, those with preexisting hypotension, or those receiving other hypotensive agents.
Drug Interaction
May paradoxically reduce pressor response to epinephrine.
Peripheral Neuritis
Possible peripheral neuritis (e.g., paresthesia, numbness, tingling); may be caused by pyridoxine deficiency.
If such symptoms occur, use concomitantly with pyridoxine.
Hematologic Effects
Possible blood dyscrasias (e.g., decreased hemoglobin and erythrocytes, leukopenia, agranulocytosis, thrombocytopenia with or without purpura).
If such abnormalities occur, discontinue therapy.
Adequate Patient Monitoring
Perform CBCs and ANA titer determinations before initiation and then periodically thereafter during prolonged therapy (even in asymptomatic patients).
Manufacturers state that a positive ANA titer requires that the implications of the test result be weighed against the benefits from therapy with the drug, whereas some experts state that an increase in ANA titer requires immediate discontinuance of the drug.
Carefully monitor hemodynamic and clinical status in patients with acute MI.
Use of Fixed Combinations
When hydralazine is used in fixed combination with isosorbide dinitrate, consider the cautions, precautions, and contraindications associated with isosorbide dinitrate.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk. Use caution.
Pediatric Use
Safety and efficacy alone or in fixed combination with isosorbide dinitrate not established. Use is based on clinical experience.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. (See Geriatric Patients under Dosage.)
Renal Impairment
Generally considered to be safe; manufacturers state to use with caution in severe renal impairment.
Common Adverse Effects
Headache, palpitation, tachycardia.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β-Blockers |
Additive hypotensive effect Concomitant use may minimize adverse cardiac effects (e.g., tachycardia, precipitation of angina) associated with hydralazine |
Usually used to therapeutic advantage; adjust dosages carefully and monitor for excessive BP reduction |
|
Diazoxide, IV (no longer commercially available in US) |
Possibly profound hypotensive episodes |
|
|
Diuretics |
Additive hypotensive effect Concomitant use may prevent tolerance to hydralazine and also prevent sodium retention and increased plasma volume that may occur after prolonged hydralazine therapy |
Usually used to therapeutic advantage; adjust dosage carefully and monitor for excessive BP reduction |
|
Epinephrine |
Decreased pressor response to epinephrine |
|
|
Hypotensive agents |
Additive hypotensive effect |
Usually used to therapeutic advantage; adjust dosage carefully and monitor for excessive BP reduction |
|
MAO inhibitors |
Synergistic effect, resulting in marked BP decrease |
Use concomitantly with caution |
|
Phosphodiesterase (PDE) inhibitors, selective when using hydralazine in fixed combination with isosorbide dinitrate |
Sildenafil and other selective PDE inhibitors (e.g., tadalafil, vardenafil) profoundly potentiate the vasodilatory effects of isosorbide dinitrate and potentially life-threatening hypotension and/or hemodynamic compromise can result |
Because of the serious risk of concurrent use of isosorbide dinitrate and selective PDE inhibitors, such combined use is contraindicated |
Hydralazine Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Absorption from GI tract is rapid; 66% of an oral dose may be absorbed.
Onset
Following oral administration, antihypertensive effect occurs in 20–30 minutes.
Following IM administration, hypotensive effect occurs within 10–30 minutes.
Following IV administration, hypotensive effect occurs within 5–20 minutes, is maximum in 10–80 minutes.
Duration
Following oral administration, antihypertensive effect lasts 2–4 hours.
Following IM administration, hypotensive effect lasts 2–6 hours.
Following IV administration, hypotensive effect lasts 2–6 hours.
Food
Food increases plasma hydralazine concentrations. The effect of food on the bioavailability of hydralazine when administered in fixed combination with isosorbide dinitrate is not known.
Distribution
Extent
Widely distributed into body tissues in animals; highest concentrations in kidneys, plasma, and liver; high affinity for arterial walls; lower concentrations in the brain, lungs, muscle, heart, and fat.
Readily crosses the placenta.
Distributed into milk.
Plasma Protein Binding
85–87%.
Elimination
Metabolism
Metabolized extensively in the GI mucosa during absorption and in the liver by acetylation, hydroxylation, and conjugation with glucuronic acid.
Acetylation rate is genetically determined; slow acetylators have higher plasma hydralazine concentrations than rapid acetylators at the same oral dose.
Elimination Route
Excreted principally in urine as metabolites and in feces (10%).
Half-life
Plasma half-life: approximately 2–4 hours.
Special Populations
Not known whether hydralazine is dialyzable.
Not known whether impaired renal or hepatic function has an effect on the pharmacokinetics of hydralazine.
Hydralazine may be eliminated more slowly in geriatric patients.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 15–30°C.
Tablets (Hydralazine Hydrochloride and Isosorbide Dinitrate)
Tight, light-resistant containers at 25°C (may be exposed to 15–30°C).
Parenteral
Injection
15–30°; avoid freezing.
Compatibility
Parenteral
Color change develops after dilution with most IV infusion solutions. Color changes that occur over 8–12 hours generally do not indicate loss of potency when stored at ≤30°C.
Actions
-
Mechanism of action as an antihypertensive agent is presumed to be a result of a direct vasodilatory effect on vascular smooth muscle.
Advice to Patients
-
Importance of informing clinician about occurrence of SLE symptoms (e.g., joint or chest pain or fever).
-
Potential to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on individual are known.
-
Importance of consulting clinician if headache continues with repeated dosing.
-
Importance of informing patients receiving hydralazine in fixed combination with isosorbide dinitrate that inadequate fluid intake or excessive fluid loss due to diarrhea, vomiting, or perspiration may result in excessive hypotension, possibly leading to lightheadedness or syncope; if syncope occurs, discontinue treatment and notify clinician immediately.
-
Importance of taking hydralazine regularly and continuously as prescribed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
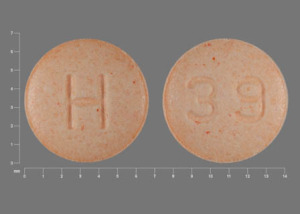
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
10 mg* |
Hydralazine Hydrochloride Tablets |
|
|
25 mg* |
Hydralazine Hydrochloride Tablets |
|||
|
50 mg* |
Hydralazine Hydrochloride Tablets |
|||
|
100 mg* |
Hydralazine Hydrochloride Tablets |
|||
|
Parenteral |
Injection |
20 mg/mL* |
Hydralazine Hydrochloride Injection |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
37.5 mg with Isosorbide Dinitrate 20 mg |
BiDil (scored) |
NitroMed |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about hydralazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (92)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: vasodilators
- Breastfeeding
- En español