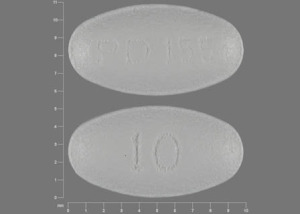
Lipitor
Generic name: atorvastatin [ a-TOR-va-sta-tin ]
Dosage form: oral tablet (10 mg; 20 mg; 40 mg; 80 mg)
Drug class: Statins
What is Lipitor?
Lipitor is used together with diet, weight loss, and exercise to reduce the risk of heart attack and stroke and to decrease the chance that heart surgery will be needed in people who have heart disease or who are at risk of developing heart disease.
Lipitor is also used to lower the amount of fatty substances such as low-density lipoprotein (LDL) cholesterol ('bad cholesterol') and triglycerides in the blood and to increase the amount of high-density lipoprotein (HDL) cholesterol ('good cholesterol') in the blood.
Lipitor may also be used to decrease the amount of cholesterol and other fatty substances in the blood in children and teenagers 10 to 17 years of age who have familial heterozygous hypercholesterolemia (an inherited condition in which cholesterol cannot be removed from the body normally).
Lipitor (atorvastatin) belongs to a class of medications called HMG-CoA reductase inhibitors (statins). It works by slowing the production of cholesterol in the body to decrease the amount of cholesterol that may build up on the walls of the arteries and block blood flow to the heart, brain, and other parts of the body.
Accumulation of cholesterol and fats along the walls of your arteries (a process known as atherosclerosis) decreases blood flow and, therefore, the oxygen supply to your heart, brain, and other parts of your body. Lowering your blood level of cholesterol and fats with Lipitor has been shown to prevent heart disease, angina (chest pain), strokes, and heart attacks.
Warnings
You should not take Lipitor if you have liver disease or cirrhosis.
Lipitor can cause the breakdown of muscle tissue, which can lead to kidney failure. Call your doctor right away if you have unexplained muscle pain, tenderness, or weakness especially if you also have fever, unusual tiredness, or dark urine.
Serious drug interactions can occur when certain medicines are used together with Lipitor. Tell each of your healthcare providers about all medicines you use now, and any medicine you start or stop using.
Avoid eating foods that are high in fat or cholesterol. Lipitor will not be as effective in lowering your cholesterol if you do not follow a cholesterol-lowering diet plan.
Lipitor is only part of a complete program of treatment that also includes diet, exercise, and weight control. Follow your diet, medication, and exercise routines very closely.
Before taking this medicine
You should not use Lipitor if you are allergic to atorvastatin, or if you have liver failure or cirrhosis.
To make sure Lipitor is safe for you, tell your doctor if you have ever had:
-
muscle pain or weakness;
-
diabetes;
-
stroke;
-
a thyroid disorder;
-
a habit of drinking more than 2 alcoholic beverages per day; or
-
kidney disease.
Lipitor can cause the breakdown of muscle tissue, which can lead to kidney failure. This happens more often in women, in older adults, or people who have kidney disease or poorly controlled hypothyroidism (underactive thyroid).
Atorvastatin may harm an unborn baby. Tell your doctor if you are pregnant.
Ask a doctor if it is safe to breastfeed while using Lipitor.
How should I take Lipitor?
Take Lipitor exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
Do not change your dose or stop taking any of your medications without your doctor's advice.
Lipitor is usually taken once per day. Follow your doctor's instructions.
You may take Lipitor tablets with or without food.
It may take up to 2 weeks before your cholesterol levels improve, and you may need frequent blood tests. Even if you have no symptoms, tests can help your doctor determine if Lipitor is effective.
Your treatment may also include diet, exercise, weight control, and blood tests.
Store at room temperature away from moisture, heat, and light.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if you are more than 12 hours late for the dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking Lipitor?
Avoid eating foods high in fat or cholesterol, or Lipitor will not be as effective.
Drinking alcohol may increase your risk of liver damage.
Grapefruit may interact with atorvastatin and cause side effects. Avoid consuming grapefruit products and drinking more than 1.2 liters of grapefruit juice each day.
Lipitor side effects
Get emergency medical help if you have signs of an allergic reaction to Lipitor (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Lipitor can cause the breakdown of muscle tissue, which can lead to kidney failure. Call your doctor right away if you have unexplained muscle pain, tenderness, or weakness especially if you also have fever, unusual tiredness, or dark urine.
Muscle problems may be more likely in older adults and those who have kidney problems, thyroid problems, or take certain other medicines.
Also call your doctor at once if you have:
-
muscle weakness in your hips, shoulders, neck, and back;
-
trouble lifting your arms, trouble climbing or standing;
-
liver problems - loss of appetite, stomach pain (upper right side), tiredness, itching, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
kidney problems - swelling, urinating less, feeling tired or short of breath; or
-
high blood sugar - increased thirst, increased urination, dry mouth, fruity breath odor.
Common Lipitor side effects may include:
-
pain in your bones, spine, joints, or muscles;
-
pain and burning when you urinate, painful urination;
-
muscle spasms;
-
trouble with sleeping;
-
stuffy nose, runny nose, sore throat;
-
pain in arms or legs (limbs).
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect Lipitor?
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which can increase risk of serious muscle problems or make the medicines less effective.
Tell your doctor about all your current medicines. Many drugs can interact with atorvastatin, especially:
-
other cholesterol lowering medicine - gemfibrozil, niacin, fenofibrate, fenofibric acid, and others;
-
antibiotic or antifungal medicine - rifampin, erythromycin, clarithromycin, itraconazole, ketoconazole, posaconazole, and voriconazole;
-
medicine to prevent organ transplant rejection; or
-
antiviral medicine to treat hepatitis C or HIV.
This list is not complete and many other drugs may interact with atorvastatin. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Ingredients
Active ingredient: atorvastatin calcium
Inactive ingredients: calcium carbonate, USP; candelilla wax, croscarmellose sodium, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, Opadry White YS-1-7040 (hypromellose, polyethylene glycol, talc, titanium dioxide); polysorbate 80, simethicone emulsion.
Manufacturer
Distributed by: Parke-Davis, Division of Pfizer Inc., NY, NY 10017, USA.
Popular FAQ
Does Green Tea interact with any drugs?
Drug interactions with green tea can include certain blood pressure medicines, statin cholesterol-lowering treatments, and warfarin, an anticoagulant (blood thinner) used to help prevent blood clots and medicines used to treat hot flashes and night sweats in women due to menopause. Continue reading
Can you use limes or lime juice while taking statin drugs (i.e. atorvastatin)?
Limes, pomegranates, pomelos, and Seville oranges can also interact with some medications, including statins such as atorvastatin. There just hasn't been as much research published regarding how other types of citrus (apart from grapefruit) interact with statins. Large quantities of lime or lime peel should be avoided, although small amounts (such as a twist of lime in a drink) are unlikely to cause a significant interaction. Continue reading
More FAQ
- Do I need to eat food when taking atorvastatin?
- What are the side effects of statins?
- Does Lipitor work better if you take it at night?
- Can Lipitor affect libido?
- How long does atorvastatin stay in the system after stopping the drug?
More about Lipitor (atorvastatin)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (103)
- Drug images
- Latest FDA alerts (9)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Generic availability
- Support group
- Drug class: statins
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Lipitor only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 23.02.H2