Phenylephrine (Monograph)
Brand names: Biorphen, Immphentiv, Vazculep
Drug class: alpha-Adrenergic Agonists
Introduction
α1-adrenergic receptor agonist.
Uses for Phenylephrine
Hypotension
Used parenterally in the setting of anesthesia or septic shock to treat clinically important hypotension resulting principally from vasodilation.
The American College of Obstetricians and Gynecologists (ACOG) and American Society of Anesthesiologists (ASA) have published guidelines on obstetric anesthesia that include recommendations on vasopressor therapy in this setting. ASA states that either IV ephedrine or IV phenylephrine may be used to treat hypotension during neuraxial anesthesia. In the absence of maternal bradycardia, consider phenylephrine over ephedrine.
The Surviving Sepsis guidelines recommend norepinephrine first-line over other vasopressors for treatment of low blood pressure in septic shock. Guidelines give no recommendation for or against use of phenylephrine in this setting.
Phenylephrine has also been used to treat hypotension due to cardiogenic shock† [off-label] in certain patients (e.g., patients with aortic or mitral valve stenosis, patients with hypertrophic cardiomyopathy and left ventricular outflow tract obstruction).
Other Uses
Phenylephrine has been used via intracavernosal injection† [off-label] for the treatment of priapism† [off-label].
Phenylephrine Dosage and Administration
General
Pretreatment Screening
-
Identify and correct intravascular volume depletion and acidosis if present. Acidosis may reduce the effectiveness of phenylephrine.
Patient Monitoring
-
Monitor BP and adjust dosage as necessary to achieve appropriate goals.
-
Monitor renal function during phenylephrine use in patients with septic shock.
Dispensing and Administration Precautions
-
Based on the Institute for Safe Medication Practices (ISMP), phenylephrine is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
Administration
Parenteral Administration
Administer by IV bolus or continuous IV infusion for treatment of clinically important hypotension.
For treatment of hypotension during anesthesia, manufacturers recommend administration by IV injection or continuous infusion; for treatment of septic shock, administer as a continuous IV infusion without an initial IV bolus dose.
Must dilute injection concentrate prior to administration. Ready-to-use 100 mcg/mL must not be further diluted before IV bolus administration.
Commercially available bulk vials are intended for use in a pharmacy admixture program. Penetrate each vial only one time with a suitable sterile transfer device or dispensing set. Dispensing from a pharmacy bulk vial should be completed within 4 hours after the vial is penetrated.
Avoid extravasation; check infusion site for free flow.
Dilution
To prepare solution for bolus IV administration, withdraw 1 mL of phenylephrine hydrochloride injection concentrate from a vial containing 10 mg/mL of the drug and dilute with 99 mL of 5% dextrose or 0.9% sodium chloride injection to produce final concentration of 100 mcg/mL.
To prepare solution for continuous IV infusion, withdraw 1 mL of phenylephrine hydrochloride injection concentrate from a vial containing 10 mg/mL of the drug and add to 500 mL of 5% dextrose or 0.9% sodium chloride injection to produce final concentration of 20 mcg/mL.
Standardize 4 Safety
Standardized concentrations for phenylephrine have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web].
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
80 mcg/mL |
mcg/kg/min |
|
400 mcg/mL |
||
|
Pediatric patients (<50 kg) |
80 mcg/mL |
mcg/kg/min |
|
400 mcg/mL |
Dosage
Adults
Hypotension During Anesthesia
IV
When administered as an IV bolus, manufacturers recommend direct IV bolus doses ranging from 40–250 mcg; usual initial dose is 50 or 100 mcg. Some manufacturers state that additional doses may be administered every 1–2 minutes as needed (not to exceed total dosage of 200 mcg); however, if blood pressure response not adequate, initiation of a continuous IV infusion recommended.
When administered as an IV infusion, manufacturers recommend infusion rate of 10–35 mcg/minute or 0.5–1.4 mcg/kg per minute; generally initiate at a low rate and titrate to effect.
Some manufacturers state that total dosage should not exceed 200 mcg (if given by direct IV injection) or 200 mcg/minute (if given by continuous infusion). Higher dosages do not necessarily produce incremental increases in blood pressure and may cause hypertension and reflex bradycardia.
Septic Shock
IV
Initially, 0.5–6 mcg/kg per minute as a continuous IV infusion; titrate to blood pressure goal.
Higher infusion rates do not necessarily provide greater effect.
Special Populations
Hepatic Impairment
Higher dosages may be required in patients with hepatic cirrhosis.
Renal Impairment
Reduced dosages may be required in patients with end-stage renal disease.
Geriatric Patients
Select dosage carefully, usually starting at low end of recommended range.
Cautions for Phenylephrine
Contraindications
-
Known hypersensitivity to phenylephrine or to any ingredient in the respective formulation.
Warnings/Precautions
Cardiovascular Effects
Risk of severe bradycardia and decreased cardiac output.
May precipitate angina in patients with a history of the condition or with severe atherosclerosis. Also may induce or exacerbate heart failure, and increase pulmonary arterial pressure.
Peripheral and Visceral Ischemia
Can cause severe peripheral and visceral vasoconstriction, reducing blood flow to vital organs; increased risk in patients with substantial peripheral vascular disease.
Renal Toxicity in Septic Shock
In patients with septic shock, phenylephrine may increase the need for renal replacement therapy. Monitor renal function when used in such patients.
Potentiated Pressor Effects
In patients with autonomic dysfunction (e.g., those with spinal cord injuries), blood pressure response to phenylephrine may be increased.
If used in conjunction with oxytocic drugs, pressor response may be augmented, increasing the risk of hemorrhagic stroke.
Extravasation
May cause necrosis or sloughing of tissue if extravasation occurs during IV administration. Avoid extravasation during administration and check infusion site for free flow.
Allergic Reactions
Some formulations of phenylephrine hydrochloride injection contain sulfites, which may cause allergic-type reactions (including anaphylaxis and life-threatening or less severe asthmatic episodes) in susceptible individuals.
Specific Populations
Pregnancy
Data in women undergoing Cesarean delivery receiving phenylephrine injection have not established a drug-associated risk of major birth defects or miscarriage. At recommended dosage, phenylephrine does not significantly affect fetal heart rate or fetal heart rate variability. Data not available on phenylephrine use in the first or second trimester.
Animal studies suggest a potential for fetal malformations if drug administered IV during the period of organogenesis.
Sustained decreases in uterine blood flow due to maternal hypotension associated with fetal bradycardia and acidosis.
If a vasopressor is used in conjunction with oxytocic drugs, the vasopressor effect is potentiated and may result in potentially serious adverse effects.
Lactation
Not known whether phenylephrine or its metabolite distributed into human or animal milk; effects on breast-fed infant and milk production unknown.
Weigh the benefits of breast-feeding along with the mother’s clinical need for the drug and any potential adverse effects on the breast-fed infant from phenylephrine or from the underlying maternal condition.
Pediatric Use
Safety and efficacy of parenteral preparations not established.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Hepatic Impairment
Patients with hepatic cirrhosis may have reduced response.
Renal Impairment
Patients with end-stage renal disease may have increased response.
Common Adverse Effects
Most common adverse effects in patients receiving IV phenylephrine hydrochloride include nausea, vomiting, headache.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
α-adrenergic blocking agents |
May block the effects of both agents |
|
|
α2-adrenergic agonists (e.g., clonidine) |
May potentiate pressor effect of phenylephrine |
|
|
β-adrenergic blocking agents |
May potentiate pressor effect of phenylephrine |
|
|
ACE inhibitors |
May antagonize effects of phenylephrine |
|
|
Amiodarone |
May block the effects of both agents |
|
|
Antidepressants, tricyclic |
May potentiate pressor effect of phenylephrine |
|
|
Atropine |
May potentiate the pressor response to phenylephrine |
|
|
Benzodiazepines |
May reduce pressor effect of phenylephrine |
|
|
Calcium channel blockers (e.g., nifedipine) |
May antagonize pressor effects of phenylephrine |
|
|
Centrally-acting sympatholytics (e.g., guanfacine, reserpine) |
May antagonize pressor effects of phenylephrine |
|
|
Corticosteroids (e.g., hydrocortisone) |
May potentiate pressor effect of phenylephrine |
|
|
Ergot alkaloids (e.g., ergonovine maleate) |
May potentiate pressor effects of phenylephrine |
|
|
MAO inhibitors |
Potentiation of pressor effects of phenylephrine |
|
|
Mixed α- and β-adrenergic blocking agents |
May antagonize pressor effect of phenylephrine |
|
|
Norepinephrine-reuptake inhibitors (e.g., atomoxetine) |
May potentiate pressor effect of phenylephrine |
|
|
Oxytocic drugs |
May potentiate pressor effect of phenylephrine, with risk of hemorrhagic stroke |
|
|
Phenothiazines (e.g., chlorpromazine) |
May block the effects of both agents |
|
|
Phosphodiesterase (PDE) type 5 inhibitors |
May reduce pressor effect of phenylephrine |
Phenylephrine Pharmacokinetics
Absorption
Onset
IV administration: Pressor effect rapid, occurs within minutes.
Duration
IV administration: Pressor effect persists for up to 20 minutes.
Distribution
Extent
Wide distribution into organs and peripheral tissues.
Not known if excreted into human milk.
Elimination
Metabolism
Undergoes extensive metabolism in the liver.
Principally metabolized by sulfotransferase and monoamine oxidase (MAO). Metabolites not pharmacologically active.
Elimination Route
Excreted in urine (86%) mainly as metabolites; unchanged drug accounts for 16% of an IV dose.
Half-life
Terminal elimination half-life: 2.5 hours following IV administration.
Observed effective half-life: Approximately 5 minutes following IV infusion.
Stability
Storage
Parenteral
Injection
Single-dose and pharmacy bulk vials: 20–25°C (may be exposed to 15–30°C); store in original carton and protect from light. Discard bulk vials 4 hours after initial entry.
Diluted solutions: Stable for ≤4 hours at room temperature or ≤24 hours under refrigeration.
Actions
-
Activation of α1-adrenergic receptors on vascular smooth muscle results in vasoconstriction; following IV administration, SBP, DBP, mean arterial pressure, and total peripheral vascular resistance increased.
-
Constricts both arterial and venous blood vessels, although effects on arterial vessels more pronounced.
-
Vasoconstriction occurs in most vascular beds, including renal, pulmonary, and splanchnic arteries but minimal to no effect observed on cerebral blood vessels; hepatic vascular beds also affected.
-
Increased vagal activity causes reflex bradycardia.
-
At clinically relevant doses, increases myocardial work and oxygen requirements.
Advice to Patients
-
Inform patients or caregivers that the primary side effect of phenylephrine is hypertension, and rarely, hypertensive crisis. Patients can also experience bradycardia (in some cases, producing heart block or other cardiac arrhythmias, extra ventricular beats, myocardial ischemia in patients with underlying cardiac disease, pulmonary edema, or rales).
-
Inform patients and caregivers of common, less serious side effects that can occur with phenylephrine, which include chest pain, skin or tissue damage due to drug leakage from the venous catheter into surrounding tissue, headache, nervousness, tremor, numbness/tingling in hands or feet, nausea or vomiting, and excitability, dizziness, sweating, or flushing.
-
Inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs as well as any concomitant illnesses.
-
Advise patients to inform clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
500 mcg/5 mL |
Biorphen (single dose ampule) |
|
|
Immphentiv (ready-to-use vial) |
||||
|
1000 mcg/10 mL |
Immphentiv (ready-to-use vial) |
|||
|
10 mg/mL* |
Biorphen (single-dose ampule and vial) |
|||
|
Vazculep (single-dose vial) |
Exela Pharma Sciences |
|||
|
Phenylephrine Hydrochloride Injection (single-dose vial) |
||||
|
50 mg/5 mL* |
Vazculep (bulk package vial) |
|||
|
Phenylephrine Hydrochloride Injection (bulk package vial) |
||||
|
100 mg/10 mL* |
Vazculep (bulk package vial) |
|||
|
Phenylephrine Hydrochloride Injection (bulk package vial) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about phenylephrine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (24)
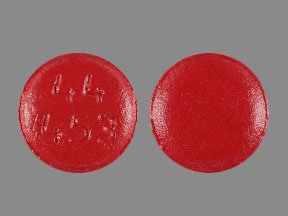
- Drug images
- Latest FDA alerts (5)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: decongestants
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Neo-Synephrine, Biorphen, Vazculep