Empagliflozin (Monograph)
Brand name: Jardiance
Drug class: Sodium-glucose Cotransporter 2 (SGLT2) Inhibitors
Introduction
Antidiabetic agent; sodium-glucose cotransporter 2 (SGLT2) inhibitor.
Uses for Empagliflozin
Type 2 Diabetes Mellitus
Glycemic Control
Used as an adjunct to diet and exercise to improve glycemic control in adults and pediatric patients ≥10 years of age with type 2 diabetes mellitus.
In adults, evaluated as monotherapy or in combination with other antidiabetic agents (e.g., metformin, sulfonylurea, thiazolidinedione, dipeptidyl peptidase-4 [DPP-4] inhibitor, glucagon-like peptide 1 [GLP-1] receptor agonist, insulin).
In pediatric patients, evaluated mainly as add-on therapy to metformin and/or insulin.
Guidelines from the American Diabetes Association (ADA) and other experts generally recommend the use of SGLT2 inhibitors or glucagon-like peptide 1 receptor agonists in patients with type 2 diabetes and established/high risk of atherosclerotic cardiovascular disease (ASCVD), heart failure, and/or chronic kidney disease. When selecting treatment regimen, consider factors such as cardiovascular and renal comorbidities, drug efficacy and adverse effects, hypoglycemic risk, presence of overweight or obesity, cost, access, and patient preferences. Weight management should be included as a distinct treatment goal, and other healthy lifestyle behaviors should be considered.
Not indicated for treatment of type 1 diabetes mellitus.
Not indicated to improve glycemic control in type 2 diabetes mellitus in patients with eGFR <30 mL/minute per 1.73 m2.
Reduction in Risk of Cardiovascular Death
Used to reduce the risk of cardiovascular death in patients with type 2 diabetes mellitus and established cardiovascular disease.
For the treatment of patients with type 2 diabetes mellitus and established ASCVD (or high risk of ASCVD), current clinical practice guidelines generally recommend the use of an SGLT2 inhibitor with proven efficacy in cardiovascular outcome trials.
Beneficial Effects on Renal Function
SGLT2 inhibitors reduce renal tubular glucose reabsorption, weight, systemic blood pressure, intraglomerular pressure, and albuminuria and slow GFR loss through mechanisms that appear to be independent of glucose-lowering effects.
In a cardiovascular outcomes trial in patients with type 2 diabetes and high risk of cardiovascular events, empagliflozin was found to be associated with slower progression of kidney disease and lower rates of renal events.
For the treatment of patients with type 2 diabetes mellitus and CKD, current clinical practice guidelines generally recommend the use of an SGLT2 inhibitor with proven benefit in reducing adverse renal outcomes.
Heart Failure
Used to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with heart failure.
Current expert guidelines on heart failure recommend guideline-directed medical therapy with a combination of the following drugs to reduce morbidity and mortality: angiotensin-converting enzyme (ACE) inhibitors, SGLT2 inhibitors, angiotensin II receptor antagonists, angiotensin receptor-neprilysin inhibitors (ARNIs), β-adrenergic blocking agents, and mineralocorticoid receptor antagonists. SGLT2 inhibitors are recommended in all patients with heart failure (either reduced ejection fraction or preserved ejection fraction), irrespective of the presence of type 2 diabetes mellitus, in the absence of contraindications.
Chronic Kidney Disease
Used to reduce the risk of sustained decline in eGFR, end stage kidney disease, cardiovascular death, and hospitalization in adults with chronic kidney disease at risk for disease progression.
Empagliflozin Dosage and Administration
General
Pretreatment Screening
-
Assess renal function.
-
Assess volume status; volume depletion should be corrected prior to initiation.
Patient Monitoring
-
Assess renal function as clinically indicated.
-
Monitor for signs and symptoms of volume depletion.
-
Monitor for signs and symptoms of urinary tract and genital mycotic infections.
-
Monitor for infections or ulcers of lower limbs.
Other General Considerations
-
Hold empagliflozin for at least 3 days, if possible, prior to major surgery or procedures associated with prolonged fasting. Resume when patient is clinically stable and has resumed oral intake.
Administration
Oral Administration
Commercially available as a single entity preparation and in fixed combination with immediate- or extended-release metformin hydrochloride (Synjardy or Synjardy XR, respectively), linagliptin (Glyxambi), or extended-release metformin hydrochloride and linagliptin (Trijardy XR).
Empagliflozin: administer once daily in the morning.
See full prescribing information for additional administration instructions for combination products.
If dose of empagliflozin is missed, take missed dose as soon as it is remembered followed by resumption of the regular schedule. If missed dose is not remembered until it is almost time for the next dose, skip the missed dose and resume the regular schedule; do not double the dose to replace a missed dose.
Dosage
Pediatric Patients
Type 2 Diabetes Mellitus - Glycemic Control (Patients ≥10 Years of Age)
Empagliflozin Monotherapy
OralInitially, 10 mg once daily in the morning.
If well tolerated, may increase dosage to 25 mg once daily in the morning.
Empagliflozin/Immediate-release Metformin Hydrochloride Fixed-Combination Therapy
OralIndividualize dosage based on current regimen with empagliflozin and/or metformin hydrochloride.
May gradually increase dosage based on effectiveness and tolerability to maximum total daily dosage of 25 mg of empagliflozin and 2 g of metformin hydrochloride administered in 2 divided doses.
Adults
Type 2 Diabetes Mellitus - Glycemic Control or Reduction in Risk of Cardiovascular Death
Empagliflozin Monotherapy
OralInitially, 10 mg once daily in the morning.
If well tolerated, may increase dosage to 25 mg once daily in the morning for additional glycemic control.
Empagliflozin/Linagliptin Fixed-combination Therapy
OralRecommended dosage is 10 mg of empagliflozin and 5 mg of linagliptin once daily in the morning.
If well tolerated, may increase dosage to 25 mg of empagliflozin and 5 mg of linagliptin once daily in the morning.
Empagliflozin/Immediate-release Metformin Hydrochloride Fixed-combination Therapy
OralIndividualize dosage of empagliflozin in fixed combination with immediate-release metformin hydrochloride based on patient's current regimen. May increase dosage gradually based on effectiveness and tolerability up to maximum daily dosage of 25 mg of empagliflozin and 2 g of immediate-release metformin hydrochloride.
Patients currently receiving metformin hydrochloride: Initially, 10 mg of empagliflozin and total daily dosage of immediate-release metformin hydrochloride similar to patient's existing dosage, administered in 2 divided doses.
Patients currently receiving empagliflozin: Initially, same daily dosage of empagliflozin and 1 g of immediate-release metformin hydrochloride, administered in 2 divided doses.
Patients currently receiving both empagliflozin and metformin hydrochloride: Initially, same daily dosage of empagliflozin and a total daily dosage of immediate-release metformin hydrochloride similar to patient's existing dosage, administered in 2 divided doses.
Empagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
OralIndividualize dosage of empagliflozin in fixed combination with extended-release metformin hydrochloride based on patient's current regimen. May increase dosage gradually based on effectiveness and tolerability up to daily maximum of 25 mg of empagliflozin and 2 g of extended-release metformin hydrochloride.
Patients currently receiving metformin hydrochloride: Initially, 10 mg of empagliflozin and total daily dosage of extended-release metformin hydrochloride similar to patient's existing dosage, administered once daily in the morning.
Patients currently receiving empagliflozin: Initially, same daily dosage of empagliflozin and 1 g of extended-release metformin hydrochloride, administered once daily in the morning.
Patients currently receiving both empagliflozin and metformin hydrochloride: Initially, same daily dosage of empagliflozin and total daily dosage of extended-release metformin hydrochloride similar to patient's existing dosage, administered once daily in the morning.
Empagliflozin/Linagliptin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
OralIndividualize dosage of empagliflozin in fixed combination with linagliptin and extended-release metformin hydrochloride based on patient's current regimen. May increase dosage gradually based on effectiveness and tolerability up to maximum daily dosage of 25 mg of empagliflozin, 5 mg of linagliptin, and 2 g of extended-release metformin hydrochloride.
Patients currently receiving metformin hydrochloride (with or without linagliptin): initially, 10 mg of empagliflozin, 5 mg of linagliptin, and total daily dosage of extended-releasemetformin hydrochloride similar to patient's existing dosage, administered once daily in the morning.
Patients currently receiving metformin hydrochloride and empagliflozin (with or without linagliptin): initially, 5 mg of linagliptin and an extended-release metformin hydrochloride and empagliflozin dosage similar to patient's existing total daily dosage, administered once daily in the morning.
Heart Failure
Empagliflozin
Oral10 mg once daily in the morning.
Chronic Kidney Disease
Empagliflozin
Oral10 mg once daily in the morning.
Special Populations
Hepatic Impairment
Empagliflozin Monotherapy
Mild, moderate, or severe: No dosage adjustment necessary.
Empagliflozin/Linagliptin Fixed-combination Therapy
May be used in patients with hepatic impairment.
Empagliflozin/Metformin Hydrochloride Fixed-combination Therapy
Use not recommended.
Empagliflozin/Linagliptin/Metformin Hydrochloride Fixed-combination Therapy
Use not recommended.
Renal Impairment
Empagliflozin Monotherapy
Manufacturer states no dosage adjustment necessary in adults with altered renal function.
Not recommended for glycemic control in patients without established cardiovascular disease or cardiovascular risk factors when eGFR <30 mL/minute per 1.73 m2.
Efficacy and safety trials did not enroll adult patients with GFR <20 mL/minute per 1.73 m2 or on dialysis; however, once enrolled, patients were not required to discontinue therapy for worsening renal function (eGFR <20 mL/minute per 1.73 m2 or requiring dialysis).
Empagliflozin/Linagliptin Fixed-combination Therapy
eGFR ≥30 mL/minute per 1.73 m2: No dosage adjustment necessary.
eGFR <30 mL/minute per 1.73 m2: Use not recommended.
Dialysis: contraindicated.
Empagliflozin/Metformin Hydrochloride Fixed-combination Therapy
eGFR ≥45 mL/minute per 1.73 m2: No dosage adjustment necessary.
eGFR <45 mL/minute per 1.73 m2: Do notinitiate drug..
eGFR <30 mL/minute per 1.73 m2or dialysis: Contraindicated.
Empagliflozin/Linagliptin/Metformin Hydrochloride Fixed-Combination Therapy
eGFR ≥45 mL/minute per 1.73 m2: No dosage adjustment necessary.
eGFR <45 mL/minute per 1.73 m2: Do not initiate drug.
eGFR <30 mL/minute per 1.73 m2 or dialysis: Contraindicated.
Geriatric Patients
Monotherapy
No dosage adjustment necessary based solely on age.
Empagliflozin/Metformin Hydrochloride Fixed-combination Therapy
Monitor renal function frequently after initiating fixed-combination therapy.
Empagliflozin/Linagliptin/Metformin Hydrochloride Fixed-combination Therapy
Monitor renal function frequently after initiating fixed-combination therapy. Recommended dosage of extended-releasemetformin component should start at lower end of dosage range.
Cautions for Empagliflozin
Contraindications
-
Hypersensitivity to empagliflozin or any ingredient in the formulation.
Warnings/Precautions
Diabetic Ketoacidosis in Patients with Type 1 Diabetes Mellitus and Other Ketoacidosis
Ketoacidosis requiring hospitalization reported in patients with type 1 or type 2 diabetes mellitus receiving SGLT2 inhibitors; occur in some cases without markedly elevated blood glucose concentrations (e.g., <250 mg/dL).
Evaluate for presence of ketoacidosis in patients experiencing severe metabolic acidosis regardless of the patient's blood glucose concentration; discontinue empagliflozin and initiate appropriate treatment if confirmed.
Prior to initiating empagliflozin therapy, consider factors that may predispose patients to ketoacidosis (e.g., insulin deficiency, reduced caloric intake, acute febrile illness, ketogenic diet, surgery, volume depletion, alcohol abuse). Risk factors for development of ketoacidosis should be resolved prior to initiation.
Educate patients on signs and symptoms of ketoacidosis and instruct them to discontinue empagliflozin and seek medical attention immediately if signs and symptoms occur.
Withhold empagliflozin therapy if possible in temporary clinical situations that may predispose patients to ketoacidosis resume therapy once patient is clinically stable and able to resume oral intake. Consider discontinuing empagliflozin for ≥3 days prior to surgery for patients with scheduled surgery or procedures that require prolong fasting.
Some clinicians suggest monitoring of urine and/or plasma ketone levels if indicated by the clinical situation.
Volume Depletion
May cause intravascular volume contraction, which can manifest as symptomatic hypotension or acute transient changes in serum creatinine. Acute kidney injury, some requiring hospitalization and dialysis, reported. Patients with impaired renal function (eGFR <60 mL/minute per 1.73 m2), geriatric patients, or patients receiving loop diuretics are at increased risk for volume depletion or hypotension.
Assess and correct intravascular volume status prior to initiating empagliflozin in patients.
Monitor patients for signs and symptoms of volume depletion and renal function after initiating therapy; increase monitoring in clinical situations in which volume contraction is expected.
Urosepsis and Pyelonephritis
May increase risk of serious urinary tract infections, including urosepsis and pyelonephritis. Patients with a history of chronic or recurrent urinary tract infections more likely to develop such infections. Urinary tract infections also occurred more frequently in female than in male patients, and in patients ≥75 years of age.
Prior to initiating empagliflozin therapy, consider patient factors that may predispose to serious urinary tract infections (e.g., history of difficulty urinating; infection of the bladder, kidneys, or urinary tract).
Monitor patients for urinary tract infections and initiate treatment if indicated.
Hypoglycemia
When adding empagliflozin to therapy with an insulin secretagogue (e.g., a sulfonylurea) or insulin, risk of hypoglycemia is increased. In pediatric patients ≥10 years of age, risk of hypoglycemia is higher with empagliflozin regardless of insulin use.
Risk of hypoglycemia may be lowered by a reduction in dosage of the concomitant insulin secretagogue or insulin.
Inform patients of the risk of hypoglycemia and educate on signs and symptoms.
Necrotizing Fasciitis of the Perineum (Fournier's Gangrene)
Necrotizing fasciitis of the perineum (Fournier's gangrene), a rare but serious and life-threatening bacterial infection requiring urgent surgical intervention, reported during postmarketing surveillance in males and females with type 2 diabetes mellitus receiving an SGLT2 inhibitor.
Assess for necrotizing fasciitis in patients receiving empagliflozin who develop pain or tenderness, erythema, or swelling in the genital or perineal area, in addition to fever or malaise. Discontinue empagliflozin if Fournier's gangrene suspected; initiate treatment with broad-spectrum antibiotics and perform surgical debridement if necessary. Monitor blood glucose concentrations closely; initiate alternative antidiabetic agents to maintain glycemic control.
Genital Mycotic Infections
Increased risk of genital mycotic infections in males (e.g., balanitis, balanoposthitis) and females (e.g., vulvovaginitis). Patients with a history of chronic or recurrent genital mycotic infections more likely to develop such infections.
Monitor patients for genital mycotic infections and institute appropriate treatment if these infections occur.
Lower Limb Amputations
Imbalance in incidence of lower limb amputation observed in some clinical studies. Amputation of the toe and midfoot were most frequent, although some involved above and below the knee amputation. Some patients had multiple amputations.
Peripheral artery disease and diabetic foot infection (including osteomyelitis) were most common precipitating medical events leading to need for amputation. Risk of amputation was highest in patients with baseline history of diabetic foot, peripheral artery disease (including previous amputation), or diabetes.
Counsel patients about importance of routine preventative foot care. Monitor patients for signs and symptoms of diabetic foot infection (including osteomyelitis), new pain or tenderness, sores or ulcers involving the lower limbs, and institute appropriate treatment.
Laboratory Test Interference
Increases urinary glucose excretion and will result in false-positive urine glucose tests. In addition, manufacturer states that the 1,5-anhydroglucitol assay is unreliable for monitoring glycemic control.
Alternate methods of monitoring glycemic control should be used.
Use of Fixed Combinations
When empagliflozin is used in fixed combination with metformin hydrochloride, linagliptin, or other drugs, consider the cautions, precautions, contraindications, and interactions associated with the concomitant agent(s) in addition to those associated with empagliflozin.
Hypersensitivity Reactions
Serious hypersensitivity reactions (e.g., angioedema, urticaria) reported.
Discontinue drug if hypersensitivity reaction occurs, institute appropriate treatment, and monitor patients until signs and symptoms resolve.
Specific Populations
Pregnancy
Insufficient data to evaluate drug-associated risk of major birth defects or miscarriage.
Studies in animals indicate that empagliflozin use during pregnancy may affect renal development and maturation.
Not recommended for use in the second or third trimesters of pregnancy.
Lactation
Limited information regarding presence of empagliflozin in human milk, effects on breast-fed infant, or effects on milk production. Distributed into milk in rats. Because of potential risk for serious adverse reactions in breast-fed infants, including potential to affect postnatal renal development, use of empagliflozin during breastfeeding is not recommended.
Pediatric Use
Safety and efficacy in type 2 diabetes mellitus established in pediatric patients ≥10 years of age. Safety profile similar to that observed in adults, with exception of hypoglycemia, which is higher in pediatric patients regardless of concomitant insulin use.
Safety and efficacy not established in pediatric patients for other indications.
Geriatric Use
Geriatric patients with renal impairment expected to experience reduced glycemic efficacy.
Risk of volume depletion-related adverse effects and urinary tract infections increased in patients ≥75 years of age.
Hepatic Impairment
No dosage adjustment necessary in mild, moderate, or severe hepatic impairment.
Renal Impairment
Glucose-lowering effect of empagliflozin 25 mg was reduced in patients with type 2 diabetes mellitus who had worsening renal function in a clinical study. In addition, risk of renal impairment and volume depletion-related and urinary tract infection-related adverse effects increased with worsening renal function. Use of empagliflozin for glycemic control in patients without established cardiovascular disease or cardiovascular risk factors not recommended when eGFR <30 mL/minute per 1.73 m2.
Efficacy and safety trials did not enroll adult patients with GFR <20 mL/minute per 1.73 m2 or on dialysis; however, once enrolled, patients were not required to discontinue therapy for worsening renal function (eGFR <20 mL/minute per 1.73 m2 or requiring dialysis).
Assess renal function before initiating empagliflozin and during therapy. Patients with impaired renal function (eGFR <60 mL/minute per 1.73 m2) may be at increased risk for volume depletion or hypotension.
Common Adverse Effects
Empagliflozin (≥5%): Urinary tract infection, female genital mycotic infections.
Empagliflozin and linagliptin fixed-combination therapy (≥5%): Urinary tract infection, nasopharyngitis, upper respiratory tract infection.
Empagliflozin and metformin fixed-combination therapy (≥5%): Urinary tract infections, female genital mycotic infections, diarrhea, nausea/vomiting, flatulence, abdominal discomfort, indigestion, asthenia, headache.
Empagliflozin, linagliptin, and metformin fixed-combination therapy (≥5%): Upper respiratory tract infection, urinary tract infection, nasopharyngitis, diarrhea, constipation, headache, gastroenteritis.
Drug Interactions
Metabolized principally by glucuronidation via uridine diphosphate-glucuronosyltransferase (UGT) isoenzymes 2B7, 1A3, 1A8, and 1A9.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Does not inhibit, inactivate, or induce CYP isoforms in vitro; no effect of empagliflozin expected on concomitantly administered drugs that are substrates of the major CYP isoforms.
Drugs Affecting Efflux Transport Systems
Substrate of organic anion transporter (OAT) 3 and organic anion transport proteins (OATP) 1B1 and 1B3. Not a substrate of OAT1. Does not inhibit any of these transporters at clinically relevant plasma concentrations; no effect of empagliflozin expected on concomitantly administered drugs that are substrates of these transporters.
Not a substrate of organic cation transporter (OCT)2; does not inhibit OCT2 at clinically relevant plasma concentrations. No effect of empagliflozin expected on concomitantly administered drugs that are substrates of this transporter.
Does not inhibit UGT1A1, 1A3, 1A8, 1A9, or 2B7; no effect of empagliflozin expected on concomitantly administered drugs that are substrates of these UGT isoenzymes. Effect of UGT induction on empagliflozin exposure not studied.
Substrate of P-glycoprotein (P-gp); does not inhibit P-gp at therapeutic doses. Considered unlikely to cause interactions with drugs that are P-gp substrates based on in vitro studies.
Substrate of breast cancer resistance protein (BCRP); does not inhibit BCRP at therapeutic doses.
Empagliflozin Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentration usually attained within 1.5 hours after oral dosing in fasted state. Empagliflozin exposure increases in proportion to the dose.
Bioequivalence studies: Fixed-combination tablets of empagliflozin and immediate-release metformin hydrochloride or empagliflozin and linagliptin are bioequivalent to individual tablets of empagliflozin, metformin hydrochloride, or linagliptin administered concomitantly in equivalent doses.
Food
Administration with a high-fat and high-calorie meal decreased peak concentration and AUC by approximately 37 and 16%, respectively, compared with fasting condition. These changes not considered clinically relevant; administer empagliflozin with or without food.
Special Populations
Mild hepatic impairment (Child-Pugh class A): AUC and peak plasma concentration increased by 23 and 4%, respectively, compared with that in individuals with normal hepatic function.
Moderate hepatic impairment (Child-Pugh class B): AUC and peak plasma concentration increased by 47 and 23%, respectively, compared with that in individuals with normal hepatic function.
Severe hepatic impairment (Child-Pugh class C): AUC and peak plasma concentration increased by 75 and 48%, respectively, compared with that in individuals with normal hepatic function.
Mild renal impairment (eGFR 60 to <90 mL/minute per 1.73 m2): AUC and peak plasma concentration increased by approximately 18 and 20%, respectively, compared with that in individuals with normal renal function.
Moderate renal impairment (eGFR 30 to <60 mL/minute per 1.73 m2): AUC increased by 20% and peak plasma concentrations were similar compared with that in individuals with normal renal function.
Severe renal impairment (eGFR <30 mL/minute per 1.73 m2): AUC and peak plasma concentration increased by approximately 66 and 20%, respectively, compared with that in individuals with normal renal function.
Patients with renal failure/end-stage renal disease: AUC increased by approximately 48% and peak plasma concentrations were similar compared with that in individuals with normal renal function.
Distribution
Plasma Protein Binding
86.2%
Elimination
Metabolism
Metabolized principally via glucuronidation by UGT isoenzymes 2B7, 1A3, 1A8, and 1A9.
Elimination Route
Following administration of radiolabeled dose of empagliflozin, eliminated in feces (41.2%) and urine (54.4%).
Half-life
Approximately 12.4 hours.
Special Populations
Apparent oral clearance of empagliflozin decreases with a reduction in eGFR. Fraction of empagliflozin excreted unchanged in urine and urinary glucose excretion decline with decrease in eGFR.
Gender, race, and body weight have no clinically meaningful effect on pharmacokinetics of empagliflozin.
Stability
Storage
Oral
Tablets
20-25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits SGLT2, the transporter principally responsible for reabsorption of glucose from the glomerular filtrate back into the circulation.
-
Reduces renal reabsorption of filtered glucose and lowers the renal threshold for glucose, thereby increasing urinary glucose excretion.
-
Increases glucose excretion independent of insulin secretion.
-
Reduces blood glucose concentrations.
Advice to Patients
-
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Medication Guide) before initiating therapy and each time the drug is dispensed.
-
When empagliflozin is used in fixed combination with other drugs, inform patients and/or caregivers of important cautionary information about the concomitant agent(s).
-
Inform patients and/or caregivers of the potential risks and benefits of empagliflozin and of alternative therapies.
-
Inform patients and/or caregivers that empagliflozin is not recommended in type 1 diabetes mellitus or diabetic ketoacidosis.
-
Advise patients and/or caregivers that the use of empagliflozin in combination with other antidiabetic agents (including insulin and insulin secretagogues) may increase risk of hypoglycemia. Inform pediatric patients and their caregivers that hypoglycemia may occur regardless of concomitant antidiabetic treatment. Educate patients and/or caregivers on the signs and symptoms of hypoglycemia.
-
Advise patients and/or caregivers that ketoacidosis, a potentially life-threatening condition, has been reported with empagliflozin therapy (sometimes associated with illness or surgery among other risk factors). Inform patients and/or caregivers that blood glucose can be normal in the presence of ketoacidosis. Advise patients and/or caregivers that they may be asked to monitor ketones. Educate patients and their caregivers of the risk factors and signs and symptoms of ketoacidosis (e.g., nausea, vomiting, abdominal pain, tiredness, labored breathing). If signs or symptoms of acidosis occur, instruct patients to discontinue empagliflozin and seek medical attention immediately.
-
Advise patients and/or caregivers that symptomatic hypotension may occur with empagliflozin and to report such symptoms to their clinicians. Inform patients that dehydration may increase the risk of hypotension and that patients should maintain adequate fluid intake. Inform patients and/or caregivers that renal function should be assessed prior to initiation of empagliflozin and monitored periodically thereafter.
-
Inform patients and/or caregivers of the potential for urinary tract infections, which may be serious, with empagliflozin therapy. Advise patients of the signs and symptoms of urinary tract infection (e.g., dysuria, cloudy urine, pelvic or back pain) and the need to contact a clinician if such signs and symptoms occur.
-
Inform patients and/or caregivers that necrotizing infections of the perineum (Fournier's gangrene) have occurred with empagliflozin therapy. Advise patients to seek prompt medical attention if they experience any symptoms of pain or tenderness, redness, or swelling of the genitals or the area from the genitals back to the rectum, occurring with a fever above 38°C or malaise.
-
Inform patients and/or caregivers that genital yeast infections (e.g., vulvovaginitis, balanitis, balanoposthitis) may occur. Inform female patients of the signs and symptoms of vaginal yeast infections (e.g., vaginal discharge, odor, itching) and male patients of the signs and symptoms of balanitis or balanoposthitis (e.g., rash or redness of the glans or foreskin of the penis, foul-smelling discharge from the penis, pain in skin around the penis). Advise patients of treatment options and when to seek medical advice.
-
Inform patients and/or caregivers about the importance of routine preventative foot care. Instruct patients and/or caregivers to monitor for new pain or tenderness, sores or ulcers, or infections involving the leg or foot and to seek medical advice immediately if such signs or symptoms develop.
-
Inform patients and/or caregivers that serious hypersensitivity reactions, such as urticaria and angioedema, have been reported with empagliflozin. Advise patients and/or caregivers to immediately report any skin reaction or angioedema and to discontinue empagliflozin until they have consulted a clinician.
-
Inform patients that due to the mechanism of action of empagliflozin, patients taking the drug will test positive for glucose in the urine. Advise patients and/or caregivers that urine glucose tests should not be used to monitor glycemic status while taking empagliflozin.
-
Advise patients and/or caregivers of the importance of adherence to dietary instructions, regular physical activity, periodic blood glucose monitoring and glycosylated hemoglobin (hemoglobin A1c; HbA1c) testing, recognition and management of hypoglycemia and hyperglycemia, and assessment of diabetes complications.
-
Advise patients and/or caregivers of the importance of seeking medical advice promptly during periods of stress such as fever, trauma, infection, or surgery as drug dosage requirements may change.
-
Inform female patients of reproductive potential of the potential risk to a fetus from empagliflozin. Instruct patients to notify their clinician if they are or plan to become pregnant. Inform female patients that breastfeeding is not recommended during treatment with empagliflozin.
-
Advise patients and/or caregivers to inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise patients and/or caregivers of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
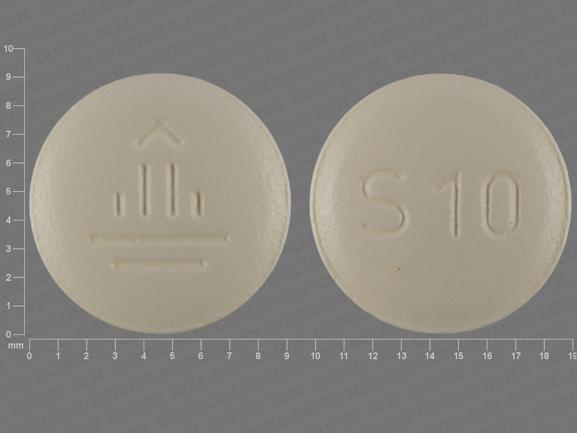
Tablets, film-coated |
10 mg |
Jardiance |
Boehringer Ingelheim |
|
25 mg |
Jardiance |
Boehringer Ingelheim |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release |
5 mg with Extended-release Metformin Hydrochloride 1 g |
Synjardy XR |
Boehringer Ingelheim |
|
5 mg with Linagliptin 2.5 mg and Extended-release Metformin Hydrochloride 1 g |
Trijardy XR |
Boehringer Ingelheim |
||
|
10 mg with Extended-release Metformin Hydrochloride 1 g |
Synjardy XR |
Boehringer Ingelheim |
||
|
10 mg with Linagliptin 5 mg and Extended-release Metformin Hydrochloride 1 g |
Trijardy XR |
Boehringer Ingelheim |
||
|
12.5 mg with Extended-release Metformin Hydrochloride 1 g |
Synjardy XR |
Boehringer Ingelheim |
||
|
12.5 mg with Linagliptin 2.5 mg and Extended-release Metformin Hydrochloride 1 g |
Trijardy XR |
Boehringer Ingelheim |
||
|
25 mg with Extended-release Metformin Hydrochloride 1 g |
Synjardy XR |
Boehringer Ingelheim |
||
|
25 mg with Linagliptin 5 mg and Extended-release Metformin Hydrochloride 1 g |
Trijardy XR |
Boehringer Ingelheim |
||
|
Tablets, film-coated |
5 mg with Metformin Hydrochloride 500 mg |
Synjardy |
Boehringer Ingelheim |
|
|
5 mg with Metformin Hydrochloride 1 g |
Synjardy |
Boehringer Ingelheim |
||
|
10 mg with Linagliptin 5 mg |
Glyxambi |
Boehringer Ingelheim |
||
|
12.5 mg with Metformin Hydrochloride 500 mg |
Synjardy |
Boehringer Ingelheim |
||
|
12.5 mg with Metformin Hydrochloride 1 g |
Synjardy |
Boehringer Ingelheim |
||
|
25 mg with Linagliptin 5 mg |
Glyxambi |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about empagliflozin
- Check interactions
- Compare alternatives
- Reviews (351)
- Side effects
- Dosage information
- During pregnancy
- Drug class: SGLT-2 inhibitors
- Breastfeeding
- En español