Zonisamide (Monograph)
Brand name: Zonegran
Drug class: Ion Channel Inhibition Agents
Introduction
Anticonvulsant; a sulfonamide.
Uses for Zonisamide
Seizure Disorders
Adjunctive therapy (i.e., in combination with other anticonvulsants) of partial seizures in adults with epilepsy.
Zonisamide Dosage and Administration
General
-
Do not discontinue abruptly; withdraw gradually to minimize potential for increased seizure frequency. (See Discontinuance of Therapy under Cautions.)
-
Closely monitor for marked changes in behavior that could indicate emergence or worsening of suicidal thoughts or behavior or depression. (See Suicidality Risk under Cautions.)
Administration
Oral Administration
Administer orally without regard to meals. Encourage patients to drink plenty of fluids while taking the drug to reduce the risk of kidney stones.
Administer initial dosage (100 mg daily) once daily; following dosage adjustment, administer once or twice daily.
Swallow capsules whole.
Dosage
Adults
Seizure Disorders
Partial Seizures
OralAdults >16 years of age: Initially, 100 mg daily.
After 2 weeks, may increase dosage to 200 mg daily for at least 2 weeks. May further increase to 300 and 400 mg daily; allow ≥2 weeks between dosage changes (to achieve steady state at each dosage level). Some clinicians may prefer to administer lower dosages for longer periods (in order to fully assess safety at steady state).
Dosages >400 mg daily may not be associated with increased therapeutic benefit.
Adverse effects occur more frequently at dosages ≥300 mg daily.
Special Populations
Hepatic Impairment
Titrate dosage slowly.
Renal Impairment
Titrate dosage slowly. Do not use in patients with renal failure (GFR <50 mL/minute).
Geriatric Patients
No specific dosage recommendations; however, select dosage cautiously, usually starting at the lower end of the dosage range, because of age-related decreases in hepatic, renal, or cardiac function and concomitant diseases and drug therapy.
Cautions for Zonisamide
Contraindications
-
Known hypersensitivity to zonisamide, sulfonamides, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Hematologic Effects
Aplastic anemia and agranulocytosis reported rarely; relationship between these events and dosage or duration of therapy not established.
Oligohidrosis and Hyperthermia
Oligohidrosis (a reduction in sweating) and hyperthermia reported, particularly in pediatric patients. Closely monitor patients for evidence of decreased sweating and increased body temperature, particularly in warm or hot weather.
Consider risk of hyperthermia when zonisamide is used concomitantly with other drugs that predispose patients to heat-related disorders. (See Pediatric Use under Cautions, Drugs Predisposing to Heat-related Disorders under Interactions, and Advice to Patients.)
Suicidality Risk
Increased risk of suicidality (suicidal ideation or behavior) observed in an analysis of studies using various anticonvulsants, including zonisamide, in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.
Balance risk of suicidality with the risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerge during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself. (See Advice to Patients.)
Metabolic Acidosis
Hyperchloremic, non-anion gap, metabolic acidosis reported. (See Pediatric Use under Cautions.) Manifestations may include hyperventilation, fatigue, anorexia, cardiac arrhythmias, or stupor. Generally occurs early in treatment, but may occur at any time during therapy.
Risk appears greater at higher dosages of zonisamide, but can occur with dosages ≤25 mg daily. Renal disease, severe respiratory disorders, status epilepticus, diarrhea, surgery, ketogenic diets, or other drugs (e.g., acetazolamide) may predispose patients to acidosis. Also appears to be more frequent and severe in pediatric patients. (See Pediatric Use under Cautions.)
Potential for serious sequelae (e.g., nephrolithiasis, nephrocalcinosis, osteomalacia and/or osteoporosis with increased risk for fractures) from chronic, untreated metabolic acidosis.
Measure serum bicarbonate concentrations prior to and periodically during therapy. If metabolic acidosis develops and persists, consider reducing dosage or discontinuing therapy (by gradually tapering dosage) and modifying the patient’s anticonvulsant drug regimen as appropriate. If therapy is continued, consider alkali treatment.
Discontinuance of Therapy
Abrupt withdrawal may result in increased seizure frequency or status epilepticus; withdraw zonisamide gradually and reduce dosage slowly.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. (See Pregnancy under Cautions.) Teratogenic effects and embryolethality observed in animal studies. Fetal abnormalities included cardiovascular, skeletal, and craniofacial malformations, and fetal growth retardation.
Cognitive/Neuropsychiatric Effects
Possible somnolence or fatigue, psychiatric symptoms (e.g., depression, psychosis), and impaired psychomotor or cognitive performance (e.g., difficulties in concentrating, language, speech, and word finding). (See Suicidality Risk under Cautions.)
Sensitivity Reactions
Dermatologic and Sensitivity Reactions
Zonisamide is a sulfonamide; potentially fatal reactions may occur as a result of severe reactions to sulfonamides, including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias.
Rash (usually occurring early in treatment and not dose related) reported in clinical studies. At least 49 cases of severe rash (Stevens-Johnson syndrome or toxic epidermal necrolysis) reported during postmarketing experience in Japan; no confirmed cases reported to date in US.
Discontinue immediately if signs or symptoms of hypersensitivity occur. Consider drug discontinuance if unexplained rash occurs; if drug is continued, observe patient frequently.
Multi-organ Hypersensitivity
Multi-organ hypersensitivity (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) reported; can be fatal or life-threatening. Clinical presentation is variable but typically includes fever, rash, lymphadenopathy, and/or facial swelling associated with other organ system involvement (e.g., eosinophilia, hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).
If manifestations of multi-organ hypersensitivity occur, evaluate patient immediately. If an alternative cause cannot be identified, discontinue zonisamide.
General Precautions
Renal Calculi
Clinically possible or confirmed renal calculi (kidney stones), composed of calcium or urate salts, reported.
In general, increasing fluid intake and urine output may reduce the risk of kidney stone formation, particularly in patients with predisposing risk factors; not known whether these measures reduce the risk of kidney stone formation in patients receiving zonisamide.
Other Renal Effects
Substantial increases in Scr and BUN reported; such increases appeared to persist over time but were not progressive. Consider periodically monitoring renal function during zonisamide therapy.
Discontinue use in patients who develop acute renal failure or clinically important, sustained increases in Scr and BUN.
Status Epilepticus
In controlled studies, status epilepticus occurred in 1.1 or 0% of patients receiving zonisamide or placebo, respectively. In all (uncontrolled and controlled) clinical studies, the incidence of status epilepticus in patients receiving zonisamide was 1%.
Specific Populations
Pregnancy
Risk of fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
North American Antiepileptic Drug (NAAED) Pregnancy Registry (for patients) at 888-233-2334 or [Web].
If zonisamide-induced metabolic acidosis occurs during pregnancy, may affect fetal development (i.e., decreased fetal growth, decreased fetal oxygenation, fetal death) and the ability of the fetus to tolerate labor. In pregnant women, monitor and treat metabolic acidosis in the same manner as nonpregnant patients. In addition, monitor neonates for metabolic acidosis because of possible fetal drug transfer and transient metabolic acidosis following birth.
Some clinicians recommend closely monitoring zonisamide concentrations and adjusting zonisamide dosage as necessary in pregnant women.
Lactation
Distributes into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <16 years of age. However, the drug has been used in some pediatric patients† [off-label] for the treatment of epilepsy.
Studies conducted with pediatric patients indicate that frequency of some adverse effects (e.g., metabolic acidosis, oligohidrosis and hyperthermia) may be increased compared with adults.
Oligohidrosis and hyperthermia reported in pediatric patients (1.6–17 years of age) and sometimes have resulted in heat stroke and hospitalization. (See Oligohidrosis and Hyperthermia under Cautions.)
If used in pediatric patients (not an FDA-labeled population), closely monitor for evidence of decreased sweating and increased body temperature, especially in warm or hot weather or when other drugs that predispose patients to heat-related disorders (e.g., carbonic anhydrase inhibitors) are used concomitantly. (See Drugs Predisposing to Heat-related Disorders under Interactions.)
Pediatric patients may be at increased risk for zonisamide-induced metabolic acidosis; may be more severe in younger patients. Specific effects of zonisamide on growth and bone not studied; chronic metabolic acidosis may reduce growth rates in pediatric patients, resulting in a reduction in the maximal height achieved. (See Metabolic Acidosis under Cautions, Specific Drugs under Interactions, and Advice to Patients.)
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.
Hepatic Impairment
Use with caution in patients with hepatic impairment; slower dosage titration and more frequent monitoring may be necessary.
Renal Impairment
Use with caution in patients with renal impairment; slower dosage titration and more frequent monitoring may be necessary.
Because of insufficient experience concerning dosage and toxicity, do not use in patients with renal failure (GFR <50 mL/minute).
Common Adverse Effects
Abdominal pain, anorexia, diarrhea, nausea, dyspepsia, constipation, dry mouth, taste perversion, headache, dizziness, ataxia, nystagmus, paresthesia, confusion, difficulty concentrating, impaired memory, mental slowing, speech abnormalities, difficulty in verbal expression, agitation and/or irritability, depression, insomnia, anxiety, nervousness, schizophrenic and/or schizophreniform behavior, somnolence, fatigue, tiredness, flu-like syndrome, ecchymosis, rhinitis, weight loss, rash, diplopia.
Drug Interactions
Metabolized by CYP3A4. Does not appear to substantially inhibit CYP1A2, 2A6, 2C9, 2C19, 2D6, 2E1, 3A4, 2B6, or 2C8 in vitro.
Weak inhibitor of P-glycoprotein (P-gp) in vitro.
Drugs Metabolized by or Affecting Hepatic Microsomal Enzymes
CYP3A4 inhibitors: Pharmacokinetics of zonisamide may be altered, but not expected to be clinically important; dosage adjustment not necessary.
CYP3A4 inducers: Zonisamide concentrations may be altered when CYP3A4-inducing drugs are introduced or withdrawn from therapy, or dosage is adjusted. Closely monitor patients and adjust dosage of zonisamide as necessary.
CYP substrates: Pharmacokinetic interactions not expected.
Drugs Affected by P-Glycoprotein
May potentially affect the pharmacokinetics of P-gp substrates.
Drugs Affected by UGT Enzymes
Not expected to interact with drugs metabolized by UGT enzymes.
Drugs Predisposing to Heat-related Disorders
Increased risk of oligohidrosis and hyperthermia with drugs that predispose to heat-related disorders.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticholinergic agents |
Increased risk of oligohidrosis and hyperthermia |
|
|
Carbamazepine |
Clinically important changes in plasma zonisamide concentrations may occur when carbamazepine is introduced or withdrawn, or dosage adjusted; no change in steady-state plasma carbamazepine concentrations |
Closely monitor patient; dosage adjustment of zonisamide may be required |
|
Carbonic anhydrase inhibitors (e.g., acetazolamide, dichlorphenamide, topiramate) |
Possible increased risk of metabolic acidosis and kidney stone formation Increased risk of oligohidrosis and hyperthermia |
Monitor for onset or worsening of metabolic acidosis |
|
Cimetidine |
Clinically important changes in zonisamide pharmacokinetics not observed |
Dosage adjustment not necessary |
|
CNS depressants (including alcohol) |
Potential for additive CNS effects (e.g., somnolence, fatigue) |
Use concomitantly with caution |
|
Desipramine |
Pharmacokinetics of desipramine not substantially altered |
|
|
Digoxin |
Pharmacokinetics of digoxin may be altered |
|
|
Ketoconazole |
Clinically important changes in zonisamide pharmacokinetics not observed |
Dosage adjustment not necessary |
|
Lamotrigine |
No change in steady-state plasma concentrations of lamotrigine |
|
|
Oral contraceptives |
Pharmacokinetic interaction unlikely Oral contraceptive containing ethinyl estradiol and norethisterone: No changes in concentrations of either contraceptive component |
|
|
Phenobarbital |
Clinically important changes in plasma zonisamide concentrations may occur when phenobarbital is introduced or withdrawn, or dosage adjusted |
Closely monitor patient; dosage adjustment of zonisamide may be required |
|
Phenytoin |
Clinically important changes in plasma zonisamide concentrations may occur when phenytoin is introduced or withdrawn, or dosage adjusted; no change in steady-state plasma phenytoin concentrations |
Closely monitor patient; dosage adjustment of zonisamide may be required |
|
Quinidine |
Pharmacokinetics of quinidine may be altered |
|
|
Rifampin |
Clinically important changes in plasma zonisamide concentrations may occur when rifampin is introduced or withdrawn, or dosage adjusted |
Closely monitor patient; dosage adjustment of zonisamide may be required |
|
Valproic acid |
No change in steady-state plasma concentrations of valproic acid |
Zonisamide Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed following oral administration, with nearly 100% oral bioavailability. Peak plasma concentrations attained within 2–6 hours after oral administration.
Food
Food delays the time to peak plasma concentration but does not affect bioavailability.
Distribution
Extent
Extensively binds to erythrocytes, resulting in an 8-fold higher concentration of zonisamide in erythrocytes than in plasma.
Crosses the placenta; distributed into breast milk.
Plasma Protein Binding
Approximately 40%.
Elimination
Metabolism
Undergoes acetylation to form N-acetyl zonisamide, subsequent reduction to form 2-sulfamoylacetyl phenol, and further glucuronide conjugation. The reduction of N-acetyl zonisamide is mediated by CYP3A4.
Does not induce own metabolism.
Elimination Route
Excreted principally in urine as unchanged drug and a glucuronide metabolite.
Half-life
About 63 hours.
Special Populations
In patients with marked renal impairment (Clcr≤ 20 mL/minute), AUC was increased by 35%. Renal clearance decreases with decreasing renal function.
In patients with hepatic impairment, pharmacokinetics not studied to date.
Clearance of zonisamide may be increased at the end of the second trimester in pregnant women.
Pharmacokinetics were similar in geriatric and young healthy volunteers in single-dose studies. (See Geriatric Patients under Dosage and Administration.)
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C); protect from moisture and light.
Actions
-
Exact mechanism of action is not known; anticonvulsant activity may be associated with the drug’s sodium- and calcium-channel blocking activities.
-
May potentiate dopaminergic and serotonergic neurotransmission but does not appear to potentiate the synaptic activity of GABA.
-
Exhibits weak inhibition of carbonic anhydrase activity; not thought to contribute substantially to anticonvulsant activity.
Advice to Patients
-
Importance of instructing patients to read the patient information (medication guide) prior to initiating zonisamide therapy.
-
Importance of patients taking zonisamide exactly as prescribed.
-
Risk of serious skin rash that can cause death; these skin reactions are more likely to happen within the first 4 months of starting therapy, but may occur later. Importance of immediately contacting clinician if skin rash occurs.
-
Importance of patients being aware that zonisamide can prevent sweating, which makes it harder for the body to cool down when it gets very hot; this is more likely to occur in warmer weather, in children, and during physical exercise. Importance of avoiding exposure to heat, maintaining adequate hydration, and informing clinicians immediately if fever or increased body temperature and/or decreased sweating occurs, particularly in children or in hot weather.
-
Risk of blood cell abnormalities such as reduced RBC and WBC counts. Importance of contacting clinician if fever, sore throat, sores in the mouth, or unusual bruising occurs.
-
Risk of suicidality (anticonvulsants, including zonisamide, may increase risk of suicidal thoughts or actions in about 1 in 500 people). Importance of patients, family, and caregivers being alert to day-to-day changes in mood, behavior, and actions and immediately informing clinician of any new or worrisome behaviors (e.g., talking or thinking about wanting to hurt oneself or end one’s life, withdrawing from friends and family, becoming depressed or experiencing worsening of existing depression, becoming preoccupied with death and dying, giving away prized possessions).
-
Importance of advising patients that zonisamide may cause metabolic acidosis and that blood tests to measure serum bicarbonate concentrations may be performed. Patients should contact their clinician immediately if they develop symptoms of metabolic acidosis such as fast breathing (hyperventilation), fatigue, loss of appetite, irregular heart beat, palpitations, or unconsciousness.
-
Potential for drowsiness, especially at higher dosages. Importance of advising patients to avoid driving or operating complex machinery until experience with the drug’s effects has been established. Because of the potential for additive CNS effects, patients should be advised to use caution when consuming alcohol or taking concomitant CNS depressants.
-
Risk of kidney stones. Importance of informing patients that increasing fluid intake (i.e., by drinking 6–8 glasses of water a day) and urine output may reduce the risk of stone formation, particularly in those with predisposing factors. Importance of immediately reporting symptoms of kidney stones (e.g., sudden back pain, abdominal pain, and/or blood in urine) to clinician.
-
Importance of immediately reporting worsening of seizures and severe muscle pain and/or weakness to clinician.
-
Importance of women informing clinicians if they are or plan to become pregnant. Importance of informing women who are or plan to become pregnant that zonisamide may cause metabolic acidosis, which may negatively affect fetal development during pregnancy. Importance of clinicians informing women about the existence of and encouraging enrollment in pregnancy registries (see Pregnancy under Cautions).
-
Importance of informing nursing women and those who plan to breast-feed that zonisamide can appear in the breast milk, and that the effects of this exposure on the infant are unknown. Importance of women informing clinicians if they plan to breast-feed.
-
Importance of swallowing zonisamide capsules whole and not biting into or breaking into the capsules; zonisamide may be taken with or without food.
-
Importance of informing patients not to stop taking zonisamide without talking to their clinician since stopping the drug suddenly can cause serious problems, including seizures.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription drugs, OTC drugs, and special diets (e.g., ketogenic diet), as well as any concomitant illnesses (e.g., liver disease, kidney disease, severe lung disorders, diarrhea, surgery, depression, bipolar disorder) or family history of suicidality or bipolar disorder.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
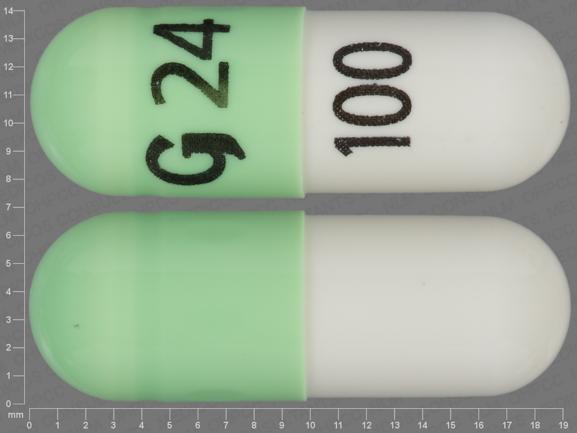
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
25 mg* |
Zonegran |
Eisai |
|
Zonisamide Capsules |
||||
|
50 mg* |
Zonisamide Capsules |
|||
|
100 mg* |
Zonegran |
Eisai |
||
|
Zonisamide Capsules |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about zonisamide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (146)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: carbonic anhydrase inhibitor anticonvulsants
- Breastfeeding
- En español