Vortioxetine (Monograph)
Brand name: Trintellix
Drug class: Serotonin Modulators
- Selective Serotonin-reuptake Inhibitors
- Serotonin-reuptake Inhibitors
- Serotonin 5-HT1A Receptor Agonists
- Serotonin 5-HT3 Receptor Antagonists
VA class: CN609
Chemical name: 1-[2-[(2,4-Dimethylphenyl)thio]phenyl]-piperazine
Molecular formula: C18H22N2SC18H22N2S•HBr
CAS number: 508233-74-7
Warning
- Suicidality
-
Antidepressants increased risk of suicidal thinking and behavior (suicidality) compared with placebo in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need. Vortioxetine has not been evaluated for use in pediatric patients. (See Pediatric Use under Cautions.)
-
In pooled data analyses, risk of suicidality was not increased in adults >24 years of age and apparently was reduced in adults ≥65 years of age with antidepressant therapy compared with placebo.
-
Depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide.
-
Appropriately monitor and closely observe all patients who are started on vortioxetine therapy for clinical worsening, suicidality, or unusual changes in behavior; involve family members and/or caregivers in this process. (See Worsening of Depression and Suicidality Risk under Cautions.)
Introduction
Antidepressant; serotonin-reuptake inhibitor with several other activities, including 5-HT3 receptor antagonism and 5-HT1A receptor agonism.
Uses for Vortioxetine
Major Depressive Disorder
Treatment of major depressive disorder in adults.
APA states that effectiveness of antidepressants is generally comparable between and within classes of medications, including SSRIs, SNRIs, tricyclic antidepressants (TCAs), MAO inhibitors, and other antidepressants (e.g., bupropion, mirtazapine, trazodone). Choose antidepressant based mainly on the following factors: patient preference; nature of prior response to medication; safety, tolerability, and anticipated adverse effects; concurrent psychiatric and medical conditions; specific properties of the medication (e.g., half-life, actions on CYP isoenzymes, other drug interactions); and cost. For most patients, an SSRI, SNRI, mirtazapine, or bupropion is considered optimal. Consult APA’s Practice Guidelines for the Treatment of Patients with Major Depressive Disorder (at [Web]) for additional information.
Vortioxetine Dosage and Administration
General
-
Allow at least 2 weeks to elapse between discontinuance of an MAO inhibitor intended to treat psychiatric disorders and initiation of vortioxetine and allow at least 3 weeks to elapse between discontinuance of vortioxetine and initiation of MAO inhibitor therapy intended to treat psychiatric disorders. (See Contraindications and Serotonin Syndrome under Cautions and also see Specific Drugs under Interactions.)
-
Monitor for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustments. (See Worsening of Depression and Suicidality Risk under Cautions.)
-
Although vortioxetine can be abruptly discontinued, transient adverse reactions (including headache, muscle tension, mood swings, sudden outbursts of anger, dizziness, runny nose) reported in the first week following abrupt discontinuance of dosages of 15 or 20 mg daily. Manufacturer recommends decreasing dosage to 10 mg daily for one week before full discontinuance in patients receiving 15 or 20 mg of the drug daily, if possible.
Administration
Oral Administration
Administer orally once daily, without regard to meals, at approximately the same time each day.
Use caution in prescribing and dispensing due to similarities in spelling and pronunciation of Brintellix (former trade name for vortioxetine; changed to Trintellix in May 2016) and Brilinta (ticagrelor). (See Prescribing and Dispensing Precautions under Cautions.)
Dosage
Available as vortioxetine hydrobromide; dosage expressed in terms of vortioxetine.
Adults
Major Depressive Disorder
Oral
Initially, 10 mg once daily. Increase dosage to 20 mg daily, as tolerated, since higher dosages demonstrated better efficacy in US clinical trials. In the main clinical trials, dosage increases were made after the first week of therapy. Efficacy and safety of dosages >20 mg daily not evaluated in controlled trials. Consider decreasing dosage to 5 mg once daily in patients who do not tolerate higher dosages.
In poor metabolizers of CYP2D6, maximum recommended dosage is 10 mg once daily.
If used with a potent CYP2D6 inhibitor, a 50% reduction in vortioxetine dosage is required. If used with a potent CYP inducer for >14 days, consider increasing dosage of vortioxetine. (See Interactions.)
Optimum duration not established; may require several months or longer of sustained antidepressant therapy.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment: Dosage adjustment not necessary.
Severe hepatic impairment: Not studied; use not recommended.
Renal Impairment
Dosage adjustment not necessary in patients with renal impairment (ranging from mild impairment to end-stage renal disease). (See Renal Impairment under Cautions.)
Geriatric Patients
Dosage adjustment not necessary.
Gender
Dosage adjustment based on gender not necessary.
Race or Ethnicity
Dosage adjustment based on race or ethnicity not necessary.
Cautions for Vortioxetine
Contraindications
-
Known hypersensitivity to vortioxetine or any ingredients in the formulation. Angioedema reported in vortioxetine-treated patients.
-
Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor intended to treat psychiatric disorders. Use of an MAO inhibitor intended to treat psychiatric disorders within 3 weeks of vortioxetine discontinuance. (See Serotonin Syndrome under Cautions and also see Specific Drugs under Interactions.)
-
Initiation of vortioxetine in patients receiving MAO inhibitors such as linezolid or IV methylene blue. (See Specific Drugs under Interactions.)
Warnings/Precautions
Warnings
Worsening of Depression and Suicidality Risk
Possible worsening of depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior in both adult and pediatric patients with major depressive disorder, whether or not they are taking antidepressants; may persist until clinically important remission occurs. (See Boxed Warning and also see Pediatric Use under Cautions.) However, suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide.
Appropriately monitor and closely observe patients receiving vortioxetine for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments.
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania may be precursors to emerging suicidality. Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
Other Warnings and Precautions
Serotonin Syndrome
Potentially life-threatening serotonin syndrome reported with serotonergic antidepressants, including vortioxetine, when used alone, but particularly during concurrent therapy with other serotonergic drugs (e.g., 5-HT1 receptor agonists [triptans], TCAs, buspirone, fentanyl, lithium, tramadol, tryptophan, St. John’s wort [Hypericum perforatum]) and with drugs that impair the metabolism of serotonin (particularly MAO inhibitors, both those used to treat psychiatric disorders and others, such as linezolid and methylene blue). (See Contraindications under Cautions and also see Interactions.)
Symptoms of serotonin syndrome may include mental status changes (e.g., agitation, hallucinations, delirium, coma), autonomic instability (e.g., tachycardia, labile BP, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or GI symptoms (e.g., nausea, vomiting, diarrhea).
Concurrent or recent (i.e., within 2 weeks) therapy with MAO inhibitors intended to treat psychiatric disorders is contraindicated. Use of an MAO inhibitor intended to treat psychiatric disorders within 3 weeks of vortioxetine discontinuance also contraindicated. Do not initiate vortioxetine in patients treated with other MAO inhibitors such as linezolid or IV methylene blue. (See Specific Drugs under Interactions.)
If concurrent therapy with other serotonergic drugs is clinically warranted, advise patient of potentially increased risk for serotonin syndrome, particularly during initiation of therapy and dosage increases.
Monitor patients receiving vortioxetine for the development of serotonin syndrome. If manifestations occur, immediately discontinue vortioxetine and any concurrently administered serotonergic agents and initiate supportive and symptomatic treatment.
Abnormal Bleeding
Possible increased risk of bleeding with serotonergic antidepressants, including vortioxetine; events ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages. Concurrent use of aspirin, NSAIAs, warfarin, or other anticoagulants may increase risk. (See Specific Drugs under Interactions and also see Advice to Patients.)
Activation of Mania/Hypomania
Possible activation of mania and hypomania; use with caution in patients with personal or family history of bipolar disorder, mania, or hypomania.
Angle-closure Glaucoma
Pupillary dilation (mydriasis) occurs with many antidepressants, including vortioxetine, and may trigger an acute attack of angle-closure glaucoma (narrow-angle glaucoma) in patients with anatomically narrow angles who do not have a patent iridectomy. (See Advice to Patients.)
Hyponatremia/SIADH
Treatment with serotonergic drugs, including vortioxetine, may result in hyponatremia; in many cases, SIADH is apparent cause. Increased risk in patients who are volume-depleted, elderly, or taking diuretics. Initiate appropriate medical intervention and consider drug discontinuance in patients with symptomatic hyponatremia.
Prescribing and Dispensing Precautions
Ensure accuracy of prescription; similarity in spelling and pronunciation of Brintellix (former trade name of vortioxetine; changed to Trintellix in May 2016) and Brilinta (ticagrelor, a platelet-aggregation inhibitor) may result in medication errors.
Specific Populations
Pregnancy
Category C.
Possible complications, sometimes severe and requiring prolonged hospitalization, respiratory support, enteral nutrition, and other forms of supportive care, in neonates exposed to SSRIs or SNRIs late in the third trimester; may arise immediately upon delivery.
Consult joint APA and ACOG guidelines (at [Web]) for additional information on management of depression in women prior to conception and during pregnancy, including treatment algorithms.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and effectiveness not established in pediatric patients; not studied in such patients.
FDA warns that a greater risk of suicidal thinking or behavior (suicidality) occurred during the first few months of antidepressant treatment compared with placebo in children and adolescents with major depressive disorder, obsessive-compulsive disorder (OCD), or other psychiatric disorders based on pooled analyses of 24 short-term, placebo-controlled trials of 9 antidepressant drugs (SSRIs and other antidepressants). However, a later meta-analysis of 27 placebo-controlled trials of 9 antidepressants (SSRIs and others) in patients <19 years of age with major depressive disorder, OCD, or non-OCD anxiety disorders suggests that the benefits of antidepressant therapy in treating these conditions may outweigh the risks of suicidal behavior or ideation. No suicides occurred in these pediatric trials.
Carefully consider these findings when assessing potential benefits and risks of vortioxetine in a child or adolescent for any clinical use. (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Geriatric Use
In clinical trials with vortioxetine, 11% of patients were ≥65 years of age, including those in a placebo-controlled study conducted specifically in geriatric patients. No overall differences in safety or effectiveness observed between geriatric and younger adults in these studies; other reported clinical experience has not identified any differences in response to vortioxetine between geriatric and younger adults. (See Geriatric Patients under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Serotonergic antidepressants, including vortioxetine, associated with clinically important hyponatremia in geriatric patients, who may be at greater risk for this adverse effect. (See Hyponatremia/SIADH under Cautions.)
In pooled data analyses, a reduced risk of suicidality was observed in adults ≥65 years of age with antidepressant therapy compared with placebo. (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Hepatic Impairment
No dosage adjustment required in patients with mild or moderate hepatic impairment. Not studied in patients with severe hepatic impairment; use not recommended in such patients.
Renal Impairment
No dosage adjustment is necessary in patients with mild, moderate, or severe renal impairment or end-stage renal disease. (See Special Populations under Pharmacokinetics.)
Common Adverse Effects
Nausea, constipation, vomiting. Nausea is the most common adverse effect and occurs most often during the first week of treatment; incidence is dose related and higher in females than males.
Drug Interactions
Metabolized principally by CYP2D6 with lesser contributions from CYP isoenzymes 3A4/5, 2C19, 2C9, 2A6, 2C8, and 2B6. Unlikely to inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or CYP3A4/5. In vitro, did not induce CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, or 3A4/5.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP2D6 inhibitors: Reduce vortioxetine dosage by 50% during concurrent use. Increase vortioxetine dosage back to the original dosage when the CYP2D6 inhibitor is discontinued.
Potent CYP inducers: When vortioxetine is administered with a potent CYP inducer for >14 days, consider increasing vortioxetine dosage; maximum dosage of vortioxetine should not exceed 3 times the original dosage. Resume original vortioxetine dosage within 14 days following discontinuance of the potent CYP inducer.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5: Clinically important pharmacokinetic interaction unlikely; dosage adjustment of the concurrently administered drug not necessary.
Substrates of CYP2E1: Clinically important pharmacokinetic interaction unlikely.
Drugs Affecting or Affected by P-glycoprotein Transport
Vortioxetine is a poor P-glycoprotein (P-gp) substrate and inhibitor. Dosage adjustment not necessary when a P-gp substrate is concurrently administered.
Drugs Highly Bound to Plasma Protein
Potential pharmacokinetic interaction (possible increased free concentrations of other highly protein bound drugs if used concurrently with vortioxetine).
Drugs Associated with Serotonin Syndrome
Potentially serious, sometimes fatal serotonin syndrome with other serotonergic drugs. If concomitant use of other serotonergic drugs with vortioxetine is clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases.
If serotonin syndrome occurs, immediately discontinue vortioxetine and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment. (See Serotonin Syndrome under Cautions.)
Drugs Affecting Hemostasis
Potential increased risk of bleeding if used concurrently with drugs that affect coagulation or bleeding; use with caution. (See Abnormal Bleeding under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Vortioxetine (20- or 40-mg single dose) did not increase impairment of mental and motor skills caused by alcohol |
Avoid alcohol use during vortioxetine therapy |
|
Anticoagulants (e.g., warfarin) |
Potential increased risk of bleeding Warfarin: No clinically important effect on INR, prothrombin values, or warfarin pharmacokinetics following concurrent administration of stable doses of warfarin with multiple daily doses of vortioxetine |
Carefully monitor patients receiving anticoagulants during initiation and discontinuance of vortioxetine Warfarin: Dosage adjustment not necessary |
|
Antidepressants, SSRIs (e.g., citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) or SNRIs (e.g., desvenlafaxine, duloxetine, levomilnacipran, milnacipran, venlafaxine) |
Potentially life-threatening serotonin syndrome Duloxetine (CYP1A2 substrate): Clinically important pharmacokinetic interaction unlikely Fluoxetine and paroxetine (potent CYP2D6 inhibitors): Potential pharmacokinetic interaction (increased plasma vortioxetine concentrations) |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, the SSRI or SNRI, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment Duloxetine: Dosage adjustment of duloxetine not necessary Fluoxetine and paroxetine: Reduce vortioxetine dosage by 50% during concurrent use; increase vortioxetine dosage back to original dosage when fluoxetine or paroxetine is discontinued Venlafaxine: Dosage adjustment of venlafaxine not necessary |
|
Antidepressants, tricyclics (TCAs) |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, the TCA, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Aspirin |
Potential increased risk of bleeding Concomitant administration of aspirin (150 mg daily) with multiple doses of vortioxetine did not have a clinically important effect on platelet aggregation or pharmacokinetics of aspirin and salicylic acid |
Carefully monitor patients receiving aspirin during initiation and discontinuance of vortioxetine Dosage adjustment of aspirin not necessary |
|
Budesonide |
Clinically important pharmacokinetic interaction unlikely |
Budesonide dosage adjustment not necessary |
|
Bupropion |
Concurrent administration of vortioxetine and bupropion increased bupropion peak plasma concentrations by 18%, and increased vortioxetine peak plasma concentrations and AUC by 114 and 128%, respectively Risk of increased adverse effects |
Reduce vortioxetine dosage by 50% during concurrent use; increase vortioxetine dosage back to original dosage when bupropion is discontinued Bupropion dosage adjustment not necessary |
|
Buspirone |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, buspirone, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Caffeine |
Multiple-dose vortioxetine did not have a clinically important effect on pharmacokinetics of caffeine (a CYP1A2 substrate) |
|
|
Carbamazepine |
Potential pharmacokinetic interaction (decreased vortioxetine concentrations) |
Consider increasing vortioxetine dosage when concomitantly administered with carbamazepine for >14 days; maximum dosage of vortioxetine should not exceed 3 times the original dosage Following discontinuance of carbamazepine, resume original vortioxetine dosage within 14 days |
|
Diazepam |
Multiple daily doses of vortioxetine did not affect pharmacokinetics or pharmacodynamics (i.e., composite cognitive score) of diazepam (a CYP2C19 substrate) |
Diazepam dosage adjustment not necessary |
|
Digoxin |
Clinically important pharmacokinetic interaction unlikely |
Digoxin dosage adjustment not necessary |
|
Diuretics |
Possible increased risk of hyponatremia |
|
|
Fentanyl |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, fentanyl, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Fluconazole |
Administration of a single dose of vortioxetine (10 mg) with fluconazole (200 mg once daily) increased peak plasma concentrations and AUC of vortioxetine by 15 and 46%, respectively; not considered clinically important |
Fluconazole dosage adjustment not necessary |
|
5-HT1 receptor agonists (triptans; e.g., almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan, zolmitriptan) |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, the triptan, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Ketoconazole |
Administration of a single dose of vortioxetine (10 mg) with ketoconazole (400 mg once daily) increased peak plasma concentrations and AUC of vortioxetine by 26 and 30%, respectively; not considered clinically important |
Ketoconazole dosage adjustment not necessary |
|
Linezolid |
Potentially life-threatening serotonin syndrome |
Do not use concurrently; consider availability of alternative anti-infectives and weigh benefit of linezolid against the risk of serotonin syndrome If emergency use of linezolid is considered necessary, immediately discontinue vortioxetine; monitor for symptoms of CNS toxicity for 3 weeks or until 24 hours after the last linezolid dose, whichever comes first May resume vortioxetine 24 hours after last linezolid dose If nonemergency use of linezolid is planned, withhold vortioxetine for at least 2 weeks prior to initiating linezolid Do not initiate vortioxetine in patients receiving linezolid If urgent treatment of a psychiatric condition is necessary, consider other interventions, including hospitalization; may initiate vortioxetine 24 hours after last linezolid dose |
|
Lithium |
Potentially life-threatening serotonin syndrome Multiple-dose vortioxetine did not have a clinically important effect on steady-state lithium exposure |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, lithium, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment Lithium dosage adjustment not necessary |
|
MAO inhibitors |
Potentially life-threatening serotonin syndrome |
Concomitant use is contraindicated Allow at least 2 weeks between discontinuance of an MAO inhibitor intended to treat psychiatric disorders and initiation of vortioxetine and at least 3 weeks between discontinuance of vortioxetine and initiation of MAO inhibitor therapy |
|
Methylene blue |
Potentially life-threatening serotonin syndrome Most cases occurred when methylene blue was used as a diagnostic (visualizing) dye† [off-label] (1–8 mg/kg IV) during parathyroid surgery; unclear whether there is a risk of serotonin syndrome when methylene blue is administered by other routes or in lower IV doses in patients receiving serotonergic drugs |
Generally should not use methylene blue in patients receiving vortioxetine; consider availability of alternative interventions and weigh benefits of IV methylene blue against risk of serotonin syndrome If emergency use of IV methylene blue is considered necessary, immediately discontinue vortioxetine and monitor for symptoms of CNS toxicity for 3 weeks or until 24 hours after last methylene blue dose, whichever comes first May resume vortioxetine 24 hours after last dose of IV methylene blue If nonemergency use of methylene blue is planned, withhold vortioxetine for at least 2 weeks prior to initiating methylene blue Do not initiate vortioxetine in patients receiving IV methylene blue If urgent treatment of a psychiatric condition is necessary, consider other interventions, including hospitalization; may initiate vortioxetine 24 hours after last IV methylene blue dose |
|
Midazolam |
Multiple-dose vortioxetine did not have a clinically important effect on the pharmacokinetics of midazolam (a CYP3A4 substrate) |
|
|
NSAIAs |
Potential increased risk of bleeding (see Aspirin) |
Carefully monitor patients receiving NSAIAs during initiation and discontinuance of vortioxetine |
|
Omeprazole |
Concomitant administration of single-dose omeprazole (40 mg) and vortioxetine (10 mg once daily) did not have a clinically important effect on the pharmacokinetics of either drug |
|
|
Oral contraceptives |
Vortioxetine (10 mg once daily) did not have a clinically important effect on the pharmacokinetics of concurrently administered ethinyl estradiol (0.03 mg) or levonorgestrel (0.15 mg). |
|
|
Phenytoin |
Potential pharmacokinetic interaction (decreased vortioxetine concentrations) |
Consider increasing vortioxetine dosage when concomitantly administered with phenytoin for >14 days; maximum dosage of vortioxetine should not exceed 3 times the original dosage Following discontinuance of phenytoin, resume original vortioxetine dosage within 14 days |
|
Quinidine |
Potential pharmacokinetic interaction (increased plasma vortioxetine concentrations) |
Reduce vortioxetine dosage by 50% when administered concomitantly with quinidine; following discontinuance of quinidine, resume original vortioxetine dosage |
|
Repaglinide |
Clinically important pharmacokinetic interaction unlikely |
Repaglinide dosage adjustment not necessary |
|
Rifampin |
Concurrent administration of a single dose of vortioxetine (20 mg) with multiple-dose rifampin decreased peak concentrations and AUC of vortioxetine by 51 and 72–77%, respectively |
Consider increasing vortioxetine dosage when concomitantly administered with rifampin for >14 days; maximum dosage of vortioxetine should not exceed 3 times the original dosage Following discontinuance of rifampin, resume original vortioxetine dosage within 14 days |
|
St. John's wort (Hypericum perforatum) |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, St. John's wort, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Tolbutamide |
Multiple-dose vortioxetine did not have a clinically important effect on the pharmacokinetics of tolbutamide (a CYP2C9 substrate) |
|
|
Tramadol |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, tramadol, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
|
Tryptophan |
Potentially life-threatening serotonin syndrome |
If concomitant use clinically warranted, advise patients of the increased risk for serotonin syndrome, particularly during treatment initiation and dosage increases If serotonin syndrome occurs, immediately discontinue vortioxetine, tryptophan, and any concurrently administered serotonergic agents; initiate supportive and symptomatic treatment |
Vortioxetine Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability of 75%.
Peak plasma concentrations achieved within 7–11 hours after oral administration. Steady-state concentrations are achieved within 2 weeks.
Onset
Antidepressant effect generally evident in 2 weeks; full antidepressant effect may take ≥4 weeks.
Food
Administration with food does not affect pharmacokinetics.
Distribution
Extent
Extensively distributed.
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
98% (independent of plasma concentration).
Elimination
Metabolism
Extensively metabolized via oxidation by CYP isoenzymes, principally by CYP2D6 with lesser contributions from CYP3A4/5, 2C19, 2C9, 2A6, 2C8, and 2B6, and subsequent glucuronic acid conjugation. CYP2D6 is the main enzyme catalyzing the metabolism of vortioxetine to its principal, inactive carboxylic acid metabolite.
Elimination Route
59 and 26% recovered in the urine and feces, respectively, as metabolites. Negligible amounts of unchanged vortioxetine excreted in urine.
Half-life
Approximately 66 hours.
Special Populations
Mild or moderate hepatic impairment does not affect apparent clearance.
Mild, moderate, or severe renal impairment or end-stage renal disease does not affect apparent clearance. Only a small fraction of a single, 10-mg dose of vortioxetine was removed by dialysis; AUC and peak plasma concentrations were 13 and 27% lower, respectively.
In a single-dose pharmacokinetic study, pharmacokinetics generally similar between geriatric individuals >65 years of age and younger individuals (24–45 years of age).
Poor CYP2D6 metabolizers: Plasma concentrations of vortioxetine are approximately twice those in extensive CYP2D6 metabolizers. (See Dosage under Dosage and Administration.)
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Actions
-
Serotonergic antidepressant. Precise mechanism of antidepressant effect not fully understood, but thought to be related to enhancement of serotonergic activity in the CNS through inhibition of serotonin reuptake.
-
Possesses several other activities, including 5-HT3 receptor antagonism and 5-HT1A receptor agonism; contribution of these activities to the drug’s antidepressant effect not established.
-
Binds with high affinity to the human serotonin transporter, but not to norepinephrine or dopamine transporters.
-
Potently and selectively inhibits the reuptake of serotonin and binds to 5-HT3, 5-HT1A, 5-HT7, 5-HT1D, and 5-HT1B receptors. The drug is a 5-HT3, 5-HT1D, and 5-HT7 receptor antagonist; a 5-HT1B receptor partial agonist; and a 5-HT1A receptor agonist.
Advice to Patients
-
Importance of providing copy of written patient information (medication guide) each time vortioxetine is dispensed. Importance of advising patients and their caregivers to read the patient information before taking vortioxetine and each time the prescription is refilled.
-
Importance of advising patients to check their prescription carefully to ensure that they have received the correct drug; prescribing and dispensing errors have been reported due to similarities in the spelling and pronunciation of Brintellix (the former trade name for vortioxetine, which was changed to Trintellix in May 2016) and Brilinta (the trade name for ticagrelor, a platelet aggregation inhibitor). (See Prescribing and Dispensing Precautions under Cautions.)
-
Risk of suicidality; importance of patients, family, and caregivers being alert to and immediately reporting emergence of suicidality, worsening depression, or unusual changes in behavior, especially during the first few months of therapy or during periods of dosage adjustment. (See Worsening of Depression and Suicidality Risk under Cautions.)
-
Importance of informing patients who are receiving vortioxetine 15 or 20 mg daily that they may experience possible withdrawal reactions (e.g., headache, muscle tension, mood swings, sudden outbursts of anger, dizziness, runny nose) if they abruptly stop the drug. Patients should be advised not to stop taking vortioxetine without first talking with their clinician.
-
Importance of instructing patients not to take vortioxetine with or within 14 days of discontinuing an MAO inhibitor and to allow 21 days after stopping vortioxetine before starting an MAO inhibitor.
-
Importance of informing patients of potential risk of serotonin syndrome, particularly with concurrent use of vortioxetine and other serotonergic agents or antipsychotic agents. (See Interactions.) Importance of immediately contacting clinician if manifestations of serotonin syndrome develop (e.g., restlessness, hallucinations, delirium, loss of coordination, fast heart beat, increased body temperature, sweating, muscle stiffness, labile BP, diarrhea, coma, nausea, vomiting, confusion).
-
Importance of advising patients that vortioxetine can be taken with or without food, and should be taken at about the same time every day.
-
Importance of informing patients that if they receive diuretics, are otherwise volume depleted, or are elderly, that they may be at greater risk of developing hyponatremia while taking vortioxetine.
-
Importance of informing patients that nausea is the most common adverse effect associated with vortioxetine, and that it is dose related. Nausea commonly occurs within the first week of treatment then decreases in frequency, but can persist.
-
Risk of cognitive and motor impairment; although not observed in a trial in healthy individuals, importance of patients exercising caution while operating hazardous machinery, including driving a motor vehicle, until they are reasonably certain that vortioxetine therapy does not adversely affect their ability to engage in such activities.
-
Importance of advising patients to avoid alcohol consumption during vortioxetine therapy.
-
Importance of advising patients to notify their clinician if any signs or symptoms of an allergic reaction develop during therapy (e.g., rash, hives, swelling, difficulty breathing).
-
Importance of advising patients, their families, and caregivers to look for signs of activation of mania/hypomania.
-
Importance of advising patients that vortioxetine can cause mild pupillary dilation, which can lead to an episode of angle-closure glaucoma in susceptible individuals. Possible symptoms include eye pain, vision changes, and swelling or redness in or around the eye. Preexisting glaucoma is almost always open-angle glaucoma since angle-closure glaucoma can be treated definitively with iridectomy when diagnosed; open-angle glaucoma is not a risk factor for angle-closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle-closure glaucoma and have a prophylactic procedure (e.g., iridectomy) if they are susceptible.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs or herbal supplements, as well as any concomitant illnesses (e.g., liver disease, glaucoma) or personal or family history of suicidality or bipolar disorder. Importance of advising patients about the risk of bleeding associated with concomitant use of vortioxetine with aspirin or other NSAIAs, warfarin, or other drugs that affect coagulation.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
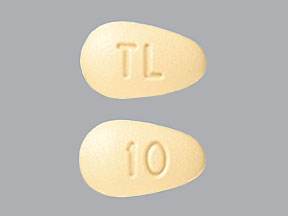
Tablets, film-coated |
5 mg (of vortioxetine) |
Trintellix |
Takeda |
|
10 mg (of vortioxetine) |
Trintellix |
Takeda |
||
|
15 mg (of vortioxetine) |
Trintellix |
Takeda |
||
|
20 mg (of vortioxetine) |
Trintellix |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 8, 2016. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Is Trintellix the same as Brintellix?
- Does Trintellix (vortioxetine) cause weight gain or loss?
- How long does it take for Trintellix (vortioxetine) to start working?
- Is Trintellix (vortioxetine) good for anxiety?
- Shall I take Trintellix (vortioxetine) in the night or morning?
- Can I take Cymbalta (duloxetine) and Trintellix (vortioxetine) together?
More about vortioxetine
- Check interactions
- Compare alternatives
- Reviews (1,579)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: miscellaneous antidepressants
- Breastfeeding
- En español