Pantoprazole (Monograph)
Brand name: Protonix
Drug class: Proton-pump Inhibitors
Introduction
Acid- or proton-pump inhibitor (PPI); gastric antisecretory agent.1 10
Uses for Pantoprazole
Gastroesophageal Reflux (GERD)/Erosive Esophagitis
Orally for short-term treatment of erosive esophagitis in patients with GERD.1 352 353
Orally to maintain healing and decrease recurrence of erosive esophagitis.1 354 355
IV for up to 7–10 days in the treatment of GERD in patients with a history of erosive esophagitis.10 28 356 Discontinue IV therapy as soon as patient is able to initiate or resume oral therapy.10
Guidelines recommend a 4- or 8-week trial of once-daily PPI therapy for initial management of GERD symptoms (i.e., heartburn, regurgitation, non-cardiac chest pain).8000 8001
In patients who experience incomplete symptom relief or symptom recurrence following trial PPI therapy for GERD, esophagogastroduodenoscopy is recommended.8000 8001 Optimize PPI therapy in patients with evidence of erosion (i.e. Los Angeles A-D esophagitis); may continue indefinitely in patients with more severe disease.8000 8001
Pathologic GI Hypersecretory Conditions
Orally for treatment of pathologic hypersecretory conditions, including Zollinger-Ellison syndrome.1 357 358
IV for up to 6 days in the treatment of pathologic hypersecretory conditions associated with Zollinger-Ellison syndrome or other neoplastic conditions.10 359 360
Duodenal Ulcer
Orally for treatment of duodenal ulcer† [off-label].2 3 5 6 8
Gastric Ulcer
Orally for treatment of gastric ulcer† [off-label].2 3 5 6 8
Pantoprazole Dosage and Administration
General
Pretreatment Screening
-
In patients expected to receive long-term therapy with a PPI or in those receiving a PPI concomitantly with digoxin or medications that may cause hypomagnesemia (e.g., diuretics), clinicians should consider measurement of serum magnesium concentrations prior to initiation of PPI therapy.1 10
-
In patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism), consider monitoring magnesium and calcium levels prior to initiation of PPI therapy.1 10
Patient Monitoring
-
In patients expected to receive long-term therapy with a PPI or in those receiving a PPI concomitantly with digoxin or medications that may cause hypomagnesemia (e.g., diuretics), clinicians should consider measurement of serum magnesium concentrations periodically during therapy.1 10
-
In patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism), consider monitoring magnesium and calcium levels periodically during therapy.1 10
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) includes Protonix, protamine, and Lotronex on their ISMP List of Confused Drug Names, and recommends using special safeguards to ensure the accuracy of prescriptions for these medications.362
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes pantoprazole on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings.999 The criteria are intended to apply to adults 65 years of age and older in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings.999 For proton-pump inhibitors including pantoprazole, the Beers Criteria Expert Panel recommends that scheduled use for more than 8 weeks generally be avoided with certain exceptions.999
Administration
Administer orally or IV.1 10 Administer once daily for GERD and erosive esophagitis.1 10 Generally given twice daily for pathologic GI hypersecretory conditions, although may be administered IV every 8 hours if necessary.1 10
Oral Administration
Delayed-release Tablets
Administer delayed-release tablets without regard to meals.1
Antacids may be used concomitantly.1
Swallow tablets whole; do not split, crush, or chew.1 May administer two 20-mg tablets if unable to swallow a 40-mg tablet.1
Delayed-release Oral Suspension
Do not divide the contents of a packet of delayed-release granules for oral suspension to prepare a dose that is smaller than the full labeled dose (e.g., do not use a 40-mg packet to prepare a 20-mg dose for a child who is unable to swallow the delayed-release tablets).1
Administer delayed-release oral suspension 30 minutes before a meal.1
Mix delayed-release granules for oral suspension with applesauce or apple juice; do not mix with any other foods or liquids (including water).1
Sprinkle the contents of a single-dose packet of pantoprazole sodium delayed-release granules for oral suspension onto 1 teaspoonful of applesauce and administer within 10 minutes of preparation.1 Follow with sips of water, repeated as necessary, to ensure complete delivery of the dose.1
Alternatively, sprinkle the packet contents into 5 mL of apple juice, stir for 5 seconds (granules will not dissolve), and swallow the resulting suspension immediately.1 Rinse the container once or twice with apple juice; swallow the rinsings immediately to ensure complete delivery of the dose.1
Swallow granules in the oral suspension intact; do not crush or chew the granules.1
Nasogastric (NG) Tube
May administer pantoprazole sodium delayed-release granules for oral suspension via a nasogastric or (NG) gastrostomy tube (16 French or larger).1
Remove the plunger from a 60-mL syringe and attach the catheter tip of the syringe to the NG or gastrostomy tube.1 Empty the contents of a single-dose packet of the granules into the syringe barrel while holding the syringe as high as possible to prevent bending of the tubing.1 Add 10 mL of apple juice to the syringe; gently tap or shake the syringe to facilitate emptying.1 Rinse the syringe and tubing with 10 mL of apple juice at least 2 more times (until no granules remain).1
IV Administration
Administer through a dedicated IV line or a Y-site.10
Must reconstitute commercially available injection.10 In adults, the reconstituted solution may be administered directly as an IV injection (over at least 2 minutes) or further diluted for administration as an IV infusion (over 15 minutes); for pediatric patients, the reconstituted solution must be further diluted prior to administration and administered as an IV infusion over 15 minutes.10
Reconstitution and Dilution
2-minute IV injection method in adults with GERD: reconstitute each vial with 10 mL of 0.9% sodium chloride injection to provide a solution containing about 4 mg/mL.10 May store reconstituted solution for up to 24 hours at room temperature (up to 30°C) prior to administration; do not freeze.10
15-minute IV infusion method in pediatric patients or adults with GERD:reconstitute each vial with 10 mL of 0.9% sodium chloride injection.10 In adults and pediatric patients ≥1 year of age, further dilute reconstituted solution with 100 mL of 0.9% sodium chloride injection or 5% dextrose injection to final concentration of approximately 0.4 mg/mL.10 In pediatric patients 3 months to <1 year of age, further dilute reconstituted solution with 21 mL of 0.9% sodium chloride injection to final concentration of about 1.3 mg/mL.10 May store reconstituted solution for up to 6 hours at room temperature (up to 30°C) prior to further dilution; may store diluted solution at room temperature but must use within 24 hours from time of initial reconstitution.10 Do not freeze.10
2-minute IV injection method in adults with hypersecretory conditions:reconstitute each of two vials with 10 mL of 0.9% sodium chloride injection to a final concentration of approximately 4 mg/mL.10 May store reconstituted solution for up to 24 hours at room temperature prior to IV injection; do not freeze.10
15-minute IV infusion method in adults with hypersecretory conditions:reconstitute each of two vials with 10 mL of 0.9% sodium chloride injection; combine contents and dilute with 80 mL of 0.9% sodium chloride injection or 5% dextrose injection to a total volume of 100 mL with final concentration of approximately 0.8 mg/mL.10 May store reconstituted solution at room temperature (up to 30°C) for up to 6 hours prior to further dilution.1 May store diluted solution at room temperature for up to 24 hours from the time of initial reconstitution; do not freeze the reconstituted or diluted solution.10
Rate of Administration
Pediatric patients with GERD (≥3 months to 17 years of age): Administer desired dose IV as the 1.3 mg/mL dilution or 0.4-mg/mL dilution depending on age over about 15 minutes.10
Adults with GERD: Administer 40-mg dose IV as the reconstituted (4 mg/mL) solution over not less than 2 minutes10 or as the 0.4-mg/mL dilution over about 15 minutes (7 mL/minute).10
Adults with pathologic hypersecretory conditions: Administer 80-mg dose IV as the reconstituted (4 mg/mL) solution over not less than 2 minutes10 or as the 0.8-mg/mL dilution over about 15 minutes (7 mL/minute).10
Standardize 4 Safety
Standardized concentrations for pantoprazole have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care.249 Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label.249 For additional information on S4S (including updates that may be available), see [Web].249
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Pediatric patients (<50 kg) |
0.8 mg/mL |
mg/kg/hour |
Dosage
Available as pantoprazole sodium; dosage expressed in terms of pantoprazole.1 10
Pediatric Patients
GERD
Treatment of Erosive Esophagitis
OralChildren ≥5 years of age: 20 mg once daily in those weighing 15 to <40 kg; 40 mg once daily in those weighing ≥40 kg.1 Continue for up to 8 weeks; safety beyond 8 weeks not established.1
IVChildren ≥3 months of age to <1 year of age: 0.8 mg/kg once daily in those weighing <12.5 kg; 10 mg once daily in those weighing ≥12.5 kg.10 Continue for up to 7 days; safety and efficacy beyond 7 days not established.10
Children ≥1 year to 17 years of age: 10 mg once daily in those weighing ≤15 kg; 20 mg once daily in those weighing >15 to ≤40 kg; 40 mg once daily in those weighing >40 kg.10 Continue for up to 7 days; safety and efficacy beyond 7 days not established.10
Adults
GERD
IV
40 mg once daily for 7–10 days.10 Discontinue IV therapy when patient is able to initiate or resume oral therapy; safety and efficacy of IV therapy for >10 days not established.10
Treatment of Erosive Esophagitis
Oral40 mg once daily for up to 8 weeks.1 If not healed, consider additional 8 weeks of therapy.1
Maintenance of Healing of Erosive Esophagitis
Oral40 mg once daily.1 Not studied for >1 year of therapy.1
Pathologic GI Hypersecretory Conditions (e.g., Zollinger-Ellison Syndrome)
Oral
40 mg twice daily.1 Adjust dosage according to patient response and tolerance; continue therapy as long as necessary.1 May require dosages of up to 240 mg daily.1 Patients with Zollinger-Ellison syndrome have been treated for >2 years.1
IV
80 mg every 12 hours.10 80 mg every 8 hours is expected to maintain acid output <10 mEq/hour in patients requiring higher dosage.10 Safety and efficacy of dosages exceeding 240 mg daily or use of IV pantoprazole for >6 days not established.10
Special Populations
Hepatic Impairment
Manufacturer states no dosage adjustment necessary; doses exceeding 40 mg daily have not been studied in this population.1 10
Renal Impairment
No dosage recommendations at this time.1 10
Geriatric Patients
No dosage recommendations at this time.10
Poor Metabolizers of CYP2C19
Manufacturer recommends considering reduced dosage in pediatric patients who are poor metabolizers of CYP2C19 substrates.1
Manufacturer states no dosage adjustment required in adults who are poor metabolizers of CYP2C19 substrates.1 10
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines state that, in patients who are CYP2C19 likely intermediate metabolizers (e.g., CYP2C19*1/*9, CYP2C19*9/*17, CYP2C19*9/*9), intermediate metabolizers (e.g., CYP2C19*1/*2, CYP2C19*1/*3, CYP2C19*2/*17, CYP2C19*3/*17), likely poor metabolizers (e.g., CYP2C19*2/*9 or CYP2C19*3/*9), or poor metabolizers (e.g., CYP2C19*1/*12, CYP2C19*2/*12, CYP2C19*12/*14), standard PPI dosages may be initiated; however, for chronic therapy >12 weeks, a 50% dosage reduction is recommended with monitoring for continued efficacy.361 Alternatively, in patients who are CYP2C19 rapid metabolizers (e.g., CYP2C19*1/*17) or normal metabolizers (e.g., CYP2C19*1/*1), standard PPI dosages may be initiated; however, dosage increases of 50-100% should be considered along with continued monitoring for treatment of H. pylori infection due to an increased risk of therapeutic failure.361 In patients who are CYP2C19 ultrarapid metabolizers (e.g., CYP2C19*17/*17), consider an increase in the starting dosage by 100% due to the risk of therapeutic failure.361
Cautions for Pantoprazole
Contraindications
-
Known hypersensitivity to pantoprazole, any ingredient in the formulation, or to other substituted benzimidazoles (e.g., esomeprazole, lansoprazole, omeprazole, rabeprazole).1 10
Warnings/Precautions
Gastric Malignancy
Response to pantoprazole does not preclude presence of occult gastric neoplasm.1 10 Consider additional follow-up and diagnostic testing (including an endoscopy in older patients) in adults with suboptimal response or early symptomatic relapse after completing PPI treatment.1 10
Injection Site Reactions
Injection site reactions (e.g., thrombophlebitis, abscess) associated with IV pantoprazole.10 Patient assessment and catheter removal recommended if clinically indicated.10
Potential for Zinc Deficiency
Pantoprazole sodium for injection contains edetate disodium (disodium EDTA), a potent metal ion (e.g., zinc) chelator.10 Consider zinc supplementation in patients prone to zinc deficiency.10 Use caution with other IV products that contain edetate disodium.10
Acute Tubulointerstitial Nephritis
Acute tubulointerstitial nephritis (TIN) reported.1 10 Clinical presentation variable; may present as symptomatic hypersensitivity reactions or non-specific symptoms of reduced renal function such as malaise, nausea, or anorexia.1 10 Discontinue pantoprazole and evaluate the patient if TIN suspected.
Clostridioides difficile-associated Diarrhea
PPIs associated with possible increased risk of Clostridioides difficile-associated diarrhea (CDAD), particularly in hospitalized inpatients.1 10 Consider CDAD in patients with diarrhea that does not improve.1 10
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient's clinical condition.1 10
Bone Fracture
Several observational studies suggest PPIs, particularly in high dosages (i.e., multiple daily doses) and/or for prolonged periods of time (i.e., ≥1 year), may be associated with increased risk of osteoporosis-related fractures of the hip, wrist, or spine.1 10
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient’s clinical condition.1 10
Individuals at risk for osteoporosis-related fractures should be managed according to current standards of care.1 10
Severe Cutaneous Adverse Reactions
Reports of severe cutaneous adverse reactions (SCARS), including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) suggest possible association with PPI therapy.1 10 Discontinue pantoprazole at first signs or symptoms of SCARS or other signs of hypersensitivity and consider further evaluation.1 10
Cutaneous and Systemic Lupus Erythematosus
New onset cases of cutaneous lupus erythematosus (CLE) and systemic lupus erythematosus (SLE) reported.1 10
Avoid administering PPIs for longer than appropriate for the clinical condition.1 10 If signs or symptoms of CLE or SLE occur, discontinue pantoprazole therapy and refer to a specialist.1 10 After discontinuation of the PPI, most patients improve after 4-12 weeks, although serological testing (e.g., antinuclear antibodies) may remain positive and serological test elevations may not result until after clinical improvement is noted.1 10
Hepatic Effects
Mild, transient elevations in transaminases reported with IV pantoprazole.10 Clinical significance of this finding not known.10
Cyanocobalamin (Vitamin B-12) Deficiency
Deficiency due to malabsorption from prolonged (e.g., >3 years) gastric acid suppression reported rarely.1 Consider possibility if manifestations of cyanocobalamin deficiency occur.1
Hypomagnesemia and Mineral Metabolism
Hypomagnesemia, symptomatic and asymptomatic, reported rarely in patients receiving long-term therapy (≥3 months or, in most cases, >1 year) with PPIs, including pantoprazole.1 10 Serious adverse effects include tetany, seizures, and arrhythmias (e.g., atrial fibrillation, supraventricular tachycardia).1 10 Most patients required magnesium replacement and discontinuance of the PPI.1 10
In patients expected to receive long-term PPI therapy or in patients currently receiving digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), consider measuring serum magnesium concentrations prior to initiation of prescription PPI therapy and periodically thereafter.1 10 In patients with preexisting risk of hypocalcemia (e.g., hypoparathyroidism), consider monitoring magnesium and calcium levels prior to initiation of PPI therapy and periodically thereafter.1 10 Supplement with calcium and/or magnesium as needed.1 10 In refractory hypocalcemia, consider discontinuation of the PPI.1 10
Tumorigenicity
Potential for prolonged administration of pantoprazole due to chronic nature of disease; in long-term animal studies, pantoprazole caused rare types of GI tumors (clinical relevance of this finding in humans not known).1
Fundic Gland Polyps
Use of PPI therapy associated with increased risk of fundic gland polyps; risk increases with long-term use, especially >1 year.1 10 Use the shortest duration of PPI therapy for the clinical condition being treated.1 10
Interference with Investigations for Neuroendocrine Tumors
Increases in intragastric pH result in secondary increases in serum chromogranin A (CgA), which can result in false positive results during diagnostic testing for neuroendocrine tumors.1 10 Clinicians should temporarily withhold pantoprazole for ≥14 days before assessing CgA levels; consider a repeat assessment if CgA levels are elevated.1 10 If performing serial testing (e.g., for monitoring), use the same commercial laboratory for testing, as reference ranges between tests may vary.1 10
Interference with Urine Screen for Cannabinoids
False-positive results for urine screening tests for tetrahydrocannabinol (THC) have been reported in patients receiving PPIs, including pantoprazole.1 10 Consider an alternative confirmatory test to verify positive urine THC screening results.1 10
Concomitant Use of IV Pantoprazole with Methotrexate
Data suggest concomitant use of PPIs with methotrexate (primarily at high doses), may elevate and prolong serum levels of methotrexate and/or its metabolite and possibly lead to methotrexate toxicities.1 10 Temporary withdrawal of the PPI may be considered in some patients receiving high-dose methotrexate.1 10
Specific Populations
Pregnancy
Observational data have not demonstrated an association between pantoprazole and major fetal malformations or other adverse pregnancy outcomes.1 10
Lactation
Limited data indicate pantoprazole passes into breast milk.1 10 Following a 40 mg dose of oral pantoprazole, drug was detectable in the milk 2 and 4 hours after the dose.1 10 Relative dose to the infant was 0.14% of the weight-adjusted maternal dose.1 10 There were no effects on the breast-fed infant from pantoprazole exposure.1 10 Not known if pantoprazole affects milk production.1 10
Pediatric Use
Safety and efficacy of oral pantoprazole for short-term treatment of erosive esophagitis associated with GERD established in pediatric patients 1–16 years of age.1 However, oral pantoprazole is labeled for use only in children ≥5 years of age because an appropriate dosage formulation is not available for children <5 years of age.1 Efficacy of oral pantoprazole not established in infants <1 year of age.1
Pantoprazole was not more effective than placebo in a treatment-withdrawal study in infants 1–11 months of age with symptomatic GERD.1
Safety and efficacy of IV pantoprazole for short term treatment of GERD was associated with a history of erosive esophagitis established in pediatric patients ≥3 months of age.10
Adverse reactions were generally similar to those reported in adults receiving IV or oral pantoprazole.10
Safety and efficacy of IV pantoprazole for treatment of GERD associated with a history of erosive esophagitis not established in pediatric patients <3 months of age.10
Safety and efficacy of IV pantoprazole not established for treatment of pathological hypersecretory conditions (including Zollinger-Ellison syndrome) in pediatric patients.10
Geriatric Use
No clinically meaningful differences in pharmacokinetics, safety, or efficacy relative to younger adults.1 10 However, a greater sensitivity of some geriatric patients cannot be ruled out.10
Hepatic Impairment
Pharmacokinetic changes in patients with hepatic impairment result in minimal accumulation following once-daily, multiple dose administration.1 10 Maximum pantoprazole concentrations increased only slightly (1.5-fold) in patients with mild to severe hepatic impairment (Child-Pugh Class A to C) relative to healthy patients.1 10 Dosages >40 mg daily not studied in patients with hepatic impairment.1 10
Renal Impairment
Pharmacokinetics similar in patients with severe renal impairment relative to healthy patients.1 10
Common Adverse Effects
Oral (adults): Headache, diarrhea, nausea, abdominal pain, vomiting, flatulence, dizziness, arthralgia.1
Oral (pediatric patients): Upper respiratory tract infection, headache, diarrhea, abdominal pain, vomiting, fever, and rash.1
IV: Headache, diarrhea, nausea, abdominal pain, vomiting, flatulence, dizziness, arthralgia.10
Drug Interactions
Extensively metabolized, principally by CYP2C19 and to a minor extent by CYP3A4, 2D6, and 2C9.1 10 No evidence that metabolites of pantoprazole have significant pharmacologic activity.1 10
Drugs that Cause Hypomagnesemia
In patients receiving digoxin or diuretics (i.e., loop or thiazide diuretics) or other medications that cause hypomagnesemia, consider monitoring magnesium concentrations prior to initiation of PPI therapy and periodically thereafter.1 10 Supplementation with magnesium may be necessary.1 10
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
||
|
Amoxicillin |
||
|
Antacids |
No clinically important effects on oral pantoprazole absorption1 |
May be used concomitantly1 |
|
Antipyrine |
||
|
Atazanavir |
Possible altered oral absorption of atazanavir, resulting in decreased plasma atazanavir concentrations; possible loss of virologic response or development of drug resistance1 10 |
Refer to atazanavir prescribing information for recommendations on concomitant use1 10 |
|
Caffeine |
||
|
Carbamazepine |
||
|
Cisapride |
||
|
Clarithromycin |
||
|
Clopidogrel |
Pantoprazole decreased exposure to the metabolite by about 14%;1 10 observed effects on metabolite exposure and clopidogrel-induced platelet inhibition not considered clinically important1 10 |
Manufacturer of pantoprazole states clopidogrel dosage adjustment not required if used with recommended pantoprazole dosages1 10 |
|
Diazepam |
||
|
Diclofenac |
||
|
Digoxin |
Pharmacokinetic interaction unlikely1 10 Possible increased risk of hypomagnesemia (e.g., resulting from long-term use of PPIs)1 10 |
Consider monitoring magnesium concentrations prior to initiation of PPI therapy and periodically thereafter1 10 |
|
Diuretics (i.e., loop or thiazide diuretics) |
Consider monitoring magnesium concentrations prior to initiation of PPI therapy and periodically thereafter1 10 |
|
|
Gastric pH-dependent drugs (e.g., iron salts, erlotinib, dasatinib, nilotinib, mycophenolate mofetil [MMF], ketoconazole, itraconazole) |
||
|
Glyburide |
||
|
Methotrexate |
Possible delayed clearance and increased serum concentrations of methotrexate and/or its metabolite hydroxymethotrexate; possible methotrexate toxicity1 10 |
Manufacturer of pantoprazole recommends considering temporary discontinuance of PPI therapy in some patients receiving high-dose methotrexate1 10 |
|
Metoprolol |
||
|
Metronidazole |
||
|
Midazolam |
||
|
Mycophenolate mofetil [MMF] |
Pantoprazole may reduce drug absorption1 10 Reduced exposure to active metabolite of MMF (mycophenolic acid) reported; clinical relevance on transplant rejection has not been established1 10 |
Use pantoprazole with caution in transplant recipients receiving MMF1 10 |
|
Naproxen |
||
|
Nelfinavir |
Omeprazole decreased plasma concentrations of nelfinavir1 10 |
|
|
Nifedipine |
||
|
Oral contraceptives (e.g., levonorgestrel/ethinyl estradiol) |
||
|
Phenytoin |
||
|
Piroxicam |
||
|
Rilpivirine |
Concomitant use of rilpivirine and pantoprazole contraindicated1 10 |
|
|
Theophylline |
||
|
Warfarin |
Pantoprazole Pharmacokinetics
Absorption
Bioavailability
Well absorbed from GI tract (absolute bioavailability about 77%).1 Peak plasma concentrations attained about 2.5 hours after single or multiple 40-mg oral doses (as delayed-release tablets).1 Time to peak concentration is similar (2–2.5 hours) for delayed-release suspension administered orally or via NG tube.1
Administration of delayed-release oral suspension (in apple juice) via NG tube is bioequivalent to oral administration of the same formulation (in applesauce or apple juice).1
AUC after single oral 40-mg dose about 39% higher in children 6–11 years of age and about 10% higher in adolescents 12–16 years of age compared with adults.1
Onset
51% mean inhibition of gastric acid secretion within 2.5 hours after a single 40-mg oral dose; 85% after daily administration for 7 days.1
15–30 minutes after single 20- to 120-mg IV infusion.10 About 96% suppression of pentagastrin-stimulated acid output within 2 hours after 80-mg IV infusion.10
Duration
Acid secretion normalized within one week after discontinuance of oral pantoprazole; no apparent rebound hypersecretion.1
24 hours after single IV infusion.10 Median percentage of time the gastric pH ≥4 similar after 40 mg IV or orally daily for 5 days.10
Food
Food delays absorption of delayed-release tablets but does not affect extent or peak plasma concentrations.1
Special Populations
Pharmacokinetics in patients with severe renal impairment similar to healthy individuals.1 10
Peak plasma concentrations and AUCs increased in patients with mild to severe hepatic impairment, but no more than in slow metabolizers.1 10 Minimal accumulation with once-daily dosing.1 10
Repeated administration of IV pantoprazole in geriatric patients 65-76 years of age results in a similar half-life to that observed in younger adults.10
Distribution
Extent
Distributed into human milk.1 10
Plasma Protein Binding
Elimination
Metabolism
Metabolized in the liver, principally by CYP2C19, and to a lesser extent by CYP3A4.1 10 Metabolites appear to be inactive.1 10
Elimination Route
Excreted in urine (about 71%) and feces (18%); no unchanged drug excreted in urine.1 10
Half-life
Special Populations
Elimination half-life increased to 7-9 hours in hepatic impairment, but no more than in slow metabolizers, and minimal accumulation occurs.1 10
In adults with poor CYP2C19 metabolizer phenotype, metabolism is slower than in those with extensive (or rapid) metabolizer phenotype; elimination half-life is 3.5–10 hours, but minimal accumulation occurs with once-daily dosing.1 10
In pediatric patients, oral clearance in poor metabolizers (CYP2C19 *2/*2 genotype) is about 10-fold lower than in extensive metabolizers (CYP2C19 *1/*1) and AUC is more than 6-fold higher than in extensive or intermediate (CYP2C19 *1/*x) metabolizers.1 10
Stability
Storage
Oral
Delayed-release Tablets
20–25°C (may be exposed to 15–30°C).1
Granules for Delayed-release Suspension
20–25°C (may be exposed to 15–30°C).1
Parenteral
Powder for Injection
20–25°C (may be exposed to 15–30°C).10 Protect from light.10
Store reconstituted (4 mg/mL) solution at room temperature for up to 24 hours prior to administration as 4-mg/mL solution.10 If reconstituted solution will be further diluted, store reconstituted solution at room temperature for up to 6 hours before dilution; then store diluted (0.4 or 0.8 mg/mL) solution at room temperature and use within 24 hours of initial reconstitution.10 Do not freeze reconstituted solution.10
Actions
-
Concentrates in acid conditions of parietal cell secretory canaliculi; forms active sulfenamide metabolite that irreversibly binds to and inactivates hydrogen-potassium ATPase (proton- or acid pump), blocking final step in secretion of hydrochloric acid.1 10 Acid secretion is inhibited until additional hydrogen-potassium ATPase is synthesized, resulting in prolonged duration of action.1 10
Advice to Patients
-
Advise patients to return to their clinician for further follow-up if they have a suboptimal response or an early symptomatic relapse.1
-
Advise patients to immediately call their healthcare provider if they have signs and/or symptoms of acute TIN.1
-
Instruct patients regarding proper administration of delayed-release oral preparations.1 Advise patients that delayed-release tablets should be swallowed whole, without crushing or chewing.1 Advise patients to prepare the delayed-release suspension according to the manufacturer’s directions and administer the suspension 30 minutes before a meal.1 Advise patients not to divide the contents of a packet of delayed-release granules for oral suspension to prepare a dose that is smaller than the full labeled dose.1
-
Advise patients to report any fractures of the hip, wrist, or spine to their healthcare provider.1
-
Advise patients to discontinue pantoprazole immediately and to contact their healthcare provider if they have any severe cutaneous adverse reaction.1
-
Advise patients to immediately contact their healthcare provider for any new or worsening symptoms associated with cutaneous or systemic lupus erythematosus.1
-
Advise patients to report any clinical symptoms to their healthcare provider that may be associated with cyanocobalamin deficiency if they have been receiving pantoprazole for >3 years.1
-
Advise patients to report any symptoms that may be associated with hypomagnesemia, hypocalcemia, or hypokalemia if they have been receiving pantoprazole for ≥3 months.1
-
Possible increased risk of Clostridioides difficile infection; advise patients to contact a clinician if they experience diarrhea that does not improve.1
-
Advise patients to continue therapy for the entire treatment course, unless directed otherwise.1
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.1 Antacid administration is permissible with pantoprazole delayed-release tablets.1
-
Advise females of child bearing potential to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1 10
-
Advise patients of other important precautionary information.1 10
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension, delayed-release (containing enteric-coated granules) |
40 mg (of pantoprazole) per packet* |
Pantoprazole Sodium Delayed-release Suspension |
|
|
Protonix |
Pfizer |
|||
|
Tablets, delayed-release (enteric-coated) |
20 mg (of pantoprazole)* |
Pantoprazole Sodium Delayed-release Tablets |
||
|
Protonix |
Pfizer |
|||
|
40 mg (of pantoprazole)* |
Pantoprazole Sodium Delayed-release Tablets |
|||
|
Protonix |
Pfizer |
|||
|
Parenteral |
For injection, for IV infusion |
40 mg (of pantoprazole)* |
Pantoprazole Sodium for Injection |
|
|
Protonix I.V. |
Pfizer |
|||
|
Injection, for IV infusion |
0.4 mg (of pantoprazole) per mL* |
Pantoprazole Sodium in 0.9% Sodium Chloride Injection (40 mg) |
||
|
0.8 mg (of pantoprazole) per mL* |
Pantoprazole Sodium in 0.9% Sodium Chloride Injection (40 mg or 80 mg) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Pfizer. Protonix (pantoprazole sodium) delayed-release tablets and for delayed-release oral suspension prescribing information. Philadelphia, PA; 2023 June.
2. Anon. Pantoprazole (Protonix). Med Lett Drugs Ther. 2000; 42:65-6. https://pubmed.ncbi.nlm.nih.gov/10908422
3. Fitton A, Wiseman L. Pantoprazole: a review of its pharmacological properties and therapeutic use in acid-related disorders. Drugs. 1996; 51:460-82. https://pubmed.ncbi.nlm.nih.gov/8882382
5. Richardson P, Hawkey CJ, Stack WA. Proton pump inhibitors: pharmacology and rationale for use in gastrointestinal disorders. Drugs. 1998; 56:307-35. https://pubmed.ncbi.nlm.nih.gov/9777309
6. Webb DD. New therapeutic options in the treatment of GERD and other acid-peptic disorders. Am J Managed Care. 2000; 6:S467-75.
8. Horn J. The proton-pump inhibitors: similarities and differences. Clin Ther. 2000; 22:266-80. https://pubmed.ncbi.nlm.nih.gov/10963283
10. Wyeth. Protonix (pantoprazole sodium) I.V. for injection prescribing information. Philadelphia, PA; 2024 Aug.
28. Pratha V, Hogan DL, Lynn RB et al. Intravenous pantoprazole as initial treatment in patients with gastroesophageal reflux disease and a history of erosive esophagitis: a randomized clinical trial. Dig Dis Sci. 2006; 51:1595-601. https://pubmed.ncbi.nlm.nih.gov/16927137
249. ASHP. Standardize 4 Safety: pediatric continuous infusion standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
352. Richter JE, Bochenek W. Oral pantoprazole for erosive esophagitis: a placebo-controlled, randomized clinical trial. Pantoprazole US GERD Study Group. Am J Gastroenterol. 2000;95(11):3071-3080.
353. Kovacs TO, Wilcox CM, DeVault K, Miska D, Bochenek W; Pantoprozole US Gerd Study Group B. Comparison of the efficacy of pantoprazole vs. nizatidine in the treatment of erosive oesophagitis: a randomized, active-controlled, double-blind study. Aliment Pharmacol Ther. 2002;16(12):2043-2052.
354. Metz DC, Bochenek WJ; Pantoprazole US GERD Study Group. Pantoprazole maintenance therapy prevents relapse of erosive oesophagitis. Aliment Pharmacol Ther. 2003;17(1):155-164.
355. Richter JE, Fraga P, Mack M, Sabesin SM, Bochenek W; Pantoprazole US GERD Study Group. Prevention of erosive oesophagitis relapse with pantoprazole. Aliment Pharmacol Ther. 2004;20(5):567-575.
356. Metz DC, Pratha V, Martin P, et al. Oral and intravenous dosage forms of pantoprazole are equivalent in their ability to suppress gastric acid secretion in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2000;95(3):626-633.
357. Metz DC, Soffer E, Forsmark CE, et al. Maintenance oral pantoprazole therapy is effective for patients with Zollinger-Ellison syndrome and idiopathic hypersecretion. Am J Gastroenterol. 2003;98(2):301-307.
358. Metz DC, Comer GM, Soffer E, et al. Three-year oral pantoprazole administration is effective for patients with Zollinger-Ellison syndrome and other hypersecretory conditions. Aliment Pharmacol Ther. 2006;23(3):437-444.
359. Lew EA, Pisegna JR, Starr JA, et al. Intravenous pantoprazole rapidly controls gastric acid hypersecretion in patients with Zollinger-Ellison syndrome. Gastroenterology. 2000;118(4):696-704.
360. Metz DC, Forsmark C, Lew EA, et al. Replacement of oral proton pump inhibitors with intravenous pantoprazole to effectively control gastric acid hypersecretion in patients with Zollinger-Ellison syndrome. Am J Gastroenterol. 2001;96(12):3274-3280.
361. Lima JJ, Thomas CD, Barbarino J, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C19 and Proton Pump Inhibitor Dosing. Clin Pharmacol Ther. 2021;109(6):1417-1423.
362. Institute for Safe Medication Practices (ISMP). ISMP List of Confused Drug Names. ISMP; 2024.
999. By the 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023 Jul;71(7):2052-2081. doi: 10.1111/jgs.18372. Epub 2023 May 4. PMID: 37139824.
8000. Yadlapati R, Gyawali CP, Pandolfino JE; CGIT GERD Consensus Conference Participants. AGA Clinical Practice Update on the Personalized Approach to the Evaluation and Management of GERD: Expert Review. Clin Gastroenterol Hepatol. 2022;20(5):984-994.e1.
8001. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022;117(1):27-56.
Related/similar drugs
Frequently asked questions
- Pantoprazole vs. omeprazole: What's the difference between them?
- Can you take pantoprazole 40 mg twice a day?
- How long can I take pantoprazole?
- Does pantoprazole cause bloating?
More about pantoprazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (434)
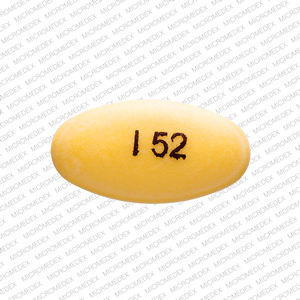
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: proton pump inhibitors
- Breastfeeding
Patient resources
Professional resources
- Pantoprazole prescribing information
- Pantoprazole Granules (FDA)
- Pantoprazole Injection (FDA)
- Pantoprazole Oral Suspension (FDA)