Levocetirizine (Monograph)
Brand name: Xyzal
Drug class: Second Generation Antihistamines
Warning
On May 16, 2025, FDA issued a drug safety communication about the risk of rare, but severe, pruritus after stopping long-term use of oral allergy medications cetirizine or levocetirizine, including both prescription and over-the-counter (OTC) preparations (e.g., Zyrtec, Xyzal, and other trade names). Most patients who experienced pruritus after drug discontinuation reported using these medications daily for more than 3 months; however, some experienced reactions after less than 1 month of use. FDA is adding a warning about this risk to the prescribing information for these medications and is requesting that manufacturers add a warning to the Drug Facts Label of the OTC versions. Patients should contact their healthcare provider if they develop severe itching after stopping prescription or OTC cetirizine or levocetirizine. For additional information, see [Web]
Introduction
Second generation antihistamine; R-enantiomer of cetirizine.
Uses for Levocetirizine
Allergic Rhinitis
Symptomatic relief of seasonal (e.g., hay fever) and perennial (nonseasonal) allergic rhinitis.
Chronic Idiopathic Urticaria
Symptomatic treatment of uncomplicated skin manifestations of chronic idiopathic urticaria.
Levocetirizine Dosage and Administration
Administration
Oral Administration
Administer orally once daily in the evening without regard to meals.
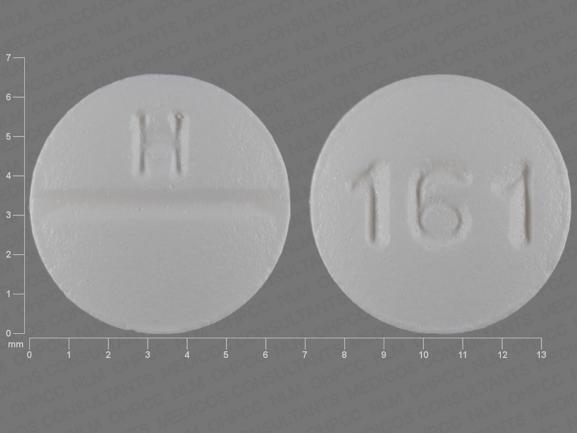
Tablets are scored and can be broken in half (each half providing a dose of 2.5 mg).
Dosage
Available as levocetirizine dihydrochloride; dosage expressed in terms of the salt.
5-mg dose administered as oral solution containing 2.5 mg/5 mL is bioequivalent to 5-mg tablet.
Pediatric Patients
Allergic Rhinitis
Seasonal
OralChildren 2–5 years of age: 1.25 mg once daily (as oral solution). (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.
Perennial
OralChildren 6 months to 5 years of age: 1.25 mg once daily (as oral solution). (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.
Chronic Idiopathic Urticaria
Oral
Children 6 months to 5 years of age: 1.25 mg once daily (as oral solution). (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.
Adults
Allergic Rhinitis
Oral
5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.
Chronic Idiopathic Urticaria
Oral
5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.
Prescribing Limits
Pediatric Patients
Allergic Rhinitis
Seasonal
OralChildren 2–5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence. (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.
Perennial
OralChildren 6 months to 5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence. (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.
Chronic Idiopathic Urticaria
Oral
Children 6 months to 5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence. (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.
Adults
Allergic Rhinitis
Oral
Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.
Chronic Idiopathic Urticaria
Oral
Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.
Special Populations
Hepatic Impairment
No dosage adjustment required.
Renal Impairment
Children 6 months to 11 years of age: Use contraindicated. (See Contraindications under Cautions.)
Adults and children ≥12 years of age: Adjust dosage based on degree of renal impairment. (See Table 1.)
|
Clcr (mL/minute) |
Dosage |
|---|---|
|
50–80 |
2.5 mg once daily |
|
30–50 |
2.5 mg every other day |
|
10–30 |
2.5 mg twice weekly (administered every 3–4 days) |
|
<10 (or undergoing hemodialysis) |
Use contraindicated |
Geriatric Patients
Select dosage with caution (usually starting at low end of dosage range) because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy. (See Geriatric Use under Cautions.)
Cautions for Levocetirizine
Contraindications
-
Known hypersensitivity (e.g., urticaria, anaphylaxis) to levocetirizine or any ingredient in the formulation, or to cetirizine.
-
Adults and children ≥12 years of age with end-stage renal disease (Clcr <10 mL/minute) or undergoing hemodialysis.
-
Pediatric patients 6 months to 11 years of age with renal impairment.
Warnings/Precautions
CNS Effects
Somnolence, fatigue, and asthenia reported. Avoid performing hazardous activities requiring complete mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle). (See Advice to Patients.)
Specific Populations
Pregnancy
Category B.
Lactation
Expected to distribute into milk (since cetirizine is distributed into milk). Use not recommended.
Pediatric Use
Safety not established in children <6 months of age.
Efficacy of 1.25-mg once daily dosage (in pediatric patients 6 months to 5 years of age years of age) and 2.5-mg daily dosage (in pediatric patients 6–11 years of age) for management of allergic rhinitis is based on extrapolation of demonstrated efficacy of 5-mg daily dosage in pediatric patients ≥12 years of age and on pharmacokinetic comparisons in adults and children.
Efficacy of 1.25-mg once daily dosage (in pediatric patients 6 months to 5 years of age years of age), 2.5-mg daily dosage (in pediatric patients 6–11 years of age), and 5-mg daily dosage (in pediatric patients ≥12 years of age) for management of chronic idiopathic urticaria is based on extrapolation of demonstrated efficacy in adults and/or on pharmacokinetic comparisons in adults and children.
Risk of overdosage and toxicity (including death) in children <2 years of age receiving OTC preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection. Clinicians should ask caregivers about use of nonprescription cough and cold preparations to avoid overdosage.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy. (See Geriatric Patients under Dosage and Administration.) Periodic monitoring of renal function may be useful.
Hepatic Impairment
Pharmacokinetics not evaluated, but clearance unlikely to be decreased. (See Elimination under Pharmacokinetics.) Dosage adjustment not necessary.
Renal Impairment
Decreased clearance, resulting in increased risk of adverse effects. Dosage adjustment necessary based on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Children 6–11 months of age (with 1.25-mg once daily dosage): Diarrhea, constipation.
Children 1–5 years of age (with 1.25-mg twice daily dosage): Pyrexia, diarrhea, vomiting, otitis media.
Children 6–12 years of age (with 5-mg daily dosage): Pyrexia, cough, somnolence, epistaxis.
Adults and children ≥12 years of age (with 2.5- or 5-mg daily dosage): Somnolence, nasopharyngitis, fatigue, dry mouth, pharyngitis.
Drug Interactions
No formal drug interaction studies with levocetirizine to date; studies have been performed with racemic cetirizine. (See Specific Drugs under Interactions.)
Does not inhibit CYP isoenzymes 1A2, 2C9, 2C19, 2A1, 2D6, 2E1, or 3A4. Does not induce UGT1A or CYP isoenzymes 1A2, 2C9, or 3A4. Unlikely to produce or be subject to pharmacokinetic interactions associated with metabolic enzyme systems.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Azithromycin |
No clinically important changes in ECG parameters observed following concomitant use with cetirizine, and no clinically important interactions reported following such concomitant use |
|
|
Cimetidine |
No pharmacokinetic interactions observed with cetirizine |
|
|
CNS depressants (e.g., alcohol) |
Possible additive CNS effects |
Avoid concomitant use |
|
Erythromycin |
No clinically important changes in ECG parameters observed following concomitant use with cetirizine, and no clinically important interactions reported following such concomitant use |
|
|
Ketoconazole |
Prolongation of QTc interval (with an increase of 17.4 msec) observed following concomitant administration with cetirizine; no other clinically important interactions reported following such concomitant use |
Not considered clinically important |
|
Pseudoephedrine |
No pharmacokinetic interactions observed with cetirizine |
|
|
Ritonavir |
Increased plasma AUC (42%), increased half-life (53%), and decreased clearance (29%) of cetirizine; disposition of ritonavir not altered following concomitant administration with cetirizine |
|
|
Theophylline |
Decreased clearance (16%) of cetirizine; disposition of theophylline not altered following concomitant administration with cetirizine |
Levocetirizine Pharmacokinetics
Absorption
Bioavailability
Rapidly and extensively absorbed following oral administration, with peak plasma concentration usually attained in 0.9 hour (tablets) or 0.5 hour (oral solution).
Onset
Antihistaminic effects occur within 1 hour. Symptomatic improvement observed as early as 1 day after initiation of therapy for allergic rhinitis or chronic idiopathic urticaria.
Duration
Antihistaminic effects persist for at least 24 hours.
Food
A high-fat meal reduces peak plasma concentration by about 36% and delays time to peak plasma concentration by about 1.25 hours, but does not affect AUC.
Special Populations
In patients with renal impairment, AUC is increased by 1.8-, 3.2-, or 4.3-fold in those with mild, moderate, or severe impairment, respectively; AUC is increased by 5.7-fold in those with end-stage renal disease.
In pediatric patients 6 months to 5 years of age, plasma concentrations following administration of 1.25 mg once daily are similar to those observed in adults receiving 5 mg once daily. In pediatric patients 6–11 years of age, peak plasma concentration and AUC following administration of 5-mg dose are approximately twice that in adults.
Distribution
Extent
Average apparent volume of distribution is 0.4 L/kg, which represents distribution in total body water.
Expected to distribute into milk.
Plasma Protein Binding
Approximately 91–92% (mainly albumin).
Elimination
Metabolism
Metabolized to a limited extent (<14% of dose) by aromatic oxidation, N-dealkylation, O-dealkylation, and taurine conjugation.
Elimination Route
Excreted in urine (85.4%) (via glomerular filtration and active tubular secretion) and in feces (12.9%).
<10% of dose removed by standard 4-hour hemodialysis procedure.
Half-life
Approximately 8–9 hours in adults.
Special Populations
In patients with renal impairment, half-life is increased by 1.4-, 2-, or 2.9-fold in those with mild, moderate, or severe impairment, respectively; half-life is increased by fourfold in those with end-stage renal disease. Total body clearance also progressively decreases based on severity of renal impairment. (See Renal Impairment under Dosage and Administration.)
In pediatric patients 6–11 years of age receiving a single 5-mg dose, total body clearance was 30% greater and elimination half-life 24% shorter than those observed in adults.
In geriatric patients receiving 30 mg once daily for 6 days, total body clearance was 33% lower than that observed in younger adults; however, levocetirizine disposition appears to be dependent on renal function rather than on age.
Stability
Storage
Oral
Tablets and Oral Solution
20–25ºC (may be exposed to 15–30ºC).
Actions
-
Exhibits selective antagonism of peripheral histamine H1-receptors.
-
At half the dosage of cetirizine, appears to be as potent as cetirizine in inhibiting histamine-induced sneezing, increased nasal airway resistance, and skin wheal and flare.
-
Has been shown to exhibit greater and more consistent inhibition of histamine-induced wheal and flare compared with other antihistamines (e.g., desloratadine, fexofenadine, loratadine). Clinical relevance of histamine wheal skin testing is unknown.
Advice to Patients
-
Importance of taking only as prescribed; do not exceed prescribed dosage because of increased risk of somnolence.
-
Risk of somnolence; avoid performing activities requiring complete mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle).
-
Avoid concomitant use with alcohol or other CNS depressants.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2.5 mg/5 mL |
Xyzal |
UCB |
|
Tablets, film-coated |
5 mg |
Xyzal (scored) |
UCB |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Is it OK to take antihistamines every day?
- Is Xyzal available over-the-counter?
- Which antihistamines make you drowsy?
More about levocetirizine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (348)
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antihistamines
- Breastfeeding
- En español