Levocetirizine (Monograph)
Brand name: Xyzal
Drug class: Second Generation Antihistamines
Warning
On May 16, 2025, FDA issued a drug safety communication about the risk of rare, but severe, pruritus after stopping long-term use of oral allergy medications cetirizine or levocetirizine, including both prescription and over-the-counter (OTC) preparations (e.g., Zyrtec, Xyzal, and other trade names). Most patients who experienced pruritus after drug discontinuation reported using these medications daily for more than 3 months; however, some experienced reactions after less than 1 month of use. FDA is adding a warning about this risk to the prescribing information for these medications and is requesting that manufacturers add a warning to the Drug Facts Label of the OTC versions. Patients should contact their healthcare provider if they develop severe itching after stopping prescription or OTC cetirizine or levocetirizine. For additional information, see [Web]
Introduction
Second generation antihistamine;34 R-enantiomer of cetirizine.1 2 3 4 5 7 14 15
Uses for Levocetirizine
Allergic Rhinitis
Symptomatic relief of seasonal (e.g., hay fever) and perennial (nonseasonal) allergic rhinitis.1 5 12 15 32 37 38 39 40
Chronic Idiopathic Urticaria
Symptomatic treatment of uncomplicated skin manifestations of chronic idiopathic urticaria.1 5 13 14 41
Levocetirizine Dosage and Administration
Administration
Oral Administration
Administer orally once daily in the evening without regard to meals.1
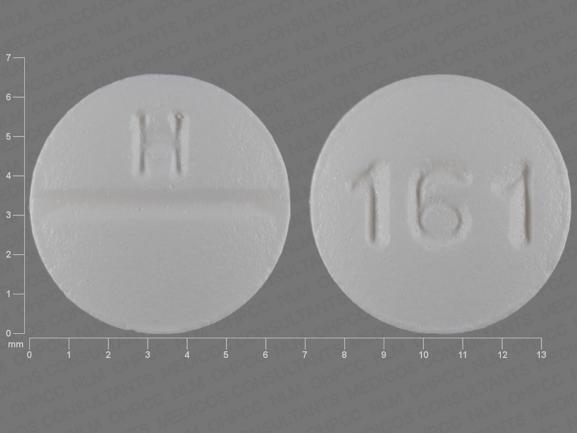
Tablets are scored and can be broken in half (each half providing a dose of 2.5 mg).1
Dosage
Available as levocetirizine dihydrochloride; dosage expressed in terms of the salt.1
5-mg dose administered as oral solution containing 2.5 mg/5 mL is bioequivalent to 5-mg tablet.1
Pediatric Patients
Allergic Rhinitis
Seasonal
OralChildren 2–5 years of age: 1.25 mg once daily (as oral solution).1 (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.1
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.1
Perennial
OralChildren 6 months to 5 years of age: 1.25 mg once daily (as oral solution).1 (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.1
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.1
Chronic Idiopathic Urticaria
Oral
Children 6 months to 5 years of age: 1.25 mg once daily (as oral solution).1 (See Pediatric Use under Cautions.)
Children 6–11 years of age: 2.5 mg once daily.1
Children ≥12 years of age: 5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.1
Adults
Allergic Rhinitis
Oral
5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.1
Chronic Idiopathic Urticaria
Oral
5 mg once daily; alternatively, 2.5 mg once daily may be adequate for some patients.1
Prescribing Limits
Pediatric Patients
Allergic Rhinitis
Seasonal
OralChildren 2–5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence.1 (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.1
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.1
Perennial
OralChildren 6 months to 5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence.1 (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.1
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.1
Chronic Idiopathic Urticaria
Oral
Children 6 months to 5 years of age: Maximum 1.25 mg daily; higher dosages associated with increased risk of somnolence.1 (See Absorption: Special Populations, under Pharmacokinetics.)
Children 6–11 years of age: Maximum 2.5 mg daily; higher dosages associated with increased risk of somnolence.1
Children ≥12 years of age: Maximum 5 mg daily; higher dosages associated with increased risk of somnolence.1
Adults
Allergic Rhinitis
Oral
Maximum 5 mg daily;1 higher dosages associated with increased risk of somnolence.1 15
Chronic Idiopathic Urticaria
Oral
Maximum 5 mg daily;1 higher dosages associated with increased risk of somnolence.1 15
Special Populations
Hepatic Impairment
No dosage adjustment required.1
Renal Impairment
Children 6 months to 11 years of age: Use contraindicated.1 (See Contraindications under Cautions.)
Adults and children ≥12 years of age: Adjust dosage based on degree of renal impairment. (See Table 1.)
|
Clcr (mL/minute) |
Dosage |
|---|---|
|
50–80 |
2.5 mg once daily |
|
30–50 |
2.5 mg every other day |
|
10–30 |
2.5 mg twice weekly (administered every 3–4 days) |
|
<10 (or undergoing hemodialysis) |
Use contraindicated |
Geriatric Patients
Select dosage with caution (usually starting at low end of dosage range) because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.1 (See Geriatric Use under Cautions.)
Cautions for Levocetirizine
Contraindications
-
Known hypersensitivity (e.g., urticaria, anaphylaxis) to levocetirizine or any ingredient in the formulation, or to cetirizine.1
-
Adults and children ≥12 years of age with end-stage renal disease (Clcr <10 mL/minute) or undergoing hemodialysis.1
-
Pediatric patients 6 months to 11 years of age with renal impairment.1
Warnings/Precautions
CNS Effects
Somnolence, fatigue, and asthenia reported.1 7 12 13 15 Avoid performing hazardous activities requiring complete mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle).1 (See Advice to Patients.)
Specific Populations
Pregnancy
Category B.1
Lactation
Expected to distribute into milk (since cetirizine is distributed into milk).1 Use not recommended.1
Pediatric Use
Safety not established in children <6 months of age.1 36
Efficacy of 1.25-mg once daily dosage (in pediatric patients 6 months to 5 years of age years of age) and 2.5-mg daily dosage (in pediatric patients 6–11 years of age) for management of allergic rhinitis is based on extrapolation of demonstrated efficacy of 5-mg daily dosage in pediatric patients ≥12 years of age and on pharmacokinetic comparisons in adults and children.1
Efficacy of 1.25-mg once daily dosage (in pediatric patients 6 months to 5 years of age years of age), 2.5-mg daily dosage (in pediatric patients 6–11 years of age), and 5-mg daily dosage (in pediatric patients ≥12 years of age) for management of chronic idiopathic urticaria is based on extrapolation of demonstrated efficacy in adults and/or on pharmacokinetic comparisons in adults and children.1
Risk of overdosage and toxicity (including death) in children <2 years of age receiving OTC preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection.a b Clinicians should ask caregivers about use of nonprescription cough and cold preparations to avoid overdosage.a
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.1 Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.1 (See Geriatric Patients under Dosage and Administration.) Periodic monitoring of renal function may be useful.1
Hepatic Impairment
Pharmacokinetics not evaluated, but clearance unlikely to be decreased.1 (See Elimination under Pharmacokinetics.) Dosage adjustment not necessary.1
Renal Impairment
Decreased clearance, resulting in increased risk of adverse effects.1 Dosage adjustment necessary based on degree of renal impairment.1 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Children 6–11 months of age (with 1.25-mg once daily dosage): Diarrhea,1 constipation.1
Children 1–5 years of age (with 1.25-mg twice daily dosage): Pyrexia,1 diarrhea,1 vomiting,1 otitis media.1
Children 6–12 years of age (with 5-mg daily dosage): Pyrexia,1 cough,1 somnolence,1 epistaxis.1 6
Adults and children ≥12 years of age (with 2.5- or 5-mg daily dosage): Somnolence,1 5 15 32 nasopharyngitis,1 fatigue,1 5 15 32 dry mouth,1 5 15 pharyngitis.1 32
Drug Interactions
No formal drug interaction studies with levocetirizine to date; studies have been performed with racemic cetirizine.1 (See Specific Drugs under Interactions.)
Does not inhibit CYP isoenzymes 1A2, 2C9, 2C19, 2A1, 2D6, 2E1, or 3A4.1 5 Does not induce UGT1A or CYP isoenzymes 1A2, 2C9, or 3A4.1 Unlikely to produce or be subject to pharmacokinetic interactions associated with metabolic enzyme systems.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Azithromycin |
No clinically important changes in ECG parameters observed following concomitant use with cetirizine, and no clinically important interactions reported following such concomitant use1 16 17 20 21 |
|
|
Cimetidine |
No pharmacokinetic interactions observed with cetirizine1 |
|
|
CNS depressants (e.g., alcohol) |
Possible additive CNS effects1 |
Avoid concomitant use1 |
|
Erythromycin |
No clinically important changes in ECG parameters observed following concomitant use with cetirizine, and no clinically important interactions reported following such concomitant use1 16 17 20 21 |
|
|
Ketoconazole |
Prolongation of QTc interval (with an increase of 17.4 msec) observed following concomitant administration with cetirizine; no other clinically important interactions reported following such concomitant use1 16 21 22 |
|
|
Pseudoephedrine |
No pharmacokinetic interactions observed with cetirizine1 16 17 |
|
|
Ritonavir |
Increased plasma AUC (42%), increased half-life (53%), and decreased clearance (29%) of cetirizine; disposition of ritonavir not altered following concomitant administration with cetirizine1 |
|
|
Theophylline |
Decreased clearance (16%) of cetirizine; disposition of theophylline not altered following concomitant administration with cetirizine1 16 17 |
Levocetirizine Pharmacokinetics
Absorption
Bioavailability
Rapidly and extensively absorbed following oral administration, with peak plasma concentration usually attained in 0.9 hour (tablets) or 0.5 hour (oral solution).1 5 18
Onset
Antihistaminic effects occur within 1 hour.1 2 7 19 Symptomatic improvement observed as early as 1 day after initiation of therapy for allergic rhinitis1 7 8 15 or chronic idiopathic urticaria.13 14 33
Duration
Antihistaminic effects persist for at least 24 hours.1 2 6 7 8 15 19
Food
A high-fat meal reduces peak plasma concentration by about 36% and delays time to peak plasma concentration by about 1.25 hours, but does not affect AUC.1
Special Populations
In patients with renal impairment, AUC is increased by 1.8-, 3.2-, or 4.3-fold in those with mild, moderate, or severe impairment, respectively; AUC is increased by 5.7-fold in those with end-stage renal disease.1
In pediatric patients 6 months to 5 years of age, plasma concentrations following administration of 1.25 mg once daily are similar to those observed in adults receiving 5 mg once daily.1 In pediatric patients 6–11 years of age, peak plasma concentration and AUC following administration of 5-mg dose are approximately twice that in adults.1
Distribution
Extent
Average apparent volume of distribution is 0.4 L/kg, which represents distribution in total body water.1
Expected to distribute into milk.1
Plasma Protein Binding
Approximately 91–92%1 (mainly albumin).5 33
Elimination
Metabolism
Metabolized to a limited extent (<14% of dose) by aromatic oxidation, N-dealkylation, O-dealkylation, and taurine conjugation.1
Elimination Route
Excreted in urine (85.4%) (via glomerular filtration and active tubular secretion) and in feces (12.9%).1 18
<10% of dose removed by standard 4-hour hemodialysis procedure.1
Half-life
Approximately 8–9 hours in adults.1
Special Populations
In patients with renal impairment, half-life is increased by 1.4-, 2-, or 2.9-fold in those with mild, moderate, or severe impairment, respectively; half-life is increased by fourfold in those with end-stage renal disease.1 Total body clearance also progressively decreases based on severity of renal impairment.1 (See Renal Impairment under Dosage and Administration.)
In pediatric patients 6–11 years of age receiving a single 5-mg dose, total body clearance was 30% greater and elimination half-life 24% shorter than those observed in adults.1
In geriatric patients receiving 30 mg once daily for 6 days, total body clearance was 33% lower than that observed in younger adults; however, levocetirizine disposition appears to be dependent on renal function rather than on age.1
Stability
Storage
Oral
Tablets and Oral Solution
20–25ºC (may be exposed to 15–30ºC).1 33
Actions
-
Exhibits selective antagonism of peripheral histamine H1-receptors.1
-
At half the dosage of cetirizine, appears to be as potent as cetirizine in inhibiting histamine-induced sneezing,4 increased nasal airway resistance,3 4 5 and skin wheal and flare.2 3 5
-
Has been shown to exhibit greater and more consistent inhibition of histamine-induced wheal and flare compared with other antihistamines (e.g., desloratadine, fexofenadine, loratadine).5 7 19 Clinical relevance of histamine wheal skin testing is unknown.1
Advice to Patients
-
Importance of taking only as prescribed; do not exceed prescribed dosage because of increased risk of somnolence.1
-
Risk of somnolence;1 7 12 15 avoid performing activities requiring complete mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle).1
-
Avoid concomitant use with alcohol or other CNS depressants.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.1
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2.5 mg/5 mL |
Xyzal |
UCB |
|
Tablets, film-coated |
5 mg |
Xyzal (scored) |
UCB |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. UCB Inc. Xyzal (levocetirizine dihydrochloride) tablets and oral solution prescribing information. 2010 Dec. From website. http://www.xyzal.com
2. Devalia JL, De Vos C, Hanotte F et al. A randomized, double-blind, crossover comparison among cetirizine, levocetirizine, and ucb 28557 on histamine-induced cutaneous responses in healthy adult volunteers. Allergy. 2001; 56:50-57. https://pubmed.ncbi.nlm.nih.gov/11167352
3. Tillement JP, Testa B, Brée F. Compared pharmacological characteristics in humans of racemic cetirizine and levocetirizine, two histamine H1-receptor antagonists. Biochem Pharmacol. 2003; 66:1123-6. https://pubmed.ncbi.nlm.nih.gov/14505791
4. Wang DY, Hanotte F, De Vos C et al. Effect of cetirizine, levocetirizine, and dextrocetirizine on histamine-induced nasal response in healthy adult volunteers. Allergy. 2001; 56:339-43. https://pubmed.ncbi.nlm.nih.gov/11284803
5. Ciprandi G, Cirillo I, Vizzaccaro A, Tosca MA. Levocetirizine improves nasal obstruction and modulates cytokine pattern in patients with seasonal allergic rhinitis: a pilot study. Clin Exp Allergy. 2004; 34(6): 958-964. https://pubmed.ncbi.nlm.nih.gov/15196286
6. de Blic J, Wahn U, Billard E et al. Levocetirizine in children: evidenced efficacy and safety in a 6-week randomized seasonal allergic rhinitis trial. Pediatr Allergy Immunol. 2005; 16:267-75. https://pubmed.ncbi.nlm.nih.gov/15853959
7. Day JH, Briscoe MP, Rafeiro E et al. Comparative clinical efficacy, onset and duration of action of levocetirizine and desloratadine for symptoms of seasonal allergic rhinitis in subjects evaluated in the Environmental Exposure Unit (EEU). Int J Clin Pract. 2004; 58:109-18. https://pubmed.ncbi.nlm.nih.gov/15055856
8. Horak F, Zieglmayer PU, Zieglmayer R et al. Levocetirizine has a longer duration of action on improving total nasal symptoms score than fexofenadine after single administration. Br J Clin Pharmacol. 2005; 60:24-31. https://pubmed.ncbi.nlm.nih.gov/15963090
9. Ciebiada M, Gorska-Ciebiada M, DuBuske LM et al. Montelukast with desloratadine or levocetirizine for the treatment of persistent allergic rhinitis. Ann Allergy Asthma Immunol. 2006; 97:664-71. https://pubmed.ncbi.nlm.nih.gov/17165277
10. Pasquali M, Baiardini I, Rogkakou A et al. Levocetirizine in persistent allergic rhinitis and asthma: effects on symptoms, quality of life and inflammatory parameters. Clin Exp Allergy. 2006; 36:1161-7. https://pubmed.ncbi.nlm.nih.gov/16961716
11. Potter PC for the Paediatric Levocetirizine Study Group. Efficacy and safety of levocetirizine on symptoms and health-related quality of life of children with perennial allergic rhinitis: a double-blind, placebo-controlled randomized clinical trial. Ann Allergy Asthma Immunol. 2005; 95:175-80. https://pubmed.ncbi.nlm.nih.gov/16136768
12. Potter PC for the Study Group. Levocetirizine is effective for symptom relief including nasal congestion in adolescent and adult (PAR) sensitized to house dust mites. Allergy. 2003; 58:893-9. https://pubmed.ncbi.nlm.nih.gov/12911418
13. Kapp A, Pichler WJ. Levocetirizine is an effective treatment in patients suffering from chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled, parallel, multicenter study. Int J Dermatol. 2006; 45:469-74. https://pubmed.ncbi.nlm.nih.gov/16650180
14. Nettis E, Colanardi MC, Barra L et al. Levocetirizine in the treatment of chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled study. Br J Dermatol. 2006; 154:533-8. https://pubmed.ncbi.nlm.nih.gov/16445787
15. Leynadier F, Mees K, Arendt C et al. Efficacy and safety of levocetirizine in seasonal allergic rhinitis. Acta Otorhinolaryngol Belg. 2001; 55:305-12. https://pubmed.ncbi.nlm.nih.gov/11859651
16. Pfizer Labs. Zyrtec (cetirizine hydrochloride) tablets and syrup prescribing information. New York, NY; 2004 Jul.
17. Pfizer Laboratories. Zyrtec (cetirizine hydrochloride) tablets product monograph. New York, NY: Undated.
18. Benedetti MS, Plisnier M, Kaise J et al. Absorption, distribution, metabolism and excretion of [14C] levocetirizine, the R enantiomer of cetirizine, in healthy volunteers. Eur J Clin Pharmacol. 2001; 57:571-82. https://pubmed.ncbi.nlm.nih.gov/11758635
19. Grant JA, Riethuisen JM, Moulaert B et al. A double-blind, randomized, single-dose, crossover comparison of levocetirizine with ebastine, fexofenadine, loratadine, mizolastine, and placebo: suppression of histamine-induced wheal-and-flare response during 24 hours in healthy male subjects. Ann Allergy Asthma Immunol. 2002; 88:190-7. https://pubmed.ncbi.nlm.nih.gov/11868924
20. Simons FER. H1-Receptor antagonists: comparative tolerability and safety. Drug Saf. 1994; 10:350-80. https://pubmed.ncbi.nlm.nih.gov/7913608
21. Reviewers’ comments (for cetirizine).
22. Pfizer Inc. Manufacturer’s comments (for cetirizine).
23. Borge PA. Problems in allergic rhinitis. Arzneimittelforschung. 1982; 32:1199-201. https://pubmed.ncbi.nlm.nih.gov/6891258
24. Anon. Treatment of seasonal and perennial rhinitis. BMJ. 1981; 283:808-10. https://pubmed.ncbi.nlm.nih.gov/6117350
25. Food and Drug Administration. Over-the-counter drugs: establishment of a monograph for OTC cold, cough, allergy, bronchodilator and antiasthmatic products. [21 CFR 341] Fed Regist. 1976; 41:38312-424.
26. Douglas WW. Histamine and 5-hydroxytryptamine (serotonin) and their antagonists. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacologic basis of therapeutics. 7th ed. New York: Macmillan Publishing Company; 1985:605-38.
27. Cirillo VJ, Tempero KF. The pharmacology and therapeutic use of H1 and H2 antihistamines. In: Miller RR, Greenblatt DJ, eds. Drug therapy reviews. Vol 2. New York: Elsevier/North Holland Inc; 1979:24-47.
28. AMA Division of Drugs. AMA drug evaluations. 5th ed. Chicago: American Medical Association; 1983:1465-79.
29. Church JA. Allergic rhinitis: diagnosis and management. Clin Pediatr (Philadelphia). 1980; 19:655-9.
30. Food and Drug Administration. Cold, cough, allergy, bronchodilator, and antiasthmatic drug products for over-the-counter human use; tentative final monograph for OTC antihistamine drug products. [21 FR Part 341] Fed Regist. 1985; 50:2200-18.
31. Holgate S. Comparative trial of two non-sedative H1 antihistamines, terfenadine and astemizole, for hay fever. Thorax. 1985; 40:399.
32. Bachert C, Bousquet J, Canonica W et al for the XPERT Study Group. Levocetirizine improves quality of life and reduces costs in long-term management of persistent allergic rhinitis. J Allergy Clin Immunol. 2004; 114:838-44. https://pubmed.ncbi.nlm.nih.gov/15480324
33. UCB, Inc., Smyrna, GA: Personal communication.
34. Anon. Drugs for allergic disorders. Treat Guidel Med Lett. 2007; 5:71-80.
36. Hampel F, Ratner P, Haeusler JM. Safety and tolerability of levocetirizine dihydrochloride in infants and children with allergic rhinitis or chronic urticaria. Allergy Asthma Proc. 2010 Jul-Aug; 31:290-5.
37. Segall N, Gawchik S, Georges G et al. Efficacy and safety of levocetirizine in improving symptoms and health-related quality of life in US adults with seasonal allergic rhinitis: a randomized, placebo-controlled study. Ann Allergy Asthma Immunol. 2010; 104:259-67. https://pubmed.ncbi.nlm.nih.gov/20377116
38. Day JH, Briscoe MP, Ratz JD. Efficacy of levocetirizine compared with montelukast in subjects with ragweed-induced seasonal allergic rhinitis in the Environmental Exposure Unit. Allergy Asthma Proc. 2008 May-Jun; 29:304-12.
39. Patel P, Patel D. Efficacy comparison of levocetirizine vs montelukast in ragweed sensitized patients. Ann Allergy Asthma Immunol. 2008; 101:287-94. https://pubmed.ncbi.nlm.nih.gov/18814452
40. Walter Canonica G, Bousquet J, Van Hammée G et al. Levocetirizine improves health-related quality of life and health status in persistent allergic rhinitis. Respir Med. 2006; 100:1706-15. https://pubmed.ncbi.nlm.nih.gov/16723217
41. Potter PC, Kapp A, Maurer M et al. Comparison of the efficacy of levocetirizine 5 mg and desloratadine 5 mg in chronic idiopathic urticaria patients. Allergy. 2009; 64:596-604. https://pubmed.ncbi.nlm.nih.gov/19053988
a. Srinivasan A, Budnitz D, Shehab N et al. Infant deaths associated with cough and cold medications—two states, 2005. MMWR Morb Mortal Wkly Rep. 2007; 56:1-4. https://pubmed.ncbi.nlm.nih.gov/17218934
b. Food and Drug Administration. Cough and cold medications in children less than two years of age. Rockville, MD; 2007 Jan 12. From FDA website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm150441.htm
Related/similar drugs
Frequently asked questions
- Is it OK to take antihistamines every day?
- Is Xyzal available over-the-counter?
- Which antihistamines make you drowsy?
More about levocetirizine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (348)
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antihistamines
- Breastfeeding
- En español