Aspirin (Monograph)
Brand names: Ascriptin, Aspergum, Bayer, Bufferin, Easprin,
... show all 11 brands
Drug class: Salicylates
- Antithrombotic Agents
- Platelet-aggregation Inhibitors
Aspirin (Systemic) is also contained as an ingredient in the following combinations:
Acetaminophen and Aspirin
Acetaminophen, Aspirin, and Caffeine
Oxycodone and Aspirin
Pentazocine Hydrochloride and Aspirin
Propoxyphene Hydrochloride, Aspirin, and Caffeine
Introduction
NSAIA; salicylate ester of acetic acid.a
Uses for Aspirin
Pain
Symptomatic relief of mild to moderate pain.a
Self-medication in children for the temporary relief of minor aches and pains and headache.841
Self-medication in adolescents and adults for the temporary relief of minor aches and pains associated with headache, common cold, toothache, muscular aches, backache, arthritis, menstrual cramps,836 and sore throat.837 840
Self-medication in fixed combination with acetaminophen and caffeine for the temporary relief of mild to moderate pain associated with migraine headache;701 702 703 also can be used for the treatment of severe migraine headache if previous attacks have responded to similar non-opiate analgesics or NSAIAs.701 702 703 778
Fever
Self-medication for reduction of fever associated with colds, sore throats, and teething.837 841 (See Contraindications and see Pediatric Use under Cautions.)
Inflammatory Diseases
Symptomatic treatment of rheumatoid arthritis, juvenile rheumatoid arthritis, osteoarthritis, spondyloarthropathies, and systemic lupus erythematosus (SLE).906 938 943 a
Rheumatic Fever
Symptomatic treatment of rheumatic fever† [off-label].a A drug of choice in patients with mild carditis (without cardiomegaly or CHF, with or without polyarthritis) or with polyarthritis only.h
Transient Ischemic Attacks and Ischemic Stroke
Reduction of the risk of recurrent TIAs or stroke or of death in patients with a history of TIAs or ischemic stroke (secondary prevention).646 682 842 906 938 1009
Also used in fixed combination with extended-release dipyridamole to reduce the risk of recurrent stroke, death from all vascular causes, or nonfatal MI in patients who have had TIAs or completed ischemic stroke caused by thrombosis.738 739 743 1009
The American College of Chest Physicians (ACCP), the American Stroke Association (ASA), and AHA consider aspirin or the combination of aspirin and extended-release dipyridamole acceptable antiplatelet regimens for secondary prevention of noncardioembolic ischemic stroke and TIAs; other options include cilostazol or clopidogrel.990 1009 When selecting an appropriate antiplatelet regimen, consider factors such as the patient's individual risk for recurrent stroke, tolerance, and cost of the different agents.990
Oral anticoagulation (e.g., dabigatran, warfarin) rather than antiplatelet therapy is recommended in patients with a history of ischemic stroke or TIA and concurrent atrial fibrillation; however, in patients who cannot take or choose not to take oral anticoagulants (e.g., those with difficulty maintaining stable INRs, compliance issues, dietary restrictions, or cost limitations), dual antiplatelet therapy with aspirin and clopidogrel is recommended.1009
Also used for acute treatment of ischemic stroke in children† [off-label].1013
Coronary Artery Disease
Recommended by AHA and the American College of Cardiology Foundation (ACCF) for reduction of the risk of vascular events (e.g., stroke, recurrent MI) in all patients with CAD, unless contraindicated.992
Recommended by American Diabetes Association (ADA) for secondary prevention of cardiovascular events in patients with diabetes mellitus and a history of atherosclerotic cardiovascular disease (ASCVD).1116
ST-Segment-Elevation MI (STEMI)
Reduction of the risk of stroke, recurrent infarction, and death in patients with STEMI.527 579 842 992 1010
Use in conjunction with a P2Y12 platelet adenosine diphosphate (ADP)-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor).527 992 993 994 1010
The addition of warfarin to antiplatelet therapy is recommended in patients with STEMI who have indications for anticoagulation (e.g., atrial fibrillation, left ventricular dysfunction, cerebral emboli, extensive wall-motion abnormality, mechanical heart valves).993 996 1007 1010
Primary Prevention of Ischemic Cardiac Events
Use of aspirin for primary prevention of cardiovascular disease remains controversial;1112 may reduce the risk of a first cardiac event (e.g., STEMI)† [off-label] in certain patient populations (primary prevention).1110 1117 1118 1119 Balance of risks and benefits is most favorable in patients at higher ASCVD risk who have a low risk of bleeding.1110 1111 1113 1114 1115
Some experts recommend reserving low-dose aspirin for primary prevention in adults 40–70 years of age who have a higher risk of cardiovascular disease without an increased risk of bleeding (e.g., history of previous GI bleed, peptic ulcer disease, thrombocytopenia, coagulopathy, chronic kidney disease, concomitant use of drugs that increase bleeding risk [e.g., NSAIAs, corticosteroids, direct oral anticoagulants, warfarin]).1110 1111
Consider totality of patient risk factors when determining risk for ASCVD, (e.g., strong family history of premature MI; inability to achieve lipid, BP, or blood glucose targets; substantial elevation in coronary artery calcium score) in conjunction with patient and clinician preferences.1110 1118 1119 High-risk patients also include adults 40–70 years of age without diabetes mellitus who have a 10-year ASCVD risk ≥20% and those with diabetes mellitus who have a 10-year ASCVD risk ≥10%.1111
The US Preventive Services Task Force (USPSTF) states that the beneficial effects of aspirin for primary prevention of cardiovascular disease are modest and occur at daily dosages of ≤100 mg, with a potentially greater relative benefit for MI prevention in older adults.1117
ADA states may be considered for primary prevention in patients with type 1 or type 2 diabetes mellitus who are at high risk for cardiovascular events (i.e., familial history of premature ASCVD, smoking, hypertension, chronic kidney disease/albuminuria, elevated blood cholesterol or triglyceride concentrations) after evaluating risks versus benefits.1116
Not currently recommended for primary prevention in patients with a low risk of ASCVD.1110 Not routinely recommended for primary prevention in individuals <40 or >70 years of age.1110
Non-ST-Segment-Elevation Acute Coronary Syndromes (NSTE ACS)
Reduction of the risk of death and/or nonfatal MI in patients with NSTE ACS (unstable angina or non-ST-segment-elevation MI [NSTEMI]).581 613 614 615 616 617 618 619 620 621 682 684 728 736 906 938 1100
Dual-drug antiplatelet therapy with aspirin and a P2Y12-receptor antagonist (e.g., clopidogrel, ticagrelor) is considered part of the current standard of care for treatment and secondary prevention in patients with NSTE ACS.992 993 994 1010
Experts state that aspirin should be administered as soon as possible after presentation (and continued indefinitely) in all patients with NSTE ACS unless contraindicated; in addition, a P2Y12-receptor antagonist should be administered for up to 12 months.1100
Chronic Stable Angina
Reduction of the risk of MI and/or sudden death in patients with chronic stable angina.646 680 728 736 822 906 938
Experts recommend that aspirin therapy (75–162 mg daily) be continued indefinitely in patients with stable ischemic heart disease who do not have contraindications.1101
Percutaneous Coronary Intervention and Revascularization Procedures
Reduction of cardiovascular risks (e.g., early ischemic complications, graft closure) in patients with ACS undergoing PCI (e.g., coronary angioplasty, coronary artery stent implantation)646 866 887 888 889 992 993 994 1010 or CABG.646 683 687 781 782
Pretreatment with aspirin prior to PCI recommended by ACCF, AHA, and the Society for Cardiovascular Angiography and Interventions (SCAI).994 Adjunctive therapy with a P2Y12-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor) also recommended in patients undergoing PCI with stent placement.994
Continue low-dose aspirin therapy indefinitely (as part of dual-drug antiplatelet therapy with a P2Y12-receptor antagonist for at least 12 months and possibly longer) as secondary prevention against cardiovascular events, including stent thrombosis, following PCI.993 994 1010 1019 1020
Embolism Associated with Atrial Fibrillation
Used as an alternative or adjunct to warfarin therapy for reduction of the incidence of thromboembolism in selected patients with chronic atrial fibrillation† [off-label].749 880 999 1007
ACCP, ASA, ACC, AHA, and other experts currently recommend that antithrombotic therapy be given to all patients with nonvalvular atrial fibrillation (i.e., atrial fibrillation in the absence of rheumatic mitral stenosis, a prosthetic heart valve, or mitral valve repair) who are considered to be at increased risk of stroke, unless such therapy is contraindicated.989 990 999 1007 1017 1021 1022 1023
Choice of antithrombotic therapy is based on patient's risk for stroke and bleeding.999 1007 1021 1022 1023 In general, oral anticoagulant therapy (traditionally warfarin) is recommended in patients with high risk for stroke and acceptably low risk of bleeding, while aspirin or no antithrombotic therapy may be considered in patients at low risk of stroke.999 1007 1017 1021 1022 1023
In patients with atrial fibrillation at increased risk of stroke who cannot take or choose not to take oral anticoagulants for reasons other than concerns about major bleeding (e.g., those with difficulty maintaining stable INRs), combination therapy with clopidogrel and aspirin rather than aspirin alone is recommended.998 1007
Antithrombotic therapy in patients with atrial flutter generally managed in the same manner as in patients with atrial fibrillation.999 1007
Peripheral Arterial Disease
Has been used for primary and secondary prophylaxis of cardiovascular events in patients with peripheral arterial disease, including those with intermittent claudication or carotid stenosis and those undergoing revascularization procedures (peripheral artery percutaneous transluminal angioplasty or peripheral arterial bypass graft surgery).1011
ACCP suggests the use of low-dose aspirin for primary prevention in patients with asymptomatic peripheral arterial disease.1011
For patients with symptomatic peripheral arterial disease or those undergoing revascularization procedures, single-drug antiplatelet therapy with aspirin or clopidogrel generally is recommended.1011
Valvular Heart Disease
Recommended by ACC and AHA for use in selected patients with mitral valve prolapse and atrial fibrillation, and also in symptomatic patients with mitral valve prolapse who experience TIAs.996
Prosthetic Heart Valves
Used for the prevention of thromboembolism in selected patients with prosthetic heart valves† [off-label].996 1008
ACCP and ACC/AHA suggest the use of low-dose aspirin for initial (i.e., first 3 months after valve insertion) and long-term antithrombotic therapy in patients with a bioprosthetic heart valve in the aortic position who are in sinus rhythm and have no other indications for warfarin.996 1008 Aspirin also may be considered after initial (3 months) warfarin therapy in patients with a bioprosthetic heart valve in the mitral position who are in sinus rhythm.1008
Addition of an antiplatelet agent such as low-dose aspirin to warfarin therapy recommended in all patients with mechanical heart valves who are at low risk of bleeding.996 1008 Combination therapy with aspirin and warfarin also recommended in patients with bioprosthetic heart valves who have additional risk factors for thrombosis (e.g., atrial fibrillation, previous thromboembolism, left ventricular dysfunction, hypercoagulable condition).996
May be added to therapy with a low molecular weight heparin (LMWH) or heparin (referring throughout this monograph to unfractionated heparin) in pregnant women with prosthetic heart valves† who are at high risk for thrombosis.1012
Thrombosis Associated with Fontan Procedure in Children
Has been used for prevention of thromboembolic complications following Fontan procedure† (definitive palliative surgical treatment for most congenital univentricular heart lesions) in children.1013
Thromboprophylaxis in Orthopedic Surgery
Has been used for the prevention of venous thromboembolism in patients undergoing major orthopedic surgery (total-hip replacement, total-knee replacement, or hip-fracture surgery†).1003 Aspirin generally not considered the drug of choice for this use;1003 however, some evidence suggests some benefit over placebo or no antithrombotic prophylaxis in patients undergoing major orthopedic surgery.953 954 1003
ACCP considers aspirin an acceptable option for pharmacologic thromboprophylaxis in patients undergoing major orthopedic surgery.1003
When selecting an appropriate thromboprophylaxis regimen, consider factors such as relative efficacy and bleeding risk in addition to other logistics and compliance issues.1003
Thromboprophylaxis in General Surgery
Has been used for thromboprophylaxis in patients undergoing general (e.g., abdominal) surgery who are at high risk of venous thromboembolism;1002 however, generally recommended as an alternative to LMWHs and low-dose heparin.1002
Pericarditis
Drug of choice for the management of pain associated with acute pericarditis† following MI.527
Kawasaki Disease
Treatment of Kawasaki disease; used in conjunction with immune globulin IV (IGIV).636 637 638 1013
Complications of Pregnancy
Has been used alone or in combination with other drugs (e.g., heparin, corticosteroids, immune globulin) for prevention of complications of pregnancy† (e.g., preeclampsia, pregnancy loss in women with a history of antiphospholipid syndrome and recurrent fetal loss).594 595 596 597 599 600 601 605 626 627 628 648 650 651 652 653 654 705 706 707 708 709 710 711 712 713 714 715 726 817 857 1012
Low-dose aspirin in combination with sub-Q heparin or an LMWH is recommended by ACCP in women with antiphospholipid antibody (APLA) syndrome† and a history of multiple (≥3) pregnancy losses.1012
Routine use of aspirin prophylaxis to reduce the incidence and severity of preeclampsia (even in patients at increased risk of preeclampsia) generally not recommended; 705 706 707 712 713 715 can consider prophylaxis in women with prior severe or early-onset preeclampsia, chronic hypertension, severe diabetes, or moderate to severe renal disease.815 816 817 In women at high risk for preeclampsia, ACCP recommends low-dose aspirin during pregnancy, starting from the second trimester.1012 (See Pregnancy under Cautions.)
Prevention of Cancer
Limited data (observational studies) suggest that aspirin or other NSAIAs may reduce the risk of various cancers† (e.g., colorectal, breast, gastric cancer);864 870 871 872 873 such results generally not confirmed in randomized controlled trials.864 874 875 876
Regular use (e.g., daily) associated with a reduction in the risk of recurrent colorectal adenomas and colorectal cancer† in some studies.789 790 791 792 793 794 795 796 797 798 799 800 801 802 803 804 805 806 807 808 809 810 811 812 813 814 815 Beneficial effects of NSAIAs in reducing colorectal cancer risk dissipate following discontinuance of such therapy.791 792 793 794 795 Preventive therapy with aspirin currently not recommended because aspirin does not completely eliminate adenomas; aspirin therapy should not be considered a replacement for colorectal cancer screening and surveillance.790 793 794 795 796 814
Aspirin Dosage and Administration
Administration
Administer orally; may administer rectally as suppositories in patients who cannot tolerate oral therapy.a
Do not use aspirin preparation if strong vinegar-like odor is present.a
Oral Administration
Usually administer orally with food or a full glass of water (240 mL).a 836 906
Film-coated, extended-release, or enteric-coated may be associated with less GI irritation and/or symptomatic GI disturbances than uncoated tablets.a
Do not use delayed-release or extended-release tablets if rapid response is required.a
Swallow delayed-release and extended-release tablets whole; do not crush or chew.a
Prepare oral solution by dissolving 2 tablets for solution (Alka-Seltzer) in 120 mL of water; ingest the entire solution to ensure adequate dosing.838 843 844
Do not chew aspirin preparations for ≥7 days following tonsillectomy or oral surgery;841 837 do not place preparations directly on tooth or gum surface (possible tissue injury from prolonged contact).a
Rectal Administration
Do not administer aspirin tablets rectally.a
Dosage
When used for pain, fever, or inflammatory diseases, attempt to titrate to the lowest effective dosage.a
When used in anti-inflammatory dosages, development of tinnitus can be used as a sign of elevated plasma salicylate concentrations (except in patients with high-frequency hearing impairment).a
Pediatric Patients
Dosage in children should be guided by body weight or body surface area.a 841
Do not use in children and teenagers with varicella or influenza, unless directed by a clinician.841 (See Contraindications under Cautions.)
Pain
Oral
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).a
Dose may be given every 4 hours as necessary (up to 5 times in 24 hours).841
|
Age |
Weight |
Oral Dose |
|---|---|---|
|
<3 years of age |
<14.5 kg |
Consult clinician |
|
3–<4 years |
14.5–16 kg |
160 mg |
|
4–<6 years |
16–20.5 kg |
240 mg |
|
6–<9 years |
20.5–30 kg |
320 mg |
|
9–<11 years |
30–35 kg |
320–400 mg |
|
11 years |
35–38 kg |
320–480 mg |
For self-medication in children ≥12 years of age, 325–650 mg every 4 hours (maximum 4 g daily) or 1 g every 6 hours as necessary.836 940
For self-medication in children ≥12 years of age, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).837
For self-medication in children ≥12 years of age, 650 mg (as highly buffered effervescent solution [Alka-Seltzer Original]) every 4 hours (maximum 2.6 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 3.5 g daily).843 844
Rectal
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).a
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).a
Fever
Oral
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).a
Dose may be given every 4 hours as necessary (up to 5 times in 24 hours).841
|
Age |
Weight |
Oral Dose |
|---|---|---|
|
<3 years of age |
<14.5 kg |
Consult physician |
|
3–<4 years |
14.5–16 kg |
160 mg |
|
4–<6 years |
16–20.5 kg |
240 mg |
|
6–<9 years |
20.5–30 kg |
320 mg |
|
9–<11 years |
30–35 kg |
320–400 mg |
|
11 years |
35–38 kg |
320–480 mg |
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).a
For self-medication in children ≥12 years of age, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).837
Rectal
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).a
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).a
Inflammatory Diseases
Juvenile Rheumatoid Arthritis
OralInitially, 90–130 mg/kg daily in divided doses.906 938 Increase dosage as necessary for anti-inflammatory efficacy; target plasma salicylate concentration is 150–300 mcg/mL.906 938 Plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.906 938
Rheumatic Fever†
Oral
Initially, 90–130 mg/kg daily given in divided doses every 4–6 hours for up to 1–2 weeks for maximal suppression of acute inflammation, followed by 60–70 mg/kg daily in divided doses for 1–6 weeks.a Adjust dosage based on response, tolerance, and plasma salicylate concentrations.a Gradually withdraw over 1–2 weeks.a
Various regimens suggested depending on severity of initial manifestations.a Consult published protocols for more information on specific dosages and schedules.a
Thrombosis
Acute Arterial Ischemic Stroke†
OralACCP recommends 1–5 mg/kg daily initially until cerebral arterial dissection and cardioembolic causes have been excluded; subsequently, continue same dosage for ≥2 years.1013
In children with acute arterial ischemic stroke secondary to non-Moyamoya vasculopathy, at least 3 months of therapy recommended; ongoing antithrombotic therapy should be guided by repeat cerebrovascular imaging.1013
Fontan Procedure†
Oral1–5 mg/kg daily recommended by ACCP; optimal duration of therapy unknown.1013
Prosthetic Heart Valves (Mechanical or Biological)†
OralACCP recommends that clinicians follow same recommendations as in adults.1013
Kawasaki Disease
Oral
Initially, 80–100 mg/kg daily given in 4 equally divided doses (in combination with IGIV) for up to 14 days; initiate within 10 days of onset of fever.636 637 638 639 640 1013 When fever subsides, decrease dosage to 1–5 mg/kg once daily.636 637 638 950 1013
Continue indefinitely in those with coronary artery abnormalities;638 950 1013 in the absence of such abnormalities, continue low-dose aspirin for 6–8 weeks.638 950 1013
Adults
Pain
Oral
For self-medication, 325–650 mg every 4 hours (maximum 4 g daily) or 0.5–1 g every 6 hours as necessary.836 940
For self-medication, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).837
Adults <60 years of age for self-medication: 650 mg (as a highly buffered effervescent solution [Alka-Seltzer Lemon-Lime or Original]) every 4 hours (maximum 2.6 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 3.5 g daily).838 843 844
Adults ≥60 years of age for self-medication: 650 mg (as a highly buffered effervescent solution [Alka-Seltzer Lemon-Lime or Original]) every 4 hours (maximum 1.3 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 1.5 g daily).838 843 844
Rectal
325–650 mg every 4 hours as necessary (maximum 4 g daily).a
Pain Associated with Migraine Headache
OralFor self-medication, 500 mg (combined with acetaminophen 500 mg and caffeine 130 mg) as a single dose.701
Fever
Oral
325–650 mg every 4 hours as necessary (maximum 4 g daily).a
For self-medication, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).837
Rectal
325–650 mg every 4 hours as necessary (maximum 4 g daily).a
Inflammatory Diseases
Rheumatoid Arthritis and Arthritis and Pleurisy of SLE
OralInitially, 3 g daily in divided doses.906 938 943 Increase dosage as necessary for anti-inflammatory efficacy; target plasma salicylate concentration is 150–300 mcg/mL.906 938 943 Plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.906 938 943
Osteoarthritis
OralUp to 3 g daily in divided doses.906 938
Spondyloarthropathies
OralUp to 4 g daily in divided doses.906 938
Rheumatic Fever†
Oral
Initially, 4.9–7.8 g daily in divided doses given for maximal suppression of acute inflammation.a Adjust dosage based on response, tolerance, and plasma salicylate concentrations.a
Various regimens suggested depending on severity of initial manifestations.a Consult published protocols for more information on specific dosages and schedules.a
Transient Ischemic Attacks and Acute Ischemic Stroke
Secondary Prevention
Oral50–325 mg daily;a 646 906 990 some data suggest lower dosages (75–81 mg daily) may have similar benefits and possibly less bleeding risk.907
In patients with noncardioembolic ischemic stroke or TIA, 75–100 mg daily (or 25 mg twice daily, in combination with extended-release dipyridamole 200 mg twice daily) recommended; continue long term.738 1009
Acute Treatment†
OralACCP recommends 160–325 mg daily, initiated ideally within 48 hours of stroke onset; may decrease dosage after 1–2 weeks to reduce bleeding risk. 1009 (See Transient Ischemic Attacks and Acute Ischemic Stroke: Secondary Prevention, under Dosage.) ACCP states that initiation of aspirin therapy should be delayed for 24 hours following administration of recombinant tissue-type plasminogen activator (r-tPA, e.g., alteplase).1009
Coronary Artery Disease and Myocardial Infarction
STEMI
Oral162–325 mg as soon as acute STEMI is suspected, continued indefinitely at a dosage of 81–325 mg daily.527 579 646 906 938 Some experts prefer use of a maintenance dosage of 81 mg daily because of a decreased risk of bleeding and lack of definitive evidence demonstrating that higher dosages confer greater benefit.527
Use in conjunction with a P2Y12-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor).992 993 994 1010 If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages.955
Primary Prevention† of STEMI
OralSome experts recommend 75–162 mg once daily in carefully selected patients.1110 1116 1118 1119 (See Primary Prevention of Ischemic Cardiac Events under Uses.)
Established Coronary Artery Disease
Oral75–100 mg daily recommended by ACCP; continue indefinitely.1010 Some data suggest lower dosages (75–81 mg daily) may have similar benefits and possibly less bleeding risk.907
NSTE ACS
OralACC and AHA recommend an initial dose of 162–325 mg as soon as possible after presentation, unless contraindicated.1100 Continue with maintenance dosage of 81–325 mg daily.1100
Use in conjunction with a P2Y12-receptor antagonist (e.g., clopidogrel, ticagrelor).991 992 993 994 1010 If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages.955
Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting Surgery
OralPCI in patients already receiving aspirin: 81–325 mg initiated ≥2 hours, and preferably 24 hours, before the procedure in conjunction with a P2Y12-receptor antagonist.994
PCI in patients not already receiving long-term aspirin therapy: 325 mg daily (as non-enteric-coated formulation), initiated ≥2 hours, preferably 24 hours, prior to PCI in conjunction with a P2Y12-receptor antagonist.994
Maintenance therapy following PCI and stent placement (drug-eluting or bare-metal): 75–162 mg daily in combination with a P2Y12-receptor antagonist.992 994 1010 If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages.955 Administer P2Y12-receptor antagonist for ≥12 months; continue aspirin indefinitely.994
CABG: Some manufacturers recommend 325 mg daily, initiated 6 hours after surgery.906 938 AHA and ACCF recommend 100–325 mg daily, initiated within 6 hours after CABG and continued for up to 1 year.992 For long-term therapy after 1 year, ACCP recommends aspirin 75–100 mg daily.1010
Embolism Associated with Atrial Fibrillation†
Oral
75–325 mg daily suggested for prevention of thromboembolism.1007
Manage atrial flutter in the same manner as atrial fibrillation.999 1007
Mitral Valve Prolapse†
Oral
75–325 mg daily.996
Peripheral Arterial Disease
Oral
Primary prevention of cardiovascular events in patients with asymptomatic disease: 75–100 mg daily.1011
Secondary prevention of cardiovascular events in patients with symptomatic disease: 75–100 mg daily; continue long term.1011
Patients with refractory intermittent claudication: ACCP suggests the use of cilostazol in addition to aspirin therapy.1011
Peripheral Artery Bypass Graft Surgery
Oral
To reduce graft occlusion: 75–100 mg daily recommended by ACCP; initiate preoperatively and continue long term.1011
ACCP suggests addition of clopidogrel 75 mg daily to aspirin therapy in patients undergoing below-the-knee prosthetic graft bypass surgery.1011
Prosthetic Heart Valves
Mechanical Prosthetic Heart Valves†
OralAspirin 50–100 mg daily in addition to warfarin therapy recommended in all patients with a mechanical heart valve who have a low risk of bleeding.996 1008
Aspirin 75–325 mg once daily as monotherapy recommended as an alternative to warfarin in patients who are unable to take warfarin.996
Bioprosthetic Heart Valves†
OralPatients with bioprosthetic valves in the aortic position: 50–100 mg daily suggested by ACCP for initial (i.e., first 3 months after valve insertion) and long-term therapy.1008
Patients with bioprosthetic heart valves in the mitral position: 50–100 mg daily may be used for long-term antithrombotic therapy after initial 3-month treatment with warfarin.1008
Combination aspirin (75–100 mg daily) and warfarin therapy recommended by ACC/AHA for patients with bioprosthetic heart valves and additional risk factors for thromboembolism.996
Aspirin 75–325 mg once daily also recommended as an alternative to warfarin therapy in any patient who is unable to take warfarin.996
Complications of Pregnancy†
Oral
Antiphospholipid syndrome† and a history of multiple (≥ 3) pregnancy losses: Antepartum prophylaxis with aspirin (75–100 mg daily) in combination with sub-Q heparin or an LMWH recommended by ACCP.1012
Patients at risk for preeclampsia: ACCP recommends low-dose aspirin during pregnancy (starting from the second trimester).1012
Prescribing Limits
Pediatric Patients
Pain
Oral
Children 2–11 years of age: Maximum 2.5 g/m2 daily.a
Children ≥12 years of age: Maximum 4 g daily.836 Maximum 2.6 g as highly buffered effervescent solution (Alka-Seltzer Original) or 3.5 g (Alka-Seltzer Extra Strength) in 24 hours.843 844
For self-medication, do not exceed recommended daily dosage.841 Treatment duration for self-medication for pain: ≤ 5 days.841 (See Advice to Patients.) Treatment duration for self-medication of sore throat pain using chewing gum: ≤2 days.837
Rectal
Children 2–11 years of age: Maximum 2.5 g/m2 daily.a
Children ≥12 years of age: Maximum 4 g daily.a
Fever
Oral
Children 2–11 years of age: Maximum 2.5 g/m2 daily.a
Children ≥12 years of age: Maximum 4 g daily.836
For self-medication, do not exceed recommended daily dosage.841 Treatment duration for self-medication: <3 days.841 (See Advice to Patients.)
Rectal
Children 2–11 years of age: Maximum 2.5 g/m2 daily.a
Children ≥12 years of age: Maximum 4 g daily.a
Adults
Pain
Oral
Maximum 4 g daily.a Treatment duration for self-medication for pain: ≤10 days.841 Aspirin chewing gum should not be used for self-medication of sore throat pain for longer than 2 days.837 (See Advice to Patients.)
Adults <60 years of age taking highly buffered effervescent solutions: Maximum 2.6 g (Alka-SeltzerLemon-lime or Original) or 3.5 g (Alka-Seltzer Extra Strength) in 24 hours.838 843 844
Adults ≥60 years of age taking highly buffered effervescent solutions: Maximum 1.3 g (Alka-SeltzerLemon-lime or Original) or 1.5 g (Alka-Seltzer Extra Strength) in 24 hours.838 843 844
Rectal
Maximum 4 g daily.a
Pain Associated with Migraine Headache
OralFor self-medication, maximum 500 mg (in combination with acetaminophen 500 mg and caffeine 130 mg) in 24 hours.701
Fever
Oral or Rectal
Maximum 4 g daily.a
Special Populations
Geriatric Patients
Highly buffered effervescent solution: Maximum 1.3 g (Alka-SeltzerLemon-Lime or Original) or 1.5 g (Alka-Seltzer Extra Strength) in 24 hours.838 843 844
Cautions for Aspirin
Contraindications
-
Known hypersensitivity to aspirin or any ingredient in the formulation.906 938
-
History of asthma, urticaria, or other sensitivity reaction precipitated by other NSAIAs.906 938
-
Syndrome of asthma, rhinitis, and nasal polyps.938
-
Children or adolescents with viral infections (with or without fever) because of the possibility that the infection may be one associated with an increased risk of Reye’s syndrome.906 938 (See Pediatric Use under Cautions.)
Warnings/Precautions
Warnings
Alcohol
Long-term heavy alcohol use (≥3 alcoholic beverages daily) associated with an increased risk of aspirin-induced bleeding.906 938 941 (See Advice to Patients.)
Hematologic Effects
Inhibits platelet aggregation and may prolong bleeding time.906 938 These effects may be particularly important in patients with inherited (e.g., hemophilia) or acquired (e.g., liver disease, vitamin K deficiency) bleeding disorders.906 938
Because of the increased risk of bleeding, avoid aspirin-containing chewing gum tablets or gargles for ≥1 week after tonsillectomy or oral surgery.h
GI Effects
Serious GI toxicity (e.g., bleeding, ulceration, perforation) can occur with or without warning symptoms.938 Increased risk in those with a history of GI bleeding or ulceration, geriatric patients, and those receiving an anticoagulant or corticosteroid, receiving excessive dosages or prolonged therapy, taking multiple NSAIAs concomitantly, or consuming ≥3 alcohol-containing beverages daily.941 1035
Avoid in patients with active peptic ulcer disease; can cause gastric mucosal irritation and bleeding.906 938
Despite current warnings on OTC product labels, serious bleeding events continue to occur in patients receiving aspirin in fixed combination with antacids for self-medication.1035 FDA is evaluating whether additional actions are needed to address this safety concern.1035
Thrombosis Associated with Drug-eluting Stents
Stent thrombosis with potentially fatal sequelae, particularly with drug-eluting stents (DES),886 890 891 associated with premature discontinuance (<12 months) of dual-drug therapy with a thienopyridine derivative and aspirin.886 890 891 892 893 894 895 896 897 898 899 900 (See Percutaneous Coronary Intervention and Revascularization Procedures under Uses.)
At least 12 months of dual-drug antiplatelet therapy is recommended in patients with any type of coronary artery stent (bare-metal or drug-eluting).993 994 1010 Preliminary evidence from a randomized controlled study suggests that an even longer duration (up to 30 months) of dual-drug antiplatelet therapy may be beneficial in reducing stent thrombosis and other cardiovascular events in patients with a drug-eluting stent; however, such prolonged therapy was associated with increased bleeding and an unexpected finding of increased all-cause mortality.1019 1020 FDA is continuing to evaluate these findings and will communicate final conclusions and recommendations once the analysis is complete.1019
For non-elective procedures that mandate premature discontinuance of thienopyridine-derivative therapy, continue aspirin therapy if at all possible.886 Restart thienopyridine therapy as soon as possible after the procedure.886 (See Advice to Patients.)
Sensitivity Reactions
Anaphylactoid reactions, severe urticaria, angioedema, or bronchospasm reported.836 906 938 h Immediate medical intervention and discontinuance for anaphylaxis.836
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs.1202 Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).1202 Symptoms may resemble those of acute viral infection.1202 Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash.1202 If signs or symptoms of DRESS develop, discontinue the drug and immediately evaluate the patient.1202
Contraindicated in patients with syndrome of asthma, rhinitis, and nasal polyps;906 938 caution in patients with asthma.938
General Precautions
Sodium Content
Avoid highly buffered aspirin preparations in patients with CHF, renal failure, or other conditions in which high sodium content would be harmful.906 938
Individuals with Phenylketonuria
Some preparations contain aspartame (NutraSweet), which is metabolized in the GI tract to phenylalanine.a 838
Use of Fixed Combinations
When aspirin is used in fixed combination with other agents, consider the cautions, precautions, and contraindications associated with the other agent(s).a
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.1200 1202
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.1202
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice.1200 1202 However, FDA states that these recommendations do not apply to low-dose aspirin therapy; low (e.g., 81-mg) doses of aspirin may be used under the direction of a clinician at any time during pregnancy for the treatment of certain pregnancy-related conditions.1200 (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs.1200 1202 Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance.1200 1202 Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation.1200 1202 In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios.1200 1202 Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis).1200 1202 Deaths associated with neonatal renal failure also reported.1200 Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use.1202 Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.1202
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization.1202 In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.1202
Maternal and fetal hemorrhagic complications observed with maternal ingestion of large doses (e.g., 12–15 g daily) of aspirin594 595 597 611 612 generally have not been observed in studies in which low doses (60–150 mg daily) of the drug were used for prevention of complications of pregnancy†.594 595 596 597 598 599 600 601 605 626 627 629 630 631 632
Lactation
Distributed into milk; use not recommended.906 938 High doses may result in adverse effects (rash, platelet abnormalities, bleeding) in nursing infants.906 938
Pediatric Use
Dosing recommendations for juvenile rheumatoid arthritis based on well controlled clinical studies.906 938 High dosages that result in plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.906 938
Use in children with varicella infection or influenza-like illnesses reportedly is associated with an increased risk of developing Reye’s syndrome.166 167 168 169 468 538 549 638 US Surgeon General, AAP Committee on Infectious Diseases, FDA, and other authorities advise that salicylates not be used in children and teenagers with varicella or influenza, unless directed by a clinician.466 467 554 638 Generally avoid salicylates in children and teenagers with suspected varicella or influenza and during presumed outbreaks of influenza, since accurate diagnosis of these diseases may be impossible during the prodromal period;466 use of salicylates in the management of viral infections in children or adolescents is contraindicated, since the infection may be one associated with an increased risk of Reye’s syndrome.646 906
Use with caution in pediatric patients who are dehydrated (increased susceptibility to salicylate intoxication).h
Safety and efficacy of aspirin in fixed combination with extended-release dipyridamole not established.738
Risk of overdosage and toxicity (including death) in children <2 years of age receiving preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection.937 939 Limited evidence of efficacy for these preparations in this age group; appropriate dosages not established.937 Use such preparations in children <2 years of age with caution and only as directed by clinician.937 939 Clinicians should ask caregivers about use of OTC cough/cold preparations to avoid overdosage.937
Hepatic Impairment
Avoid in patients with severe hepatic impairment.906 938
Renal Impairment
Avoid in patients with GFR <10 mL/minute.906 938
Common Adverse Effects
Minor upper GI symptoms (dyspepsia).938
Drug Interactions
Protein-bound Drugs
Potential for salicylate to be displaced from binding sites by, or to displace from binding sites, other protein-bound drugs.906 h Aspirin acetylates serum albumin, which may alter binding of other drugs to the protein.a
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitors938 Possible attenuation of hemodynamic actions of ACE inhibitors in patients with CHFh |
Monitor BP938 |
|
Acidifying agents |
Drugs that decrease urine pH may decrease salicylate excretionh |
|
|
Alcohol |
||
|
Alkalinizing agents |
Drugs that increase urine pH may increase salicylate excretionh |
Monitor plasma salicylate concentrations in patients receiving high-dose aspirin therapy if antacids are initiated or discontinuedh |
|
Anticoagulants (warfarin, heparin) |
Increased risk of bleeding906 938 May displace warfarin from protein-binding sites, leading to prolongation of PT and bleeding time906 938 |
Use with cautionh |
|
Anticonvulsants |
May displace phenytoin from binding sites; possible decrease in total plasma phenytoin concentrations, with increased free fraction906 938 May displace valproic acid from binding sites; possible increase in free plasma valproic acid concentrations;906 938 h possible increased risk of bleedingh |
Monitor patients receiving aspirin with valproic acidh |
|
Antidiabetic drugs (sulfonylureas) |
Monitor closelyh |
|
|
β-adrenergic blocking agents |
Reduced BP response to β-adrenergic blocking agents 906 938 Potential for salt and fluid retention906 |
Monitor BP938 |
|
Carbonic anhydrase inhibitors (acetazolamide) |
Increased risk of salicylate toxicityh Increased plasma acetazolamide concentrations; increased risk of acetazolamide toxicity906 938 |
Avoid concomitant use in patients receiving high-dose aspirinh |
|
Corticosteroids |
Decreased plasma salicylate concentrationsh |
Monitor for adverse effects of either drugh |
|
Diuretics |
Possible reduced natriuretic effect938 |
|
|
Methotrexate |
Increased plasma methotrexate concentrationsh Inhibition of renal clearance of methotrexate leading to bone marrow toxicity, especially in geriatric patients or patients with renal impairment906 |
Monitor for methotrexate toxicityh |
|
NSAIAs |
Increased risk of bleeding, GI ulceration, decreased renal function, or other complications861 906 946 947 948 No consistent evidence that low-dose aspirin mitigates increased risk of serious cardiovascular events associated with NSAIAs861 948 Pharmacokinetic interactions with many NSAIAsh Antagonism (ibuprofen, naproxen) of the irreversible platelet-aggregation inhibitory effect of aspirin; may limit the cardioprotective effects of aspirin788 858 859 860 Minimal risk of attenuating effects of low-dose aspirin with occasional use of ibuprofen858 Not known whether ketoprofen interferes with the antiplatelet effect of aspirin858 859 Decreased peak plasma concentration and AUC of diclofenac;946 947 limited data indicate that diclofenac does not inhibit antiplatelet effect of aspirin788 |
Concomitant use not recommended906 938 946 947 948 Pharmacokinetic interactions unlikely to be clinically importanth Immediate-release aspirin: Administer a single dose of ibuprofen 400 mg for self-medication≥8 hours before or ≥30 minutes after administration of aspirin858 859 Enteric-coated low-dose aspirin: No recommendations regarding timing of administration with single dose of ibuprofen858 859 Consider use of alternative analgesics that do not interfere with antiplatelet effect of low-dose aspirin (e.g., acetaminophen, opiates) for patients at high risk of cardiovascular events858 859 Concomitant use with prescription NSAIAs not recommended because of potential for increased adverse effects861 |
|
Pyrazinamide |
Possible prevention or reduction of hyperuricemia associated with pyrazinamideh |
|
|
Tetracycline |
Decreased oral absorption of tetracyclines when administered with aspirin preparations containing divalent or trivalent cations (Bufferin)h |
Administer preparations containing divalent or trivalent cations (Bufferin) 1 hr before or after tetracyclineh |
|
Thrombolytic agents |
Additive reduction in mortality reported in patients with AMI receiving aspirin in low dosages and thrombolytic agents (streptokinase, alteplase)579 580 581 582 583 584 585 586 587 588 589 590 |
Used for therapeutic effect579 580 581 582 583 584 585 586 587 588 589 590 |
|
Uricosuric agents (probenecid, sulfinpyrazone) |
||
|
Varicella virus vaccine live |
Theoretical possibility of Reye’s syndrome638 |
Manufacturer of varicella virus vaccine live recommends that individuals who receive the vaccine avoid use of salicylates for 6 weeks following vaccination756 For children who are receiving long-term salicylate therapy, AAP suggests weighing theoretical risks of vaccination against known risks of wild-type virus;638 ACIP states that children who have rheumatoid arthritis or other conditions requiring therapeutic salicylate therapy probably should receive varicella virus vaccine live in conjunction with subsequent close monitoring757 |
Aspirin Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.906 h Rapidly metabolized to salicylic acid; plasma aspirin concentrations are undetectable 1–2 hours after administration.906 Peak plasma salicylic acid concentrations attained within 1–2 hours following administration of uncoated tablets.906
Slowly and variably absorbed following rectal administration.h
Onset
Single oral doses of rapidly absorbed preparations: 30 minutes for analgesic and antipyretic effects.h
Rectal suppositories: 1–2 hours for antipyretic effects.h
Continuous oral therapy: 1–4 days for anti-inflammatory effect.h
Food
Food decreases rate but not extent of absorption; peak plasma concentrations of aspirin and salicylate may be decreased.h
Plasma Concentrations
Plasma salicylate concentrations of 30–100 mcg/mL produce analgesia and antipyresis; the concentration required for anti-inflammatory effect is 150–300 mcg/mL; toxicity noted at 300–350 mcg/mL.h
Steady-state plasma salicylate concentrations increase more than proportionally with increasing doses as a result of capacity-limiting processes.h
Special Populations
During the febrile phase of Kawasaki disease, oral absorption may be impaired or highly variable.h
Distribution
Extent
Widely distributed; aspirin and salicylate distribute into synovial fluid.906 a h Crosses placenta and distributed into milk.906
Plasma Protein Binding
Aspirin: 33%.a
Salicylate: 90–95% bound at plasma salicylate concentrations <100 mcg/mL; 70–85% bound at concentrations of 100–400 mcg/mL; 25–60% bound at concentrations >400 mcg/mL.906 h
Elimination
Metabolism
Partially hydrolyzed to salicylate by esterases in the GI mucosa.a Unhydrolyzed aspirin subsequently undergoes hydrolysis by esterases mainly in the liver but also in plasma, erythrocytes, and synovial fluid.a
Salicylate is metabolized in the liver by the microsomal enzyme system.h
Elimination Route
Excreted in urine via glomerular filtration and renal tubular reabsorption as salicylate and its metabolites.h Urinary excretion of salicylate is pH dependent; as urine pH increases from 5 to 8, urinary excretion of salicylate is greatly increased.h
Half-life
Aspirin: 15–20 minutes.a
Half-life of salicylate increases with increasing plasma salicylate concentrations.906 h
Salicylate: 2–3 hours when aspirin administered in low doses (325 mg).h
Salicylate: 15–30 hours when aspirin administered in higher dosages.h
Special Populations
Salicylate and its metabolites readily removed by hemodialysis and, to a lesser extent, by peritoneal dialysis.h
Stability
Storage
Oral
Capsules
Aspirin in fixed-combination with extended-release dipyridamole: 25°C (may be exposed to 15–30°C).738 Protect from excessive moisture.738
Gum
15–25°C; protect from excessive moisture.837
Tablets
Room temperature (Bayer products, excluding Alka-Seltzer products);839 840 841 842 906 avoid high humidity and excessive heat (40°C).840
15–30°C (Easprin).943
20–25°C (Anacin Extra Strength); protect from moisture.836
Protect from excessive heat (Alka-Seltzer products).838 843 844
Rectal
Suppositories
2–15°C.a
Actions
-
Inhibits COX-1 and COX-2 activity.1016
-
Pharmacologic actions similar to those of prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.938
-
Irreversibly acetylates and inactivates COX-1 in platelets.1016
-
The existence of 2 COX isoenzymes with different aspirin sensitivities and extremely different recovery rates of their COX activity following inactivation by aspirin at least partially explains the different dosage requirements and durations of aspirin effects on platelet function versus the drug’s analgesic and anti-inflammatory effects.1016
-
Effects on urinary excretion of uric acid are dose related; large dosages (e.g., 1.3 g 4 times daily) enhance urinary excretion and decrease serum concentrations of uric acid , intermediate dosages (e.g., 650 mg to 1 g 3 times daily) usually do not alter uric acid excretion, and low dosages (e.g., <325 mg 3 times daily) inhibit excretion and may increase serum uric acid concentrations.h
Advice to Patients
-
When used for self-medication, importance of reading the product labeling.836 841 837 838 843 844 940
-
When used for self-medication, importance of asking clinician whether to use aspirin or another analgesic if alcohol consumption is ≥3 alcohol-containing drinks per day.836 837 838 841 843 844 940
-
Importance of informing patients about risk of bleeding associated with chronic, heavy alcohol use while taking aspirin.906 941
-
When used for self-medication in children, importance of basing the dose on the child’s weight or body surface area.841
-
In patients with drug-eluting stents (DES) receiving aspirin in combination with clopidogrel or ticlopidine, importance of not discontinuing antiplatelet therapy without consulting cardiologist, even if instructed to do so by other health-care professional (e.g., dentist).886
-
Importance of not using aspirin for chicken pox or flu symptoms in children or adolescents without consulting a clinician.836 837 838 841 843 844 940
-
Patients receiving anticoagulants and those with asthma, gout, diabetes, arthritis, peptic ulcers, bleeding problems, or stomach problems that persist or recur should consult a clinician before using aspirin for self-medication.836 837 838 841 843 844 940
-
Discontinue and consult clinician if pain or fever persists or progresses, new symptoms occur, redness or swelling is present in a painful area, or ringing in the ears or loss of hearing occurs.836 837 838 841 843 844 940
-
Risk of GI bleeding or ulceration, particularly with prolonged therapy,906 938 941 and concomitant therapy with another NSAIA.941
-
Risk of anaphylactoid and other sensitivity reactions.938
-
Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding or rash develop.938
-
Importance of seeking immediate medical attention if an anaphylactic reaction occurs.938
-
Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed.938
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.1200 1202
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.938
-
Importance of informing patients of other important precautionary information.938 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Pieces, chewing gum |
227 mg |
Aspergum |
Heritage |
|
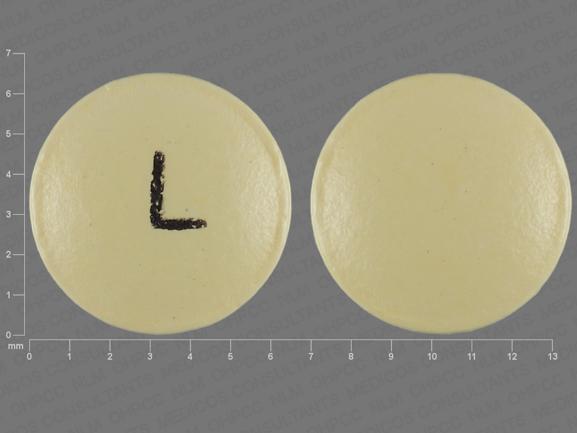
Tablets |
81 mg* |
Aspirin Tablets |
||
|
325 mg* |
Aspirin Tablets |
|||
|
Norwich Aspirin |
Chattem |
|||
|
500 mg* |
Aspirin Tablets |
|||
|
Norwich Aspirin Maximum Strength |
Chattem |
|||
|
650 mg* |
Aspirin Tablets |
|||
|
Tablets, chewable |
81 mg* |
Aspirin Chewable Tablets |
||
|
Bayer Aspirin Children’s |
Bayer |
|||
|
St. Joseph Aspirin Low Strength Adult Chewable |
McNeil |
|||
|
Tablets, delayed-release (enteric-coated) |
81 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
||
|
Bayer Aspirin Regimen Adult Low Strength |
Bayer |
|||
|
Ecotrin Adult Low Strength |
GlaxoSmithKline |
|||
|
Halfprin |
Kramer |
|||
|
St. Joseph Pain Reliever Adult |
McNeil |
|||
|
162 mg |
Halfprin |
Kramer |
||
|
325 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Bayer Aspirin Regimen Regular Strength Caplets |
Bayer |
|||
|
Ecotrin Regular Strength |
GlaxoSmithKline |
|||
|
Genacote |
Ivax |
|||
|
500 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Ecotrin Maximum Strength |
GlaxoSmithKline |
|||
|
650 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
975 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Easprin |
Rosedale |
|||
|
Tablets, extended-release |
800 mg |
ZORprin |
Par |
|
|
Tablets, film-coated |
325 mg* |
Aspirin Tablets |
||
|
Genuine Bayer Aspirin Tablets |
Bayer |
|||
|
500 mg |
Bayer Extra Strength Aspirin Caplets |
Bayer |
||
|
Rectal |
Suppositories |
60 mg* |
Aspirin Suppositories |
|
|
120 mg* |
Aspirin Suppositories |
|||
|
200 mg* |
Aspirin Suppositories |
|||
|
300 mg* |
Aspirin Suppositories |
|||
|
600 mg* |
Aspirin Suppositories |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, enteric-coated |
325 mg with buffers |
Ascriptin Enteric Regular Strength |
Novartis |
|
Tablets, film-coated |
81 mg with buffers |
Women’s Bayer Aspirin Plus Calcium Caplets |
Bayer |
|
|
325 mg with buffers |
Ascriptin Arthritis Pain Caplets |
Novartis |
||
|
Ascriptin Regular Strength |
Novartis |
|||
|
Bufferin Tablets |
Novartis |
|||
|
500 mg with buffers |
Ascriptin Maximum Strength Caplets |
Novartis |
||
|
Bayer Plus Extra Strength Caplets |
Bayer |
|||
|
Bufferin Extra Strength Caplets |
Novartis |
|||
|
Bufferin Extra Strength |
Novartis |
|||
|
Tablets, for solution |
325 mg |
Alka-Seltzer Effervescent Pain Reliever and Antacid |
Bayer |
|
|
Alka-Seltzer Lemon Lime Effervescent Pain Reliever and Antacid |
Bayer |
|||
|
500 mg |
Alka-Seltzer Extra Strength Effervescent Pain Reliever and Antacid |
Bayer |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For solution |
325 mg/packet Acetaminophen and Aspirin 500 mg/packet |
Goody’s Back & Body Pain Powder |
Prestige |
|
Tablets, film-coated |
250 mg Acetaminophen, Aspirin 250 mg, and buffer |
Excedrin Back and Body Caplets |
Novartis |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, gel-coated |
250 mg Acetaminophen, Aspirin 250 mg, and Caffeine 65 mg* |
Acetaminophen, Aspirin, and Caffeine Gelcaps |
|
|
Excedrin Menstrual Complete Gelcaps |
Novartis |
|||
|
For solution |
260 mg/packet Acetaminophen, Aspirin 520 mg/packet, and Caffeine 32.5 mg/packet |
Goody’s Extra Strength Headache Powder |
Prestige |
|
|
325 mg/packet Acetaminophen, Aspirin 500 mg/packet, and Caffeine 65 mg/packet |
Goody’s Cool Orange Extra Strength Powder |
Prestige |
||
|
Tablets, film-coated |
194 mg Acetaminophen, Aspirin 227 mg, Caffeine 33 mg, and buffers |
Vanquish Caplets |
Moberg |
|
|
250 mg Acetaminophen, Aspirin 250 mg, and Caffeine 65 mg |
Excedrin Extra Strength Caplets |
Novartis |
||
|
Excedrin Migraine Caplets |
Novartis |
|||
|
Goody's Extra Strength Caplets |
Prestige |
|||
|
Pamprin Max |
Chattem |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
4.8355 mg Oxycodone Hydrochloride and Aspirin 325 mg* |
Endodan ( C-II ) |
Qualitest |
|
Oxycodone Hydrochloride and Aspirin Tablets ( C-II ) |
||||
|
Percodan ( C-II; scored) |
Endo |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
325 mg with Butalbital 50 mg and Caffeine 40 mg* |
Butalbital, Aspirin, and Caffeine Capsules ( C-III ) |
|
|
Fiorinal ( C-III ) |
Actavis |
|||
|
325 mg with Butalbital 50 mg, Caffeine 40 mg, and Codeine Phosphate 30 mg* |
Butalbital, Aspirin, Caffeine, and Codeine Phosphate Capsules ( C-III ) |
|||
|
Fiorinal with Codeine ( C-III ) |
Actavis |
|||
|
356.4 mg with Caffeine 30 mg and Dihydrocodeine Bitartrate 16 mg |
Synalgos-DC ( C-III ) |
Leitner |
||
|
Capsules, extended-release core (dipyridamole only) |
25 mg with Dipyridamole 200 mg |
Aggrenox |
Boehringer Ingelheim |
|
|
For solution |
845 mg/packet with Caffeine 65 mg/packet |
BC Powder |
Prestige |
|
|
Stanback Powder |
Prestige |
|||
|
1000 mg/packet with Caffeine 65 mg/packet |
BC Powder Arthritis Strength |
Prestige |
||
|
Tablets |
325 mg with Butalbital 50 mg and Caffeine 40 mg* |
Butalbital, Aspirin, and Caffeine Tablets ( C-III ) |
||
|
Fortabs ( C-III ) |
United Research |
|||
|
325 mg with Carisoprodol 200 mg* |
Carisoprodol and Aspirin Tablets ( C-IV ) |
|||
|
Soma Compound ( C-IV ) |
Meda |
|||
|
325 mg with Carisoprodol 200 mg and Codeine Phosphate 16 mg* |
Carisoprodol, Aspirin, and Codeine Phosphate Tablets ( C-III ) |
|||
|
Soma Compound with Codeine ( C-III ) |
Meda |
|||
|
325 mg with Meprobamate 200 mg |
Equagesic ( C-IV; scored) |
Leitner |
||
|
Micrainin ( C-IV ) |
Wallace |
|||
|
385 mg with Caffeine 30 mg and Orphenadrine Citrate 25 mg* |
Norgesic |
3M |
||
|
Orphenadrine Citrate, Aspirin, and Caffeine Tablets |
Sandoz |
|||
|
400 mg with Caffeine 32 mg |
P-A-C Analgesic |
Lee |
||
|
770 mg with Caffeine 60 mg, and Orphenadrine Citrate 50 mg* |
Norgesic Forte (scored) |
3M |
||
|
Orphenadrine Citrate, Aspirin, and Caffeine Tablets |
Sandoz |
|||
|
Tablets, film-coated |
400 mg with Caffeine 32 mg |
Anacin Caplets |
Wyeth |
|
|
Anacin Tablets |
Wyeth |
|||
|
421 mg with Caffeine 32 mg and buffers |
Cope |
Lee |
||
|
500 mg with Caffeine 32 mg |
Anacin Maximum Strength |
Wyeth |
||
|
500 mg with Caffeine 32.5 mg |
Extra Strength Bayer Back and Body Pain (with propylene glycol) |
Bayer |
||
|
Tablets, for solution |
500 mg with Caffeine 65 mg |
Alka Seltzer Morning Relief |
Bayer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
166. Centers for Disease Control. Reye syndrome—Ohio, Michigan. MMWR Morb Mortal Wkly Rep. 1980; 29:532-9.
167. Starko KM, Ray CG, Dominguez LB et al. Reye’s syndrome and salicylate use. Pediatrics. 1980; 66:859-64. https://pubmed.ncbi.nlm.nih.gov/7454476
168. Partin JS, Schubert WK, Partin JC et al. Serum salicylate concentrations in Reye’s disease: a study of 130 biopsy-proven cases. Lancet. 1982; 1:191-4. https://pubmed.ncbi.nlm.nih.gov/6119559
169. Centers for Disease Control. National surveillance for Reye syndrome, 1981—update, Reye syndrome and salicylate usage. MMWR Morb Mortal Wkly Rep. 1982; 31:53-61. https://pubmed.ncbi.nlm.nih.gov/6799770
466. Committee on Infectious Diseases, American Academy of Pediatrics. Aspirin and Reye syndrome. Pediatrics. 1982; 69:810-2. https://pubmed.ncbi.nlm.nih.gov/7079050
467. Centers for Disease Control. Surgeon General’s advisory on the use of salicylates and Reye syndrome. MMWR Morb Mortal Wkly Rep. 1982; 31:289-90. https://pubmed.ncbi.nlm.nih.gov/6810083
468. Waldman RJ, Hall WN, McGee H et al. Aspirin as a risk factor in Reye’s syndrome. JAMA. 1982; 247:3089-04. https://pubmed.ncbi.nlm.nih.gov/7077803
469. Andresen BD, Alexander MS, Ng KJ et al. Aspirin and Reye’s disease: a reinterpretation. Lancet. 1982; 1:903. https://pubmed.ncbi.nlm.nih.gov/6122113
470. Wilson JT, Brown RD. Reye syndrome and aspirin use: the role of prodromal illness severity in the assessment of relative risk. Pediatrics. 1982; 69:822-5. https://pubmed.ncbi.nlm.nih.gov/7079054
527. O'Gara PT, Kushner FG, Ascheim DD et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e362-425.
529. Daniels SR, Greenberg RS, Ibrahim MA. Scientific uncertainties in the studies of salicylate use and Reye’s syndrome. JAMA. 1983; 249:1311-6. https://pubmed.ncbi.nlm.nih.gov/6827709
537. Remington PL, Rowley D, McGee H et al. Decreasing trends in Reye syndrome and aspirin use in Michigan, 1979 to 1984. Pediatrics. 1986; 77:93-8. https://pubmed.ncbi.nlm.nih.gov/3940363
538. Hurwitz ES, Barrett MJ, Bregman D et al. Public Health Service study on Reye’s syndrome and medications: report of the pilot phase. N Engl J Med. 1985; 313:849-57. https://pubmed.ncbi.nlm.nih.gov/4033715
539. Food and Drug Administration. Labeling for oral and rectal over-the-counter aspirin and aspirin-containing drug products. [21 CFR Part 201] Fed Regist. 1986; 51:8180-2. (IDIS 211617)
549. Hurwitz ES, Barrett MJ, Bregman D et al. Public Health Service study of Reye’s syndrome and medications: report of the main study. JAMA. 1987; 257:1905-11. https://pubmed.ncbi.nlm.nih.gov/3820509
550. Orlowski JP, Gillis J, Kilham HA. A catch in the Reye. Pediatrics. 1987; 80:638-42. https://pubmed.ncbi.nlm.nih.gov/3670965
551. Barrett MJ, Hurwitz ES, Schonberger LB et al. Changing epidemiology of Reye syndrome in the United States. Pediatrics. 1986; 77:598-602. https://pubmed.ncbi.nlm.nih.gov/3960627
552. Arrowsmith JB, Kennedy DL, Kuritsky JN et al. National patterns of aspirin use and Reye syndrome reporting, United States, 1980 to 1985. Pediatrics. 1987; 79:858-63. https://pubmed.ncbi.nlm.nih.gov/3588140
553. Centers for Disease Control. Reye syndrome surveillance—United States, 1986. MMWR Morb Mortal Wkly Rep. 1987; 36:687-91.
554. Glen-Bott AM. Aspirin and Reye’s syndrome: a reappraisal. Med Toxicol Adverse Drug Exp. 1987; 2:161-5.
555. Sweeney KR, Chapron DJ, Brandt JL et al. Toxic interaction between acetazolamide and salicylate: case reports and a pharmacokinetic explanation. Clin Pharmacol Ther. 1986; 40:518-24. https://pubmed.ncbi.nlm.nih.gov/3769383
556. Fitzgerald GA. Dipyridamole. N Engl J Med. 1987; 316:1247-57. https://pubmed.ncbi.nlm.nih.gov/3553945
557. Stein PD, Collins JJ, Kantrowitz A. American College of Chest Physicians and the National Heart, Lung, and Blood Institute National Conference on Antithrombotic Therapy. Antithrombotic therapy in mechanical and biological prosthetic heart valves and saphenous vein bypass grafts. Chest. 1986; 89(Suppl):46-53S.
558. Hirsch J, Fuster V, Salzman E. American College of Chest Physicians and the National Heart, Lung, and Blood Institute National Conference on Antithrombotic Therapy. Dose antiplatelet agents: the relationship among side effects, and antithrombotic effectiveness. Chest. 1986; 89(Suppl):4-10S. https://pubmed.ncbi.nlm.nih.gov/3510108
559. Chesebro JH, Steele PM, Fuster V. Platelet-inhibitor therapy in cardiovascular disease: effective defense against thromboembolism. Postgrad Med. 1985; 78:48-50,57-71. https://pubmed.ncbi.nlm.nih.gov/3160013
560. Chesebro JE, Clements IP, Fuster V et al. A platelet-inhibitor drug trial in coronary-artery bypass operations. N Engl J Med. 1982; 307:73-8. https://pubmed.ncbi.nlm.nih.gov/7045659
561. Chesebro JH, Fuster V, Elverback LR et al. Effect of dipyridamole and aspirin on late vein-graft patency after coronary bypass operations. N Engl J Med. 1984; 310:209-14. https://pubmed.ncbi.nlm.nih.gov/6361561
562. Chesebro JH, Fuster V, Elverback LR. Dipyridamole and aspirin and patency of coronary bypass grafts. N Engl J Med. 1984; 310:1534. https://pubmed.ncbi.nlm.nih.gov/6538932
563. Brown BG, Cukingnan RA, DeRouen T et al. Improved graft patency in patients treated with platelet-inhibiting therapy after coronary bypass surgery. Circulation. 1985; 72:138-46. https://pubmed.ncbi.nlm.nih.gov/3874009
564. The American-Canadian Co-operative Study Group. Persantine aspirin trial in cerebral ischemia. Part II: endpoint results. Stroke. 1985; 16:406-15. https://pubmed.ncbi.nlm.nih.gov/2860740
565. The ESPS Study Group. The European stroke prevention study (ESPS): principal end-points. Lancet. 1987; 2:1351-4. https://pubmed.ncbi.nlm.nih.gov/2890951
566. Grotta JC. Current medical and surgical therapy for cerebrovascular disease. N Engl J Med. 1987; 317:1505-16. https://pubmed.ncbi.nlm.nih.gov/3317048
567. Fields WS. Dipyridamole. N Engl J Med. 1987; 317:1735.
568. Goldberg TH. Dipyridamole. N Engl J Med. 1987; 317:1735.
569. Genton E, Clagett GP, Salzman EW. American College of Chest Physicians and the National Heart, Lung, and Blood Institute National Conference on Antithrombotic Therapy. Antithrombotic therapy in peripheral vascular disease. Chest. 1986; 89(Suppl):75-81S. https://pubmed.ncbi.nlm.nih.gov/3940794
570. Sherman DG, Dyken ML, Fisher M et al. American College of Chest Physicians and the National Heart, Lung, and Blood Institute National Conference on Antithrombotic Therapy. Cerebral embolism. Chest. 1986; 89(Suppl):82-98S.
571. Anon. Doubts about dipyridamole as an antithrombotic drug. Drug Ther Bull. 1984; 22:25-8. https://pubmed.ncbi.nlm.nih.gov/6368165
572. Rivey MP, Alexander MR, Taylor JW. Dipyridamole: a critical evaluation. Drug Intell Clin Pharm. 1984; 18:869-80. https://pubmed.ncbi.nlm.nih.gov/6389068
573. The Steering Committee of the Physicians’ Health Study Research Group. Preliminary report: findings from the aspirin component of the ongoing physicians’ health study. N Engl J Med. 1988; 318:262-4. https://pubmed.ncbi.nlm.nih.gov/3275899
574. Relman AS. Aspirin for the primary prevention of myocardial infarction. N Engl J Med. 1988; 318:245-6. https://pubmed.ncbi.nlm.nih.gov/3275897
575. Peto R, Gray R, Collins R et al. Randomised trial of prophylactic daily aspirin in British male doctors. BMJ. 1988; 296:313-6. https://pubmed.ncbi.nlm.nih.gov/3125882
576. Orme M. Aspirin all round. BMJ. 1988; 296:307-8. https://pubmed.ncbi.nlm.nih.gov/3125876
577. UK-TIA Study Group. United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: interim results. BMJ. 1988; 296:316-20. https://pubmed.ncbi.nlm.nih.gov/2894232
578. Anon. Labeling for oral and rectal over-the-counter aspirin and aspirin-containing drug products: Reye syndrome warning. Fed Regist. 1988; 53:21633-7.
579. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of IV streptokinase, oral aspirin, both, or neither among 17 187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988; 2:349-60. https://pubmed.ncbi.nlm.nih.gov/2899772
580. Genentech, Inc. Activase (alteplase, recombinant: a tissue plasminogen activator) prescribing information. South San Francisco, CA; 1988 Jun.
581. Topol EJ, Califf RM, George BS et al. A randomized trial of immediate versus delayed elective angioplasty after IV tissue plasminogen activator in acute myocardial infarction. N Engl J Med. 1987; 317:581-8. https://pubmed.ncbi.nlm.nih.gov/2956516
582. Guerci AD, Gerstenblith G, Brinker JA et al. A randomized trial of IV tissue plasminogen activator for acute myocardial infarction with subsequent randomization to elective coronary angioplasty. N Engl J Med. 1987; 317:1613-8. https://pubmed.ncbi.nlm.nih.gov/2960897
583. Williams DO, Borer J, Braunwald E et al. IV recombinant tissue-type plasminogen activator in patients with acute myocardial infarction: a report from the NHLBI thrombolysis in myocardial infarction trial. Circulation. 1986; 73:338-46. https://pubmed.ncbi.nlm.nih.gov/3080261
584. Chesebro JH, Knatterud G, Roberts R et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between IV tissue plasminogen activator and IV streptokinase. Clinical findings through hospital discharge. Circulation. 1987; 76:142-54. https://pubmed.ncbi.nlm.nih.gov/3109764
585. Mueller HS, Rao AK, Forman SA et al. Thrombolysis in Myocardial Infarction (TIMI): comparative studies of coronary reperfusion and systemic fibrinogenolysis with two forms of recombinant tissue-type plasminogen activator. J Am Coll Cardiol. 1987; 10:479-90. https://pubmed.ncbi.nlm.nih.gov/3114349
586. Mueller HS. Thrombolysis in Myocardial Infarction (TIMI): update 1987. Klin Wochenschr. 1988; 66(Suppl XII):93- 101. https://pubmed.ncbi.nlm.nih.gov/3126350
587. Kabivitrum, Inc. Kabikinase (streptokinase) prescribing information. Alameda, CA; 1987 Nov.
588. Hoechst-Roussel Pharmaceuticals Inc. Streptase (streptokinase) prescribing information. Somerville, NJ; 1987 Nov.
589. Van de Werf F, Arnold AER. IV tissue plasminogen activator and size of infarct, left ventricular function, and survival in acute myocardial infarction. BMJ. 1988; 297:1374-9. https://pubmed.ncbi.nlm.nih.gov/3146370
590. Van de Werf F, European Cooperative Study Group for Recombinant Tissue-Type Plasminogen Activator. Lessons from the European Cooperative recombinant tissue-type plasminogen activator (rt-PA) versus placebo trial. J Am Coll Cardiol. 1988; 12:14A-9. https://pubmed.ncbi.nlm.nih.gov/3142943
591. Marder VJ, Sherry S. Thrombolytic therapy: current status (first of two parts). N Engl J Med. 1988; 318:1512-20. https://pubmed.ncbi.nlm.nih.gov/3285216
592. Loscalzo J, Braunwald E. Tissue plasminogen activator. N Engl J Med. 1988; 319:925-31. https://pubmed.ncbi.nlm.nih.gov/3138537
593. Sobel BE. Pharmacologic thrombolysis: tissue-type plasminogen activator. Circulation. 1987; 76(Suppl II):II-39- 43.
594. Lubbe WF. Prevention of preeclampsia by low dose aspirin. N Z Med J. 1990; 103:237-8. https://pubmed.ncbi.nlm.nih.gov/2188173
595. Schiff E, Mashiach S. Aspirin to prevent pregnancy-induced hypertension. N Engl J Med. 1990; 322:204-5. https://pubmed.ncbi.nlm.nih.gov/2294442
596. Walsh SW. Low-dose aspirin: treatment for the imbalance of increased thromboxane and decreased prostacyclin in preeclampsia. Am J Perinatol. 1989; 6:124-32. https://pubmed.ncbi.nlm.nih.gov/2653334
597. Lubbe WF. Low-dose aspirin in prevention of toxaemia of pregnancy: does it have a place? Drugs. 1987; 34:515-8.
598. Trudinger BJ, Cook CM, Thompson RS et al. Low dose aspirin therapy improves fetal weight in umbilical placental insufficiency. Am J Obstet Gynecol. 1988; 159:681-5. https://pubmed.ncbi.nlm.nih.gov/3048102
599. Benigni A, Gregorini G, Frusca T et al. Effect of low-dose aspirin on fetal and maternal generation of thromboxane by platelets in women at risk for pregnancy-induced hypertension. N Engl J Med. 1989; 321:357-62. https://pubmed.ncbi.nlm.nih.gov/2664523
600. Elder MG, de Swiet M, Robertson A et al. Low-dose aspirin in pregnancy. Lancet. 1988; 1:410. https://pubmed.ncbi.nlm.nih.gov/2893204
601. Schiff E, Peleg E, Goldenberg M et al. The use of aspirin to prevent pregnancy-induced hypertension and lower the ratio of thromboxane A2 to prostacyclin in relatively high risk pregnancies. N Engl J Med. 1989; 321:351-6. https://pubmed.ncbi.nlm.nih.gov/2664522
602. Schiff E, Barkai G, Ben-Baruch G et al. Low-dose aspirin does not influence the clinical course of women with mild pregnancy-induced hypertension. Obstet Gynecol. 1990; 76:742-4. https://pubmed.ncbi.nlm.nih.gov/2216216
603. Wallenburg HCS, Dekker GA, Makovitz JW et al. Low-dose aspirin prevents pregnancy-induced hypertension and pre-eclampsia in angiotensin-sensitive primigravidae. Lancet. 1986; 1:1-3. https://pubmed.ncbi.nlm.nih.gov/2867260
604. Cunningham FG, Gant NF. Prevention of preeclampsia—a reality? N Engl J Med. 1989; 321:606-7. Editorial.
605. Trudinger BJ, Cook CM, Thompson R et al. Low-dose aspirin improves fetal weight in umbilical placental insufficiency. Lancet. 1988; 2:214-5. https://pubmed.ncbi.nlm.nih.gov/2899680
606. Ylikorkala O, Mäkilä UM, Kääpä P et al. Maternal ingestion of acetylsalicylic acid inhibits fetal and neonatal prostacyclin and thromboxane in humans. Am J Obstet Gynecol. 1986; 155:345-9. https://pubmed.ncbi.nlm.nih.gov/3526896
607. Walsh SW. Thromboxane production in placentas of women with preeclampsia. Am J Obstet Gynecol. 1989; 160:1535-6. https://pubmed.ncbi.nlm.nih.gov/2735372
608. Anon. Acetylsalicylic acid and eclampsia. WHO Drug Information. 1990; 4(1):11-2.
609. Fitzgerald D, Fitzgerald G. Thromboxane production in placentas of women with preeclampsia. Am J Obstet Gynecol. 1989; 160:1536. https://pubmed.ncbi.nlm.nih.gov/2525339
610. Anon. Aspirin and pre-eclampsia. Lancet. 1986; 1:18-20. https://pubmed.ncbi.nlm.nih.gov/2867264
611. Collins E, Turner G. Maternal effects of regular salicylate ingestion in pregnancy. Lancet. 1975; 2:335-8. https://pubmed.ncbi.nlm.nih.gov/51142
612. Stuart MJ, Gross SJ, Elrad H et al. Effects of acetylsalicylic-acid ingestion on maternal and neonatal hemostasis. N Engl J Med. 1982; 307:909-12. https://pubmed.ncbi.nlm.nih.gov/7110272
613. Lewis HD Jr, Davis JW, Archibald DG et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1983; 309:396-403. https://pubmed.ncbi.nlm.nih.gov/6135989
614. Theroux P, Ouimet H, McCans J et al. Aspirin, heparin, or both to treat acute unstable angina. N Engl J Med. 1988; 319:1105-11. https://pubmed.ncbi.nlm.nih.gov/3050522
615. Yusuf S, Wittes J, Friedman L. Overview of results of randomized clinical trials in heart disease. II. Unstable angina, heart failure, primary prevention with aspirin, and risk factor modification. JAMA. 1988; 260:2259-63. https://pubmed.ncbi.nlm.nih.gov/3050165
616. Lewis HD Jr. Which role for antiplatelet and anticoagulant drugs in unstable angina pectoris? Cardiovasc Drugs Ther. 1988; 2:103-6.
617. The RISC Group. Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. Lancet. 1990; 336:827-30. https://pubmed.ncbi.nlm.nih.gov/1976875
618. Spinler SA, Davis LE. Advances in the treatment of unstable angina pectoris. Clin Pharm. 1991; 10:825-38. https://pubmed.ncbi.nlm.nih.gov/1794219
619. Kar S, Wakida Y, Nordlander R. The high-risk unstable angina patient. An approach to treatment. Drugs. 1992; 43:837-48. https://pubmed.ncbi.nlm.nih.gov/1379156
620. Waters D, Lam J, Theroux P. Newer concepts in the treatment of unstable angina pectoris. Am J Cardiol. 1991; 68:34C-41C. https://pubmed.ncbi.nlm.nih.gov/1951101
621. Theroux P. Antiplatelet and antithrombotic therapy in unstable angina. Am J Cardiol. 1991; 68:92-8B.
622. Hyers TM. Heparin therapy. Regimens and treatment considerations. Drugs. 1992; 44:738-49. https://pubmed.ncbi.nlm.nih.gov/1280566
623. Schreiber TL, Rizik D, White C et al. Randomized trial of thrombolysis versus heparin in unstable angina. Circulation. 1992; 86:1407-14. https://pubmed.ncbi.nlm.nih.gov/1423953
624. Qui S, Theroux P, McCans J et al. Heparin prevents myocardial infarction better than aspirin in the acute phase of unstable angina. Circulation. 1991; 84(Suppl II):II-345.
625. Theroux P, Waters D, Lam J et al. Reactivation of unstable angina after the discontinuation of heparin. N Engl J Med. 1992; 327:141-5. https://pubmed.ncbi.nlm.nih.gov/1608405
626. Cowchock FS, Reece EA, Balaban D et al. Repeated fetal losses associated with antiphospholipid antibodies: a collaborative randomized trial comparing prednisone with low-dose heparin treatment. Am J Obstet Gynecol. 1992; 166:1318-23. https://pubmed.ncbi.nlm.nih.gov/1595785
627. Kutteh WH. Antiphospholipid antibody–associated recurrent pregnancy loss: treatment with heparin and low-dose aspirin is superior to low-dose aspirin alone. Am J Obstet Gynecol. 1996; 174:1584-9. https://pubmed.ncbi.nlm.nih.gov/9065133
628. Rai R, Cohen H, Dave M et al. Randomised controlled trial of aspirin and aspirin plus heparin in pregnant women with recurrent miscarriage associated with phospholipid antibodies (or antiphospholipid antibodies). BMJ. 1997; 314:253-7. https://pubmed.ncbi.nlm.nih.gov/9022487
629. Silver RK, MacGregor SN, Sholl JS et al. Comparative trial of prednisone plus aspirin versus aspirin alone in the treatment of anticardiolipin antibody-positive obstetric patients. Am J Obstet Gynecol. 1993; 169:1411-7. https://pubmed.ncbi.nlm.nih.gov/8267038
630. Silveira LH, Hubble CL, Jara LJ et al. Prevention of anticardiolipin antibody-related pregnancy losses with prednisone and aspirin. Am J Med. 1992; 93:403-10. https://pubmed.ncbi.nlm.nih.gov/1415304
631. Kwak JYH, Gilman-Sachs A, Beaman KD et al. Reproductive outcome in women with recurrent spontaneous abortions of alloimmune and autoimmune causes: preconception versus postconception treatment. Am J Obstet Gynecol. 1992; 166:1787-98. https://pubmed.ncbi.nlm.nih.gov/1615988
632. Orvieto R, Achiron A, Ben-Rafael Z et al. Intravenous immunoglobulin treatment for recurrent abortions caused by antiphospholipid antibodies. Fertil Steril. 1991; 56:1013-20. https://pubmed.ncbi.nlm.nih.gov/1743314
633. Cruzan S (US Department of Health and Human Services). FDA proposes alcohol warning for all OTC pain relievers. Rockville, MD; 1997 Nov 14. Press release No. P97-37.
635. Ryan TJ, Antman EM, Brooks NH et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: 1999 update: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). From ACC website. http://www.cardiosource.org/Science-And-Quality/Practice-Guidelines-and-Quality-Standards.aspx
636. Gersony WM. Diagnosis and management of Kawasaki disease. JAMA. 1991; 265:2699-703. https://pubmed.ncbi.nlm.nih.gov/2023352
637. Dajani SA, Taubert KA, Gerber MA et al. Diagnosis and therapy of Kawasaki disease in children. Circulation. 1993; 87:1776-80. https://pubmed.ncbi.nlm.nih.gov/8491037
638. Committee on Infectious Diseases, American Academy of Pediatrics. 2000 Red book: report of the Committee on Infectious Diseases. 25th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2000:353-4,360-3,624-38.
639. Alpha Therapeutics. Immune globulin intravenous (human) Venoglobulin-S 5% solution solvent detergent treated product information. Los Angeles, CA: 1997 Feb.
640. Immuno-U.S. Iveegam immune globulin intravenous (human) prescribing information. Rochester, MI: 1992 Jan.
641. Newburger JW, Takahashi M, Burns JC et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986; 315:341-7. https://pubmed.ncbi.nlm.nih.gov/2426590
642. Shulman ST. Recommendations for intravenous immunoglobulin therapy of kawasaki disease. Pediatr Inf Dis. 1992; 11:985-6.
643. Anon. Alcohol warning on over-the-counter pain medications. WHO Drug Info. 1998; 12:16.
644. Cruzan SM (US Food and Drug Administration). FDA announces new alcohol warnings for pain relievers and fever reducers. Rockville, MD; 1998 Oct 21. Press release No. 98-31.
645. Food and Drug Administration. Over-the-counter drug products containing analgesic/antipyretic active ingredients for internal use; required alcohol warning. 21 CFR Part 201. Final rule; technical amendments. [Docket No. 77N-094A] Fed Regist. 1999; 64:49652-55.
646. Food and Drug Administration. Internal analgesic, antipyretic, and antirheumatic drug products for over-the-counter human use; final rule for professional labeling of aspirin, buffered aspirin, and aspirin in combination with antacid drug products. 21 CFR Part 343. Final rule. [Docket No. 77N-094A] Fed Regist. 1998; 63:56802-19.
648. Anon. Pregnancy-related death associated with heparin and aspirin treatment for infertility, 1996. MMWR Morb Mortal Wkly Rep. 1998; 47:368-71. https://pubmed.ncbi.nlm.nih.gov/9603628
649. Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation. 5th ed. Baltimore, MD: Williams & Wilkins; 1998:73-81.
650. Rai R, Cohen H, Dave M et al. Randomised controlled trial of aspirin and aspirin plus heparin in pregnant women with recurrent miscarriage associated with phospholipid antibodies (or antiphospholipid antibodies). BMJ. 1997; 314:253-7. https://pubmed.ncbi.nlm.nih.gov/9022487
651. Khamashta MA. Antiphospholipid (Hughes’) syndrome: a treatable cause of recurrent pregnancy loss. BMJ. 1997; 314:244. https://pubmed.ncbi.nlm.nih.gov/9022479
652. American College of Obstetrics and Gynecology. Antiphospholipid syndrome. ACOG Educ Bull. 1998; 244:1-10.
653. American College of Obstetrics and Gynecology. Early pregnancy loss. ACOG Tech Bull. 1995; 212:1-7.
654. Kutteh WH. Antiphospholipid antibody–associated recurrent pregnancy loss: treatment with heparin and low-dose aspirin is superior to low-dose aspirin alone. Am J Obstet Gynecol. 1996; 174:1584-9. https://pubmed.ncbi.nlm.nih.gov/9065133
655. Silver RM, Branch DW. Recurrent miscarriage: autoimmune considerations. Clin Obstet Gynecol. 1994; 37:745-60. https://pubmed.ncbi.nlm.nih.gov/7955658
656. Sher G, Feinman M, Zouves C et al. High fecundity rates following in-vitro fertilization and embryo transfer in antiphospholipid antibody seropositive women treated with heparin and aspirin. Hum Reprod. 1994; 9:2278-83. https://pubmed.ncbi.nlm.nih.gov/7714144
657. Kutteh. Effect of antiphospholipid antibodies in women undergoing in-vitro fertilization: role of heparin and aspirin. Hum Reprod. 1997; 12:1171-5. https://pubmed.ncbi.nlm.nih.gov/9221995
658. Anon. Physicians’ health study report on aspirin. Circulation. 1988; 77(Suppl):1447A. https://pubmed.ncbi.nlm.nih.gov/3370779
659. Steering Committee of the Physicians’ Health Study Research Group. Final report of the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989; 321:129-35. https://pubmed.ncbi.nlm.nih.gov/2664509
660. Fuster V, Cohen M, Halperin J. Aspirin in the prevention of coronary disease. N Engl J Med. 1989; 321:183-5. https://pubmed.ncbi.nlm.nih.gov/2747748
661. Hennekens CH, Buring JE, Sandercock P et al. Aspirin and other antiplatelet agents in the secondary and primary prevention of cardiovascular disease. Circulation. 1989; 80:749-56. https://pubmed.ncbi.nlm.nih.gov/2676237
663. Hartney TJ. The Physicians’ Health Study: aspirin for the primary prevention of myocardial infarction. N Engl J Med. 1988; 924. Letter.
664. Shapiro S. The Physicians’ Health Study: aspirin for the primary prevention of myocardial infarction. N Engl J Med. 1988; 924. Letter.
665. Jain KM, Simoni EJ. The Physicians’ Health Study: aspirin for the primary prevention of myocardial infarction. N Engl J Med. 1988; 924. Letter.
666. Meade TW, Wilkes HC, Kelleher CC et al for the Medical Research Council’s General Practice Research Framework. Thrombosis Prevention Trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet. 1998; 351:233-41. https://pubmed.ncbi.nlm.nih.gov/9457092
667. Verheugt FWA. Aspirin, the poor man’s statin? Lancet. 1998; 351:227-8. Editorial.
668. Smith SC Jr, Blair SN, Criqui MH et al. Preventing heart attack and death in patients with coronary disease. Circulation. 1995; 92:2-4. https://pubmed.ncbi.nlm.nih.gov/7788911
670. Manson JE, Stampfer MJ, Colditz GA et al. A prospective study of aspirin use and primary prevention of cardiovascular disease in women. JAMA. 1991; 266:521-7. https://pubmed.ncbi.nlm.nih.gov/2061978
671. Appel LJ, Bush T. Preventing heart disease in women: another role for aspirin? JAMA. 1991; 266:565-6. Editorial.
672. Yusuf S, Wittes J, Friedman L. Overview of results of randomized clinical trials in heart disease. II: unstable angina, heart failure, primary prevention with aspirin, and risk factor modification. JAMA. 1988; 260:2259-63. https://pubmed.ncbi.nlm.nih.gov/3050165
673. Buring JE, Hennekens CH for the Women’s Health Study Research Group. The women’s health study: summary of the study design. J Myocardial Ischemia. 1992; 4:27-9.
674. He J, Whelton PK, Vu B et al. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. JAMA. 1998; 280:1930-5. https://pubmed.ncbi.nlm.nih.gov/9851479
675. Boissel JP. Individualizing aspirin therapy for prevention of cardiovascular events. JAMA. 1998; 280:1949-50. https://pubmed.ncbi.nlm.nih.gov/9851483
676. Young FE, Nightingale SL, Temple RA. The preliminary report of the findings of the aspirin component of the ongoing Physicians’ Health Study. JAMA. 1988; 259:3158-60. https://pubmed.ncbi.nlm.nih.gov/3367492
678. Murata T, Ushikubi F, Matsuoka T et al. Altered pain perception and inflamatory response in mice lacking prostacyclin receptor. Nature. 1997; 388:678-82. https://pubmed.ncbi.nlm.nih.gov/9262402
679. Smith WL, Garavito RM, DeWitt DL. Prostaglandin endoperoxide H synthases (cyclooxygenases)-1 and -2. J Biol Chem. 1996; 271:33157-60. https://pubmed.ncbi.nlm.nih.gov/8969167
680. Juul-Möller S, Edvardsson N, Jahnmatz B et al. Double-blind trial of aspirin in primary prevention of myocardial infarction in patients with stable chronic angina pectoris. Lancet. 1992; 340:1421-5. https://pubmed.ncbi.nlm.nih.gov/1360557
681. Underwood MJ, More RS. The aspirin papers: aspirin benefits patients with vascular disease and those undergoing revascularization. BMJ. 1994; 308:71-2. https://pubmed.ncbi.nlm.nih.gov/8298414
682. Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy—I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994; 308:81-106. https://pubmed.ncbi.nlm.nih.gov/8298418
683. Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy—II: maintenance of vascular graft or arterial patency by antiplatelet therapy. BMJ. 1994; 308:159-68. https://pubmed.ncbi.nlm.nih.gov/8312766
684. Théroux P, Waters D, Qiu S et al. Aspirin versus heparin to prevent myocardial infarction during the acute phase of unstable angina. Circulation. 1993; 88(Part 1):2045-8. https://pubmed.ncbi.nlm.nih.gov/8222097
687. Gavaghan TP, Gebski V, Baron DW. Immediate postoperative aspirin improves vein graft patency early and late after coronary artery bypass surgery: a placebo-controlled, randomized study. Circulation. 1991; 83:1526-33. https://pubmed.ncbi.nlm.nih.gov/2022014
688. Goldman S, Copeland J, Moritz T et al. Internal mammary artery and saphenous vein graft patency: effects of aspirin. Circulation. 1990; 82(Suppl IV):237-42.
689. Lembo NJ, Black AJR, Roubin GS et al. Effect of pretreatment with aspirin versus aspirin plus dipyridamole on frequency and type of acute complications of percutaneous transluminal coronary angioplasty. Am J Cardiol. 1990; 65:422-6. https://pubmed.ncbi.nlm.nih.gov/2407084
693. Cappelleri JC, Fiore LD, Brophy MT et al. Efficacy and safety of combined anticoagulant and antiplatelet therapy versus anticoagulant monotherapy after mechanical heart-valve replacement: a metaanalysis. Am Heart J. 1995; 130:547-52. https://pubmed.ncbi.nlm.nih.gov/7661074
694. Meschengieser SS, Carlos GF, Santarelli MT et al. Low-intensity oral anticoagulation plus low-dose aspirin versus high-intensity oral anticoagulation alone: a randomized trial in patients with mechanical prosthetic heart valves. J Thorac Cardiovasc Surg. 1997; 113:910-6. https://pubmed.ncbi.nlm.nih.gov/9159625
695. Albertal J, Sutton M, Pereyra D et al. Experience with moderate intensity anticoagulation and aspirin after mechanical valve replacement: a retrospective, non-randomized study. J Heart Valve Dis. 1993; 2:302-7. https://pubmed.ncbi.nlm.nih.gov/8269123
696. Altman R, Rouvier J, Gurfinkel E et al. Comparison of two levels of anticoagulant therapy in patients with substitute heart valves. J Thorac Cardiovasc Surg. 1991; 101:427-31. https://pubmed.ncbi.nlm.nih.gov/1999935
697. Nunez L, Aguado GM, Larrea JL et al. Prevention of thromboembolism using aspirin after mitral valve replacement with porcine bioprosthesis. Ann Thorac Surg. 1984; 37:84-7. https://pubmed.ncbi.nlm.nih.gov/6691742
699. International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19 435 patients with acute ischaemic stroke. Lancet. 1997; 349:1569-81. https://pubmed.ncbi.nlm.nih.gov/9174558
700. CAST (Chinese Acute Stroke Trial) Collaborative Group. CAST: randomised placebo-controlled trial of early aspirin use in 20 000 patients with acute ischaemic stroke. Lancet. 1997; 349:1641-9. https://pubmed.ncbi.nlm.nih.gov/9186381
701. Bristol-Myers Squibb. Excedrin Migraine (acetaminophen, aspirin, and caffeine) tablets product information. New York, NY; 1999.
702. Cruzan S. FDA approves first OTC drug for relief of migraine pain. FDA Talk Paper. Rockville, MD: Food and Drug Administration; 1998 Jan 14.
703. Bristol-Myers. Excedrin Migraine (acetaminophen, aspirin, and caffeine) tablets product monograph. Princeton, NJ; 1997.
704. Lipton RB, Stewart WF, Ryan RE et al. Efficacy and safety of acetaminophen, aspirin, and caffeine in alleviating migraine headache pain. Arch Neurol. 1998;55:210-7.
705. Caritis S, Sibai B, Hauth J et al. Low-dose aspirin to prevent preeclampsia in women at high risk. N Engl J Med. 1998; 338:701-5. https://pubmed.ncbi.nlm.nih.gov/9494145
706. Marcus LC, Marcus E. Low-dose aspirin for preeclampsia—the unresolved question. N Engl J Med. 1998; 338:756-8. https://pubmed.ncbi.nlm.nih.gov/9494153
707. American College of Obstetrics and Gynecology. Hypertension in pregnancy. ACOG Tech Bull. 1996; 219:1-8.
708. Sibai BM. Treatment of hypertension in pregnant women. N Engl J Med. 1996; 335:257-65. https://pubmed.ncbi.nlm.nih.gov/8657243
709. Lindheimer MD. Pre-eclampsia—eclampsia 1996: preventable? Have disputes on its treatment been resolved? Curr Opin Nephrol Hypertens. 1996; 5:452-8.
710. National High Blood Pressure Education Program Working Group. National High Blood Pressure Education Program Working Group report on high blood pressure in pregnancy. Am J Obstet Gynecol. 1990; 163:1689-1712.
711. Dekker GA, Sibai BM. Low-dose aspirin in the prevention of preeclampsia and fetal growth retardation: rationale, mechanisms, and clinical trials. Am J Obset Gynecol. 1993; 168:214-27.
712. Sibai BM, Caritis SN, Thom E et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. N Engl J Med. 1993; 329:1213-8. https://pubmed.ncbi.nlm.nih.gov/8413387
713. CLASP (Collaborative Low-Dose Aspirin Study in Pregnancy) Collaborative Group. CLASP: a randomised trial of low-dose aspirin for the prevention and treatment of preeclampsia among 9364 pregnant women. Lancet. 343:619-29.
714. Laskin CA, Bombardier C, Hannah ME et al. Prednisone and aspirin in women with autoantibodies and unexplained recurrent fetal loss. N Engl J Med. 1997; 337:148-53. https://pubmed.ncbi.nlm.nih.gov/9219700
715. ECPPA (Estudo Colaborativo para Prevencao da Pre-eclampsia com Aspirina) Collaborative Group. ECPPA: randomised trial of low dose aspirin for the prevention of maternal and fetal complications in high risk pregnant women. Br J Obstet Gynecol. 1996; 103:39-47.
717. Turpie AGG, Gent M, Laupacis A et al. A comparison of aspirin with placebo in patients treated with warfarin after heart-valve replacement. N Engl J Med. 1993; 329:524-9. https://pubmed.ncbi.nlm.nih.gov/8336751
718. Tamisier D, Vouhe PR, Vernant F et al. Modified Blalock-Taussig shunts: results in infants less than 3 months of age. Ann Thorac Surg. 1990; 49:797-801. https://pubmed.ncbi.nlm.nih.gov/1692681
719. Monagle P, Cochrane A, McCrindle B et al. Thromboembolic complications after fontan procedures: the role of prophylactic anticoagulation. J Thorac Cardiovasc Surg. 1998; 115:493-8. https://pubmed.ncbi.nlm.nih.gov/9535434
720. Fremes SE, Levinton C, Naylor CD et al. Optimal antithrombotic therapy following aortocoronary bypass: a meta-analysis. Eur J Cardiothorac Surg. 1993; 7(4):169-80. https://pubmed.ncbi.nlm.nih.gov/8481254
721. Henderson WG, Goldman S, Copeland JG et al. Antiplatelet or anticoagulant therapy after coronary artery bypass surgery. A meta-analysis of clinical trials. Ann Intern Med. 1989; 111:743-50. https://pubmed.ncbi.nlm.nih.gov/2679289
722. van der Meer J, Hillege HL, Kootstra GJ et al. Prevention of one-year vein-graft occlusion after aortocoronary-bypass surgery: a comparison of low-dose aspirin, low-dose aspirin plus dipyridamole, and oral anticoagulants. Lancet. 1993; 342:257-64. https://pubmed.ncbi.nlm.nih.gov/8101300
723. van der Meer J, for the CABADAS Research Group. Prevention of graft occlusion by aspirin, dipyridamole, and oral anticoagulants. Lancet. 1993; 342:807.
724. Loeliger EA. Prevention of graft occlusion by aspirin, dipyridamole, and oral anticoagulants. Lancet. 1993; 342:806. https://pubmed.ncbi.nlm.nih.gov/8103893
725. Bayer Corporation Consumer Care Division. Alka-Seltzer Original (aspirin, sodium bicarbonate, citric acid) effervescent antacid pain reliever patient information (undated). In: Physicians’ desk reference for nonprescription drugs. 19th ed. Montvale, NJ: Medical Economics Company Inc; 1998:604-5.
726. Coulam CB, Clark DB, Beer AE et al. Current clinical options for diagnosis and treatment of recurrent spontaneous abortion. Am J Reprod Health. 1997; 38:57-74.
727. Roux S, Christeller S, Ludin E. Effects of aspirin on coronary reocclusion and recurrent ischemia after thrombolysis: a meta-analysis. J Am Coll Cardiol. 1992; 19:671-7. https://pubmed.ncbi.nlm.nih.gov/1531663
728. Gibbons RJ, Chatterjee K, Daley J et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Chronic Stable Angina. J Am Coll Cardiol. 1999; 33:2092-197. https://pubmed.ncbi.nlm.nih.gov/10362225
729. Riendeau D, Charleson S, Cromlish W et al. Comparison of the cyclooxygenase-1 inhibitory properties of nonsteroidal anti-inflammatory drugs (NSAIDs) and selective COX-2 inhibitors, using sensitive microsomal and platelet assays. Can J Physiol Pharmacol. 1997; 75:1088-95. https://pubmed.ncbi.nlm.nih.gov/9365818
730. DeWitt DL, Bhattacharyya D, Lecomte M et al. The differential susceptibility of prostaglandin endoperoxide H synthases-1 and -2 to nonsteroidal anti-inflammatory drugs: aspirin derivatives as selective inhibitors. Med Chem Res. 1995; 5:325-43.
731. Cryer B, Dubois A. The advent of highly selective inhibitors of cyclooxygenase—a review. Prostaglandins Other Lipid Mediators. 1998; 56:341-61. https://pubmed.ncbi.nlm.nih.gov/9990677
732. Simon LS. Role and regulation of cyclooxygenase-2 during inflammation. Am J Med. 1999; 106(Suppl 5B):37-42S.
733. Morrison BW, Daniels SE, Kotey P et al. Rofecoxib, a specific cyclooxygenase-2 inhibitor, in primary dysmenorrhea: a randomized controlled trial. Obstet Gynecol. 1999; 94:504-8. https://pubmed.ncbi.nlm.nih.gov/10511349
734. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999; 340:1888-99. https://pubmed.ncbi.nlm.nih.gov/10369853
735. Hawkey CJ. COX-2 inhibitors. Lancet. 1999; 353:307-14. https://pubmed.ncbi.nlm.nih.gov/9929039
736. Kurumbail RG, Stevens AM, Gierse JK et al. Structural basis for selective inhibition of cyclooxygenase-2 by anti-inflammatory agents. Nature. 1996; 384:644-8. https://pubmed.ncbi.nlm.nih.gov/8967954
738. Boehringer Ingelheim Pharmaceuticals. Aggrenox (aspirin/ extended release dipyridamole) capsules prescribing information. Ridgefield CT; 2005 Aug 5.
739. Diener HC. Dipyridamole trials in stroke prevention. Neurology. 1998; 51(Suppl.3):S17-9. https://pubmed.ncbi.nlm.nih.gov/9744826
740. Antman EM, Fox KM et al. Guidelines for the diagnosis and management of unstable angina and non-Q-wave myocardial infarction: proposed revisions. Am Heart J. 2000; 139:461-75. https://pubmed.ncbi.nlm.nih.gov/10689261
741. Bonow RO, Carabello B, de Leon AC et al. ACC/AHA guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 1998; 32:1486-588. https://pubmed.ncbi.nlm.nih.gov/9809971
742. Cairns JA, Kennedy JW, Fuster V. Coronary thrombolysis. Chest. 1998; 114:(Suppl 5S):634S-57S.
743. Forbes CD et al. Secondary stroke prevention with low-dose aspirin, sustained release dipyridamole alone and in combination. Thromb Res. 1998; 92(Suppl.1):S1-6.
744. Prystowsky EN, Benson W Jr, Fuster V et al. Management of patients with atrial fibrillation: a statement for healthcare professionals from the subcommittee on electrocardiography and electrophysiology, American Heart Association. Circulation. 1996; 93:1262-77. https://pubmed.ncbi.nlm.nih.gov/8653857
745. Albers GW, Hart RG, Lutsep HL et al. Supplement to the guidelines for the management of transient ischemic attacks: a statement from the Ad Hoc Committee on Guidelines for the Management of Transient Ischemic Attacks, American Heart Association. Stroke. 1999; 30:2502-11. https://pubmed.ncbi.nlm.nih.gov/10548693
746. Salem DN, Levine HJ, Pauker SG et al. Antithrombotic therapy in valvular heart disease. Chest. 1998; 114:(Suppl 5S):590S-601S.
747. Laupacis A, Albers G, Dalen J et al. Antithrombotic therapy in atrial fibrillation. Chest. 1998; 114:(Suppl 5S):579S-89S.
748. Segal JB, McNamara RL, Miller MR et al. Prevention of thromboembolism in atrial fibrillation: a meta-analysis of trials of anticoagulant and antiplatelet drugs. J Gen Intern Med. 2000; 15:56-67. https://pubmed.ncbi.nlm.nih.gov/10632835
749. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on antithrombotic therapy in chronic atrial fibrillation. Am J Health-Syst Pharm. 1998; 55:376-81. https://pubmed.ncbi.nlm.nih.gov/9504198
750. Agency for Heathcare Research and Quality. Management of new onset atrial fibrillation. Summary. Rockville, Md. Agency for Healthcare Research and Quality, 2000 May. Evidence report/technology assessment: number 12. (AHRQ publicatin no. 00-E006).
751. Latini R, Tognoni G, Maggioni AP et al. Clinical effects of early angiotensin-converting enzyme inhibitor treatment for acute myocardial infarction are similar in the presence and absence of aspirin. J Am Coll Cardiol. 2000; 35:1801-7. https://pubmed.ncbi.nlm.nih.gov/10841227
752. Hall D. The aspirin-angiotensin-converting enzyme inhibitor tradeoff: to halve and halve not. J Am Coll Cardiol. 2000; 35:1808-12. https://pubmed.ncbi.nlm.nih.gov/10841228
753. Anon. Consensus recommendations for the management of congestive heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Part II. Management of heart failure: approaches to the prevention of heart failure. Am J Cardiol. 1999; 83:9-38A.
754. Aspirin interactions: captopril. In: Hansten PD, Horn JR. Drug interactions and updates. Vancouver, WA: Applied Therapeutics, Inc; 1997:62-3.
755. Diener HC, Cunha L, Forbes C et al. European stroke prevention study 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996; 143:1-13. https://pubmed.ncbi.nlm.nih.gov/8981292
756. Merck. Varivax (varicella virus vaccine live [Oka/Merck/]) prescribing information. West Point, PA; 2000 Feb.
757. Centers for Disease Control and Prevention. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 1996; 45(RR-11):1-25. https://pubmed.ncbi.nlm.nih.gov/8531914 https://www.cdc.gov/mmwr/PDF/rr/rr4511.pdf
758. Anon. Drugs for rheumatoid arthritis. Med Lett Drugs Ther. 2000; 42:57-64. https://pubmed.ncbi.nlm.nih.gov/10887424
759. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines.
761. Ridker PM, Cushman M, Stampfer MJ et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997; 336:973-9. https://pubmed.ncbi.nlm.nih.gov/9077376
762. Ginsberg JS, Greer I, Hirsch J. Use of antithrombotic agents during pregnancy. Chest. 2001; 119(Suppl.):122S-131S. https://pubmed.ncbi.nlm.nih.gov/11157646
763. Hyers TM, Agnelli G, Hull RD et al. Antithrombotic therapy for venous thromboembolic disease. Chest. 2001; 119(Suppl.):176S-93S. https://pubmed.ncbi.nlm.nih.gov/11157648
766. Stroke Prevention in Atrial Fibrillation Investigators. Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrilllation III randomised clinical trial. Lancet. 1996; 348:633-8. https://pubmed.ncbi.nlm.nih.gov/8782752
767. SPAF III Writing Committee for the Stroke Prevention in Atrial Fibrillation Investigators. Patients with nonvalvular atrial fibrillation at low risk of stroke during treatment with aspirin: stroke prevention in atrial fibrillation III study. JAMA. 1998; 279:1273-7. https://pubmed.ncbi.nlm.nih.gov/9565007
778. Matchar DB, Young WB, Rosenberg JH et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks. St. Paul, MN; 2001. From the American Academy of Neurology web site. http://www.aan.com
779. Bayer Corporation Consumer Care Division. Alka-Seltzer Original (aspirin, sodium bicarbonate, citric acid) effervescent antacid pain reliever product information. In: Physicians’ desk reference for nonprescription drugs. 23rd ed. Montvale, NJ: Medical Economics Company Inc; 2002.
781. Mangano DT, for the Multicenter Study of Perioperative Ischemia Research Group. Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002; 347:1309-17. https://pubmed.ncbi.nlm.nih.gov/12397188
782. Topol EJ. Aspirin with bypass surgery—from taboo to new standard of care. N Engl J Med. 2002; 347:1359-60. https://pubmed.ncbi.nlm.nih.gov/12397195
783. U.S. Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events. Recommendations and rationale. Available from AHRQ website. Accessed December 18, 2002. http://www.ahrq.gov/clinic/uspstf09/aspirincvd/aspcvdrs.htm
784. Guise JM, Mahon SM, Aickin M et al. Aspirin for the primary prevention of cardiovascular events: a summary of the evidence. Available from AHRQ website. Accessed December 18, 2002. http://www.ahrq.gov/clinic/uspstf09/aspirincvd/aspcvdart.htm
785. Hansson L, Zanchetti A, Carruthers SG et al et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998; 351:1755–62. https://pubmed.ncbi.nlm.nih.gov/9635947
786. Collaborative Group of the Primary Prevention Project (PPP). Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Lancet. 2001; 357:89–95. https://pubmed.ncbi.nlm.nih.gov/11197445
787. Kjeldsen SE, Kolloch RE, Leonetti G et al. Influence of gender and age on preventing cardiovascular disease by antihypertensive treatment and acetylsalicylic acid. The HOT study. Hypertension Optimal Treatment. J Hypertens. 2000; 18:629-42. https://pubmed.ncbi.nlm.nih.gov/10826567
788. Catella-Lawson F, Reilly MP, Kapoor SC et al. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2001; 345:1809-17. https://pubmed.ncbi.nlm.nih.gov/11752357
789. Imperiale TF. Aspirin and the prevention of colorectal cancer. N Engl J Med. 2003; 348:879-80. https://pubmed.ncbi.nlm.nih.gov/12621130
790. Sandler RS, Halabi S, Baron JA et al. A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. N Engl J Med. 2003; 348:883-90. https://pubmed.ncbi.nlm.nih.gov/12621132
791. Baron JA, Cole BF, Sandler RS et al. A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med. 2003; 348:891-9. https://pubmed.ncbi.nlm.nih.gov/12621133
792. Thun MJ, Henley SJ, Patrono C. Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. J Natl Cancer Inst. 2002 94:252-66.
793. Strul H, Arber N. Non-steroidal anti-inflammatory drugs and selective apoptotic anti-neoplastic drugs in the prevention of colorectal cancer: the role of super aspirins. Isr Med Assoc J. 2000; 2:695-702. https://pubmed.ncbi.nlm.nih.gov/11062772
794. Janne PA, Mayer RJ. Chemoprevention of colorectal cancer. N Engl J Med. 2000; 342:1960-8. https://pubmed.ncbi.nlm.nih.gov/10874065
795. Arber N. Do NSAIDs prevent colorectal cancer? Can J Gastroenterol. 2000; 14:299-307.
796. Ladabaum U, Sowers M. Potential population-wide impact of aspirin on colon cancer mortality. Gastroenterology. 1998; 115:514-5. https://pubmed.ncbi.nlm.nih.gov/9758548
797. Rosenberg L, Louik C, Shapiro S. Nonsteroidal antiinflammatory drug use and reduced risk of large bowel carcinoma. Cancer. 1998; 82:2326-33. https://pubmed.ncbi.nlm.nih.gov/9635524
798. Ruffin MT, Krishnan K, Rock CL et al. Suppression of human colorectal mucosal prostaglandins: determining the lowest effective aspirin dose. J Natl Cancer Inst. 1997; 89:1152-60. https://pubmed.ncbi.nlm.nih.gov/9262254
799. Thun MJ. Aspirin and gastrointestinal cancer. Adv Exp Med Biol. 1997; 400A:395-402. https://pubmed.ncbi.nlm.nih.gov/9547582
800. Goldberg Y. Aspirin and colon cancer. N Engl J Med. 1996; 334:800-1. https://pubmed.ncbi.nlm.nih.gov/8592564
801. Marcus AJ. Aspirin as prophylaxis against colorectal cancer. N Engl J Med. 1995; 333:656-8. https://pubmed.ncbi.nlm.nih.gov/7637730
802. Giovannucci E, Egan KM, Hunter DJ et al. Aspirin and the risk of colorectal cancer in women. N Engl J Med. 1995; 333:609-14. https://pubmed.ncbi.nlm.nih.gov/7637720
803. Muller AD, Sonnenberg A, Wasserman IH. Diseases preceding colon cancer. A case-control study among veterans. Dig Dis Sci. 1994; 39:2480-4. https://pubmed.ncbi.nlm.nih.gov/7956619
804. Schreinemachers DM, Everson RB. Aspirin use and lung, colon, and breast cancer incidence in a prospective study. Epidemiology. 1994; 5:138-46. https://pubmed.ncbi.nlm.nih.gov/8172988
805. G.D. Searle & Co. Celebrex (celecoxib) capsules prescribing information. Skokie, IL; 2001 Oct.
806. Kawamori T, Rao CV, Seibert K et al. Chemopreventive activity of celecoxib, a specific cyclooxygenase-2 inhibitor, against colon carcinogenesis. Cancer Res. 1998; 58:409-12.
807. Steinbach G, Lynch PM, RKS Phillips et al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med. 2000; 342:1946-52.
808. Sheehan KM, Sheahan K, O’Donoghue DP et al. The relationship between cyclooxygenase-2 expression and colorectal cancer. JAMA. 1999; 282:1254-7.
809. Reddy BS, Hirose Y, Lubet R et al. Chemoprevention of colon cancer by specific cyclooxygenase-2 inhibitor, celecoxib, administered during different stages of carcinogenesis. Cancer Res. 2000; 60:293-7.
810. Fournier DB, Gordon GB. COX-2 and colon cancer: potential targets for chemoprevention. J Cell Biochem. 2000; 34:97-102.
811. Jacoby RF, Seibert K, Cole CE et al. The cyclooxygenase-2 inhibitor celecoxib is a potent preventive and therapeutic agent in the min mouse model of adenomatous polyposis. Cancer Res. 2000; 60:5040-4.
812. Cryer B, Dubois A. The advent of highly selective inhibitors of cyclooxygenase--a review. Prostaglandins Lipid Mediators. 1998; 56:341-61.
813. Vane JR, Bakhle YS, Botting RM. Cyclooxygenases 1 and 2. Ann Rev Pharmacol Toxicol. 1998; 38:97-120.
814. Reviewer’s comments (personal observations).
815. Duley L, Henderson-Smart D, Knight M et al. Antiplatelet drugs for prevention of pre-eclampsia and its consequences: systematic review. BMJ. 2001; 322:329-33. https://pubmed.ncbi.nlm.nih.gov/11159655
816. Coomarasamy A, Honest H, Papaioannou S et al. Aspirin for prevention of preeclampsia in women with historical risk factors: a systematic review. Obstet Gynecol. 2003; 101:1319-32. https://pubmed.ncbi.nlm.nih.gov/12798543
817. Duley L, Henderson-Smart D, Knight M et al. Antiplatelet drugs for prevention of pre-eclampsia and its consequences: systematic review. BMJ. 2001; 322:329-33. https://pubmed.ncbi.nlm.nih.gov/11159655
821. Antman EM, Anbe DT, Armstrong PW et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction. a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). 2004. From ACC website. http://www.cardiosource.org/Science-And-Quality/Practice-Guidelines-and-Quality-Standards.aspx
822. Snow V, Barry P, Fihn SD et al. Primary care management of chronic stable angina and asymptomatic suspected or known coronary artery disease: a clinical practice guideline from the American College of Physicians/American College of Cardiology Chronic Stable Angina Panel. Ann Intern Med. 2004; 141:562-567. https://pubmed.ncbi.nlm.nih.gov/15466774
829. Adams H, Adams R, Del Zoppo G et al. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update. A scientific statement from the Stoke Council of the American Heart Association/American Stroke Association. Stoke. 2005; 36:916-21.
835. Adams H, Adams R, Brott T et al. Guidelines for the early management of patients with ischemic stroke. A scientific statement from the Stoke Council of the American Heart Association/American Stroke Association. Stoke. 2003; 34:1056-83.
836. Insight. Anacin Extra Strength Pain Relieve tablets product information. From Insight web site. Accessed 2005 Dec 20. http://www.prestigebrands.com/
837. Heritage. Aspergum Aspirin Pain Reliever, Orange Flavor Gum Tablets product information. From web site. Accessed 2007 Jun 1. http://www.medshopexpress.com/132703.html
838. Bayer. Alka-Seltzer Lemon Lime product information. Available from Alka-Seltzer website. Accessed 2007 May 10. http://www.alkaseltzer.com
839. Bayer. Aspirin Regimen Bayer 81 mg, Aspirin Regimen Bayer 325 mg, Delayed Release Enteric Aspirin, Adult Low Strength 81 mg Tablets, Regular Strength 325 mg Caplets product information. From PDR Electronic Library. Assessed 2005 Nov. 8. http://www.thomsonhc.com
840. Bayer. Genuine Bayer Aspirin product information. 2005. Available from Bayer website. Accessed 2007 Jun 1. http://www.wonderdrug.com
841. Bayer. Children’s Chewable Aspirin-Cherry product information. 2005. Available from Bayer website. Accessed 2007 Jun 1. http://www.wonderdrug.com
842. Bayer. Womens’ Aspirin Plus Calcium product information. 2005. Available from Bayer website. Accessed 2005 Nov 9. http://www.wonderdrug.com
843. Bayer. Alka-Seltzer Original product information. undated. Available from Alka-Seltzer website. Accessed 2005 Nov 9. http://www.alkaseltzer.com
844. Bayer. Alka-Seltzer Extra Strength product information. Available from Alka-Seltzer website. Accessed 2005 Nov 9. http://www.alkaseltzer.com
845. Bates SM, Greer IA, Hirsh J et al.. Use of antithrombotic agents during pregnancy. Chest. 2004; 126(Suppl):627-44S.
846. Ridker PM, Cook NR, Lee I-M et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005; 352:1293-304. https://pubmed.ncbi.nlm.nih.gov/15753114
847. Levin RI. The puzzle of aspirin and sex. N Engl J Med. 2005; 352:1366-8. Editorial. https://pubmed.ncbi.nlm.nih.gov/15755763
848. Ridker PM, Buring JE. Aspirin in the prevention of cardiovascular disease in women. N Engl J Med. 2005; 352:2752. Reply to Letter to the Editor. https://pubmed.ncbi.nlm.nih.gov/15987928
849. Schwartz DJ. Aspirin in the prevention of cardiovascular disease in women. N Engl J Med. 2005; 352:2751. Letter. https://pubmed.ncbi.nlm.nih.gov/15987927
850. Dalen JE. Aspirin in the prevention of cardiovascular disease in women. N Engl J Med. 2005; 352:2751. Letter. https://pubmed.ncbi.nlm.nih.gov/15991356
851. Jochmann N, Stangl K, Garbe E et al. Female-specific aspects in the pharmacotherapy of chronic cardiovascular diseases. Eur Heart J. 2005; 26:1585-95. https://pubmed.ncbi.nlm.nih.gov/15996977
852. COMMIT (ClOpidogrel and Metoprolol in Myocardial Infarction Trial) collaborative group. Addition of clopidogrel to aspirin in 45 852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005; 366:1607-11.
853. Sabatine MS. Something old, something new: β blockers and clopidogrel in acute myocardial infarction. Lancet. 2005; 366:1587-9. Editorial. https://pubmed.ncbi.nlm.nih.gov/16271628
854. Sabatine MS, Cannon CP, Gibson M et al, for the Clopidogrel as Adjunctive Reperfusion Therapy (CLARITY)–Thrombolysis in Myocardial Infarction (TIMI) 28 Investigators. Effect of clopidogrel pretreatment before percutaneous coronary intervention in patients with ST-elevation myocardial infarction treated with fibrinolytics The PCI-CLARITY Study. JAMA. 2005; 294:1224-32. https://pubmed.ncbi.nlm.nih.gov/16143698
855. Sabatine MS, Cannon CP, Gibson CM et al, for the CLARITY-TIMI 28 investigators. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med. 2005; 352:1179-89. https://pubmed.ncbi.nlm.nih.gov/15758000
856. Lange RA, Hillis LD. Concurrent antiplatelet and fibrinolytic therapy. N Engl J Med. 2005; 352:1179-89. Editorial. https://pubmed.ncbi.nlm.nih.gov/15758000
857. American College of Obstetricians and Gynecologists. Antiphospholipid syndrome. ACOG Practice Bulletin No. 68. Obstet Gynecol. 2005; 106:1113-21. https://pubmed.ncbi.nlm.nih.gov/16260543
858. FDA. New information for healthcare professionals: Concomitant use of ibuprofen and aspirin. 2006 Sep. From FDA website. Accessed 10 May 2007. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm125222.htm
859. Food and Drug Administration. Concomitant use of ibuprofen and aspirin: potential for attenuation of the antiplatelet effect of aspirin. FDA science paper. 2006 Sep 8. From FDA website. Accessed 10 May 2007. http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM161282.pdf
860. Capone ML, Sciulli MG, Tacconelli S et al. Pharmacodynamic interaction of naproxen with low-dose aspirin in healthy subjects. J Am Coll Cardiol. 2005; 45:1295-301. https://pubmed.ncbi.nlm.nih.gov/15837265
861. US Food and Drug Administration. Proposed NSAID Package Insert Labeling Template 1. From the FDA website. Accessed 17 Oct 2006. http://www.fda.gov
863. Chimowitz MI, Lynn MJ, Howlett-Smith H et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005; 352:1305-16. https://pubmed.ncbi.nlm.nih.gov/15800226
864. Cook NR, Lee IM, Gaziano JM et al. Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized clinical trial. JAMA. 2005; 294:47–55. https://pubmed.ncbi.nlm.nih.gov/15998890
866. Lansky AJ, Hochman JS, Ward PA et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professional from the American Heart Association. Circulation. 2005; 111:940-3 https://pubmed.ncbi.nlm.nih.gov/15687113
868. The Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001; 345:494-502. https://pubmed.ncbi.nlm.nih.gov/11519503
869. Mehta SR, Yusuf S, Peters RJG et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001; 358:527-33. https://pubmed.ncbi.nlm.nih.gov/11520521
870. Gonzalez-Perez A, Garcia Rodriguez LA, Lopez-Ridaura R. Effects of non-steroidal anti-inflammatory drugs on cancer sites other than the colon and rectum: a meta-analysis. BMC Cancer. 2003; 3:28. https://pubmed.ncbi.nlm.nih.gov/14588079
871. Garcia Rodriguez LA, Huerta-Alvarez C. Reduced risk of colorectal cancer among long-term users of aspirin and nonaspirin nonsteroidal antiinflammatory drugs. Epidemiology. 2001; 12:88-93. https://pubmed.ncbi.nlm.nih.gov/11138826
872. Asano TK, McLeod RS. Nonsteroidal antiinflammatory drugs and aspirin for the prevention of colorectal adenomas and cancer: a systematic review. Dis Colon Rectum. 2004; 47:665-73. https://pubmed.ncbi.nlm.nih.gov/15054679
873. Khuder SA, Mutgi AB. Breast cancer and NSAID use: a meta-analysis. Br J Cancer. 2001; 84:1188-92. https://pubmed.ncbi.nlm.nih.gov/11336469
874. Gann PH, Manson JE, Glynn RJ et al. Low-dose aspirin and incidence of colorectal tumors in a randomized trial. J Natl Cancer Inst. 1993; 85:1220-4. https://pubmed.ncbi.nlm.nih.gov/8331682
875. Baron JA, Cole BF, Sandler RS et al. A randomized trial to prevent colorectal adenomas. N Engl J Med. 2003; 348:891-9. https://pubmed.ncbi.nlm.nih.gov/12621133
876. Sturmer T, Glynn RJ, Lee IM et al. Aspirin use and colorectal cancer: post-trial follow-up data from the Physicians’ Health Study. Ann Intern Med. 1998; 128:713-20. https://pubmed.ncbi.nlm.nih.gov/9556464
877. Holick CN, Michaud DS, Leitzman MF et al. Aspirin use and lung cancer in men. Br J Cancer. 2003; 89:1705-8. https://pubmed.ncbi.nlm.nih.gov/14583773
880. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004; 109:672-93.
882. Goldstein LB, Adams R, Albers MJ et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council. Stroke. 2006; 37:1583-1633.
883. Algra A, for the ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006; 367:1665-73. https://pubmed.ncbi.nlm.nih.gov/16714187
885. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Available from ACC website. Accessed 2006 Nov 10. http://content.onlinejacc.org/data/Journals/JAC/23023/08002.pdf
886. Grines CL, Bonow RO, Casey DE et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stenosis. Circulation. 2007; 115:813-8. https://pubmed.ncbi.nlm.nih.gov/17224480
887. Stone GW, Aronow HD. Long-term care after percutaneous coronary intervention: focus on the role of antiplatelet therapy. Mayo Clin Proc. 2006; 81:641-52. https://pubmed.ncbi.nlm.nih.gov/16706262
888. Center for Devices and Radiological Health, Food and Drug Administration. Update to FDA statement on coronary drug-eluting stents. Rockville, MD: Food and Drug Administration; 2007 Jan 4. Available from FDA website. Accessed 2007 Mar 13. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/medsun/news/printer.cfm?id=575
889. Serruys PW, Kutryk MJ, Ong AT. Coronary artery stents. N Engl J Med. 2006; 354:483-95. https://pubmed.ncbi.nlm.nih.gov/16452560
890. Pfisterer M, Brunner-La Rocca HP, Buser PT et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents. JACC. 2006; 48:2584-91. https://pubmed.ncbi.nlm.nih.gov/17174201
891. Eisenstein EL, Anstrom KJ, Kong DF et al. Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation. JAMA. 2007;297:159-168.
892. Kereiakes DJ. Does clopidogrel each day keep stent thrombosis away? JAMA. 2007; 297:209-11. Editorial.
893. Spertus JA, Kettelkamp R, Vance C et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement. Results from the PREMIER registry. Circulation. 2006; 113:2803-9. https://pubmed.ncbi.nlm.nih.gov/16769908
894. Luscher TF, Steffel J, Eberli FR et al. Drug-eluting stent and coronary thrombosis. Biological mechanisms and clinical implications. Circulation. 2007; 115:1051-8. https://pubmed.ncbi.nlm.nih.gov/17325255
895. Jeremias A, Sylvia B, Bridges J et al. Stent thrombosis after successful sirolimus-eluting stent implantation. Circulation. 2004 109:1930-2.
896. Ong ATL, McFadden EP, Regar E et al. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. JACC. 2005; 45:2088-92. https://pubmed.ncbi.nlm.nih.gov/15963413
897. Kastrati A, Mehilli J, Pache J et al. Analysis of 14 trials comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med. 2007; 356:1030-9. https://pubmed.ncbi.nlm.nih.gov/17296823
898. Spaulding C, Daemen J, Boersma E et al. A pooled analysis of data comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med. 2007; 356:989-97. https://pubmed.ncbi.nlm.nih.gov/17296825
899. Farb A, Boam AB. Stent thrombosis redux—the FDA perspective. N Engl J Med. 2007; 356:984-7. Commentary. https://pubmed.ncbi.nlm.nih.gov/17296827
900. Stone GW, Moses JW, Ellis SG et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med. 2007; 356:998-1008. https://pubmed.ncbi.nlm.nih.gov/17296824
902. Shuchman M. Debating the risks of drug-eluting stents. N Engl J Med. 2007; 356:325-8. Commentary. https://pubmed.ncbi.nlm.nih.gov/17251527
903. Maisel WH. Unanswered questions—drug-eluting stents and the risk of late thrombosis. N Engl J Med. 2007; 356:981-4. Editorial. https://pubmed.ncbi.nlm.nih.gov/17296826
904. Curfman GD, Morrissey S, Jarcho JA et al. Drug-eluting coronary stents—promise and uncertainty. N Engl J Med. 2007; 356:1059-60. Editorial. https://pubmed.ncbi.nlm.nih.gov/17296828
905. Pepine CJ. Aspirin and newer orally active antiplatelet agents in the treatment of the post-myocardial infarction patient. J Am Coll Cardiol. 1998; 32:1126-8. https://pubmed.ncbi.nlm.nih.gov/9768742
906. Bayer Healthcare. Bayer Aspirin regular strength 325 mg, and low strength 81 mg tablets prescribing information. From PDR Electronic Library. Assessed 2007 Mar 13. http://www.thomsonhc.com
907. Campbell CL, Smyth S, Montalescot G et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007; 297(May 9):2018-24. https://pubmed.ncbi.nlm.nih.gov/17488967
916. Newburger JW, Takahashi M, Gerber MA et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004; 110:2747-71. https://pubmed.ncbi.nlm.nih.gov/15505111
917. Lyden P. Thrombolytic therapy for acute stroke — not a moment to lose. N Engl J Med. 2008; 359:1393-5. Editorial. https://pubmed.ncbi.nlm.nih.gov/18815401
918. Lees KR, Bluhmki E, von Kummer R et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010; 375:1695-703. https://pubmed.ncbi.nlm.nih.gov/20472172
919. Saver JL, Levine SR. Alteplase for ischaemic stroke—much sooner is much better. Lancet. 2010; 375:1667-8. Commentary. https://pubmed.ncbi.nlm.nih.gov/20472152
920. Adams HP Jr, del Zoppo G, Alberts MJ et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Stroke. 2007; 38:1655-1711. https://pubmed.ncbi.nlm.nih.gov/17431204
921. The Canadian Stroke Strategy. Canadian best practice recommendations for stroke care (updated 2008). CMAJ. 2008; 179 (12 suppl):E1-E93.
922. del Zoppo GJ, Saver JL, Jauch EC et al on behalf of the American Heart Association Stroke Council. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009; 40;2945-8. https://pubmed.ncbi.nlm.nih.gov/19478221
923. Bluhmki E, Ángel Chamorro, Antoni Dávalos et al. Stroke treatment with alteplase given 3.0–4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol. 2009; 8: 1095–102. https://pubmed.ncbi.nlm.nih.gov/19850525
927. The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. N Engl J Med. 1990; 323:1505-11. https://pubmed.ncbi.nlm.nih.gov/2233931
928. Singer DE. Randomized trials of warfarin for atrial fibrillation. N Engl J Med. 1992; 327:1451-3. https://pubmed.ncbi.nlm.nih.gov/1406862
929. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. Arch Intern Med. 1987; 147:1561-4. https://pubmed.ncbi.nlm.nih.gov/3632164
930. Prystowsky EN, Benson W Jr, Fuster V et al. Management of patients with atrial fibrillation: a statement for healthcare professionals from the subcommittee on electrocardiography and electrophysiology, American Heart Association. Circulation. 1996; 93:1262-77. https://pubmed.ncbi.nlm.nih.gov/8653857
931. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on antithrombotic therapy in chronic atrial fibrillation. Am J Health-Syst Pharm. 1998; 55:376-81. https://pubmed.ncbi.nlm.nih.gov/9504198
932. Segal JB, McNamara RL, Miller MR et al. Prevention of thromboembolism in atrial fibrillation: a meta-analysis of trials of anticoagulant and antiplatelet drugs. J Gen Intern Med. 2000; 15:56-67. https://pubmed.ncbi.nlm.nih.gov/10632835
935. Goldstein LB, Adams R, Becker K et al. Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation. 2001: 103:163-82.
937. Srinivasan A, Budnitz D, Shehab N et al. Infant deaths associated with cough and cold medications—two states, 2005. MMWR Morb Mortal Wkly Rep. 2007; 56:1-4. https://pubmed.ncbi.nlm.nih.gov/17218934
938. Bayer. Genuine Bayer Aspirin, Aspirin Regimen Bayer 325 mg, Aspirin Regimen Bayer 81 mg, Bayer Women’s Aspirin with Calcium, Aspirin Regimen Bayer Childrens Chewable 81 mg tablets professional labeling. From PDR Electronic Library. Assessed 2004 Feb 2.
939. Food and Drug Administration. Cough and cold medications in children less than two years of age. Rockville, MD; 2007 Jan 12. From FDA website.
940. Bayer. Bayer Tablets, Aspirin Pain Reliever. From Drugstore.com web site. Assessed 2004 Feb 2.
941. Food and Drug Administration. Internal analgesic, antipyretic, and antirheumatic drug products for over-the-counter human use: proposed amendment of the tentative final monograph; required warnings and other labeling. 21 CFR Parts 201 and 343. Proposed rule. (Docket No. 1977N-0094L). Fed Regist. 2006; 71:77314-52. Available from FDA website. Accessed 2007 Mar 8.
943. Rosedale Therapeutics. Easprin (aspirin) delayed-release tablets. Bristol, TN; 2004 Jan
944. Gage BF, Waterman AD, Shannon W et al. Validation of clinical classification schemes for predicting stroke. JAMA. 2001; 285:2864-70. https://pubmed.ncbi.nlm.nih.gov/11401607
945. Gage BF, van Walraven C, Pearce L et al. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation. 2004; 110:2287-92. https://pubmed.ncbi.nlm.nih.gov/15477396
946. Novartis. Voltaren-XR (diclofenac sodium extended-release tablets) prescribing information. East Hanover, NJ; 2006 Jan.
947. Novartis. Cataflam (diclofenac potassium immediate-release tablets) prescribing information. East Hanover, NJ; 2005 Jul.
948. Roche. EC-Naprosyn (naproxen) delayed-release tablets, Naprosyn (naproxen) tablets, Anaprox/Anaprox DS (naproxen sodium) tablets, and Naprosyn (naproxen) suspension prescribing information. Nutley, NJ; 2007.
949. Campbell CL, Smyth S, Montalescot G et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007; 297(May 9):2018-24. https://pubmed.ncbi.nlm.nih.gov/17488967
950. Hacke W, Kaste M, Bluhmki E et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317-29. https://pubmed.ncbi.nlm.nih.gov/18815396
951. Kirthi V, Derry S, Moore RA et al. Aspirin with or without an antiemetic for acute migraine headaches in adults. Cochrane Database Syst Rev. 2010, Issue 4. Art. No.: CD008041. DOI: 10.1002/14651858.CD008041.pub2.
952. Mosca L, Banka CL, Benjamin EJ et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007; 115:1481-1501. https://pubmed.ncbi.nlm.nih.gov/17309915
953. . Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000; 355:1295-302. https://pubmed.ncbi.nlm.nih.gov/10776741
954. Karthikeyan G, Eikelboom JW, Turpie AG et al. Does acetyl salicylic acid (ASA) have a role in the prevention of venous thromboembolism?. Br J Haematol. 2009; 146:142-9. https://pubmed.ncbi.nlm.nih.gov/19438502
955. AstraZeneca. Brilinta, (ticagrelor) tablets prescribing information. Wilmington, DE; 2011 July.
989. Camm AJ, Lip GY, De Caterina R et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation--developed with the special contribution of the European Heart Rhythm Association. Europace. 2012; 14:1385-413. https://pubmed.ncbi.nlm.nih.gov/22923145
990. Furie KL, Kasner SE, Adams RJ et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011; 42:227-76. https://pubmed.ncbi.nlm.nih.gov/20966421
991. Anderson JL, Adams CD, Antman EM et al. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011; 123:e426-579.
992. Smith SC, Benjamin EJ, Bonow RO et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011; 58:2432-46. https://pubmed.ncbi.nlm.nih.gov/22055990
993. Jneid H, Anderson JL, Wright RS et al. 2012 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction (Updating the 2007 Guideline and Replacing the 2011 Focused Update): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012; 60:645-81. https://pubmed.ncbi.nlm.nih.gov/22809746
994. Levine GN, Bates ER, Blankenship JC et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58:e44-122. https://pubmed.ncbi.nlm.nih.gov/22070834
996. Bonow RO, Carabello BA, Chatterjee K et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008; 118:e523-661.
998. Wann LS, Curtis AB, January CT et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011; 123:104-23. https://pubmed.ncbi.nlm.nih.gov/21173346
999. Fuster V, Rydén LE, Cannom DS et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011; 123:e269-367.
1002. Gould MK, Garcia DA, Wren SM et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e227S-77S. https://pubmed.ncbi.nlm.nih.gov/22315263
1003. Falck-Ytter Y, Francis CW, Johanson NA et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e278S-325S. https://pubmed.ncbi.nlm.nih.gov/22315265
1004. Douketis JD, Spyropoulos AC, Spencer FA et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e326S-50S.
1007. You JJ, Singer DE, Howard PA et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e531S-75S. https://pubmed.ncbi.nlm.nih.gov/22315271
1008. Whitlock RP, Sun JC, Fremes SE et al. Antithrombotic and thrombolytic therapy for valvular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e576S-600S. https://pubmed.ncbi.nlm.nih.gov/22315272
1009. Lansberg MG, O'Donnell MJ, Khatri P et al. Antithrombotic and thrombolytic therapy for ischemic stroke: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e601S-36S. https://pubmed.ncbi.nlm.nih.gov/22315273
1010. Vandvik PO, Lincoff AM, Gore JM et al. Primary and secondary prevention of cardiovascular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e637S-68S.
1011. Alonso-Coello P, Bellmunt S, McGorrian C et al. Antithrombotic therapy in peripheral artery disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e669S-90S. https://pubmed.ncbi.nlm.nih.gov/22315275
1012. Bates SM, Greer IA, Middeldorp S et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e691S-736S. https://pubmed.ncbi.nlm.nih.gov/22315276
1013. Monagle P, Chan AK, Goldenberg NA et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e737S-801S. https://pubmed.ncbi.nlm.nih.gov/22315277
1016. Eikelboom JW, Hirsh J, Spencer FA et al. Antiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e89S-119S.
1017. Bushnell C, McCullough LD, Awad IA et al; on behalf of the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Council for High Blood Pressure Research. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:1545-88. https://pubmed.ncbi.nlm.nih.gov/24503673
1018. Duley L, Henderson-Smart DJ, Meher S et al. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2007; (2):CD004659. https://pubmed.ncbi.nlm.nih.gov/17443552
1019. Food and Drug Administration. FDA drug safety communication: FDA reviews long-term antiplatelet therapy as preliminary trial data shows benefits but a higher risk of non-cardiovascular death. Rockville, MD; 2014 Nov 16. From FDA website. http://www.fda.gov/Drugs/DrugSafety/ucm423079.htm
1020. Mauri L, Kereiakes DJ, Yeh RW et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014; 371:2155-66. https://pubmed.ncbi.nlm.nih.gov/25399658
1021. January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1-76. https://pubmed.ncbi.nlm.nih.gov/24685669
1022. Meschia JF, Bushnell C, Boden-Albala B et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:3754-832. https://pubmed.ncbi.nlm.nih.gov/25355838
1023. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160-236. https://pubmed.ncbi.nlm.nih.gov/24788967
1024. Olesen JB, Torp-Pedersen C, Hansen ML et al. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study. Thromb Haemost. 2012; 107:1172–9. https://pubmed.ncbi.nlm.nih.gov/22473219
1025. . Should direct thrombin inhibitors replace warfarin for prophylaxis of thromboembolism in canadians with atrial fibrillation?. Can J Hosp Pharm. 2012; 65:401-5. https://pubmed.ncbi.nlm.nih.gov/23129871
1026. Miesbach W, Seifried E. New direct oral anticoagulants--current therapeutic options and treatment recommendations for bleeding complications. Thromb Haemost. 2012; 108:625-32. https://pubmed.ncbi.nlm.nih.gov/22782297
1027. . Choice of an oral anticoagulant in atrial fibrillation. Med Lett Drugs Ther. 2012; 54:79-80. https://pubmed.ncbi.nlm.nih.gov/23018987
1028. Potpara TS, Lip GY, Apostolakis S. New anticoagulant treatments to protect against stroke in atrial fibrillation. Heart. 2012; 98:1341-7. https://pubmed.ncbi.nlm.nih.gov/22730480
1029. Granger CB, Armaganijan LV. Newer oral anticoagulants should be used as first-line agents to prevent thromboembolism in patients with atrial fibrillation and risk factors for stroke or thromboembolism. Circulation. 2012; 125:159-64; discussion 164. https://pubmed.ncbi.nlm.nih.gov/22215890
1030. Ansell J. New oral anticoagulants should not be used as first-line agents to prevent thromboembolism in patients with atrial fibrillation. Circulation. 2012; 125:165-70; discussion 170. https://pubmed.ncbi.nlm.nih.gov/22215891
1035. US Food and Drug Administration. FDA Drug Safety Communication: FDA warns about serious bleeding risk with over-the-counter antacid products containing aspirin. Rockville, MD; 2016 Jun 16. From FDA website. Accessed 2016 July 25. http://www.fda.gov/Drugs/DrugSafety/ucm504328.htm
1100. Amsterdam EA, Wenger NK, Brindis RG et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130:e344-426.
1101. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
1102. Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017; 389:197-210. https://pubmed.ncbi.nlm.nih.gov/27502078
1110. Arnett DK, Blumenthal RS, Albert MA et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; https://pubmed.ncbi.nlm.nih.gov/30894318
1111. Meyer J, Arps K, Blumenthal RS et al. New data on aspirin use in the era of more widespread statin use. J Am Coll Cardiol. 2018;
1112. Ridker PM. Should aspirin be used for primary prevention in the post-statin era?. N Engl J Med. 2018; 379:1572-1574. https://pubmed.ncbi.nlm.nih.gov/30332575
1113. McNeil JJ, Wolfe R, Woods RL et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018; 379:1509-1518. https://pubmed.ncbi.nlm.nih.gov/30221597
1114. ASCEND Study Collaborative Group, Bowman L, Mafham M et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018; 379:1529-1539. https://pubmed.ncbi.nlm.nih.gov/30146931
1115. Gaziano JM, Brotons C, Coppolecchia R et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018; 392:1036-1046. https://pubmed.ncbi.nlm.nih.gov/30158069
1116. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2019 . Diabetes Care. 2019; 42:S103-S123. https://pubmed.ncbi.nlm.nih.gov/30559236
1117. Guirguis-Blake JM, Evans CV, Senger CA et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016; 164:804-13.
1118. Gaziano JM, Greenland P. When should aspirin be used for prevention of cardiovascular events? JAMA. Editorial. Published online November 17, 2014. https://jamanetwork.com
1119. Chiang KF, Shah SJ, Stafford RS. A practical approach to low-dose aspirin for primary prevention. JAMA. Editorial. Published online June 28, 2019. https://jamanetwork.com
1200. US Food and Drug Administration. FDA drug safety communication: FDA recommends avoiding use of NSAIDs in pregnancy at 20 weeks or later because they can result in low amniotic fluid. 2020 Oct 15. From the FDA website. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic
1202. Actavis Pharma. Sulindac tablets prescribing information. Parsippany, NJ; 2020 Oct.
a. AHFS drug information 2020. Snow EK, ed. Aspirin. Bethesda, MD: American Society of Health-System Pharmacists; 2020.
h. AHFS drug information 2004. McEvoy GK, ed. Salicylates general statement. Bethesda, MD: American Society of Health-System Pharmacists; 2004:1928-40.
Related/similar drugs
Frequently asked questions
- What's the difference between aspirin and ibuprofen?
- Can You Take Tramadol with Acetaminophen, Ibuprofen, or Aspirin?
- What temperature is considered a fever?
- What cold medicine can you take with diabetes?
- Aspirin Overdose: Symptoms, Diagnosis, Emergency Treatment
- Which painkiller should you use?
- Does aspirin lower blood pressure?
- Can I give Aspirin to my dog or cat?
- Can you take ibuprofen with Excedrin Migraine?
More about aspirin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (53)
- Drug images
- Latest FDA alerts (3)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: platelet aggregation inhibitors
- Breastfeeding