Progesterone
Generic name: progesterone [ proe-JESS-te-rone ]
Brand names: First Progesterone MC10, Menopause Formula Progesterone, Prometrium
Drug class: Progestogens
What is progesterone?
Progesterone is a naturally occurring hormone important for the regulation of ovulation and menstruation. Progesterone is produced in high amounts in females by the ovaries. It is also produced in smaller amounts by the adrenal glands both males and females.
Progesterone is used to cause menstrual periods in women who have not yet reached menopause but are not having periods due to a lack of progesterone in the body. It is also used to prevent overgrowth in the lining of the uterus in postmenopausal women who are receiving estrogen hormone replacement therapy.
Progesterone should not be used to prevent heart disease or dementia, because this medicine may actually increase your risk of developing these conditions.
Warnings
Do not use progesterone without telling your doctor if you are pregnant. It could cause harm to the unborn baby. Use an effective form of birth control, and tell your doctor if you become pregnant during treatment.
You should not use progesterone if you have: abnormal vaginal bleeding, a history of breast cancer, liver disease, or if you have recently had a heart attack, stroke, or blood clot.
Progesterone should not be used to prevent heart disease or dementia, because this medicine may actually increase your risk of developing these conditions.
Using progesterone can increase your risk of blood clots, stroke, heart attack, or breast cancer.
Some forms of this medication may contain peanut oil. Do not use this medicine without telling your doctor if you have a peanut allergy.
Before taking this medicine
You should not use progesterone if you are allergic to it, or if you have:
-
abnormal vaginal bleeding that a doctor has not checked;
-
a history of breast cancer;
-
liver disease;
-
a peanut allergy;
-
if you are pregnant;
-
if you have had a stroke, heart attack, or blood clot within the past year; or
-
if you have recently had an incomplete miscarriage or "missed" abortion.
Using progesterone can increase your risk of blood clots, stroke, heart attack, or breast cancer.
To make sure this medicine is safe for you, tell your doctor if you have:
-
heart disease, circulation problems;
-
migraines;
-
asthma;
-
kidney disease;
-
seizures or epilepsy;
-
a history of depression; or
-
risk factors for coronary artery disease (such as high blood pressure, diabetes, lupus, high cholesterol, family history of coronary artery disease, smoking, being overweight).
Do not use progesterone if you are pregnant. It could harm the unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
Progesterone can pass into breast milk and may harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
How should I use progesterone?
Use progesterone exactly as it was prescribed for you. Follow all directions on your prescription label. Do not use this medicine in larger or smaller amounts or for longer than recommended.
Read all patient information, medication guides, and instruction sheets provided to you. Ask your doctor or pharmacist if you have any questions.
Take the capsule with a full glass of water. It is best to take the medicine at night because this medicine can make you dizzy or drowsy.
Apply progesterone cream to the skin as directed by your doctor.
Progesterone is sometimes used for only a short time, such as 10 to 12 days during each menstrual cycle. Follow your doctor's dosing instructions very carefully.
Have regular physical exams and self-examine your breasts for lumps on a monthly basis while using progesterone.
If you need surgery or medical tests or if you will be on bed rest, you may need to stop using this medicine for a short time. Any doctor or surgeon who treats you should know that you are using this medicine.
Store at room temperature away from moisture, heat, and light.
What happens if I miss a dose?
Use the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not use extra medicine to make up the missed dose.
Call your doctor if you miss more than one dose of this medication.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using progesterone?
Progesterone may impair your thinking or reactions. Be careful if you drive or do anything that requires you to be alert.
Progesterone side effects
Get emergency medical help if you have signs of an allergic reaction to progesterone: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have:
-
unusual vaginal bleeding;
-
pain or burning when you urinate;
-
a breast lump;
-
sudden vision problems, severe headache or pain behind your eyes;
-
symptoms of depression (sleep problems, weakness, mood changes);
-
severe dizziness or drowsiness, spinning sensation, confusion, shortness of breath;
-
heart attack symptoms - chest pain or pressure, pain spreading to your jaw or shoulder, nausea, sweating;
-
liver problems - nausea, upper stomach pain, itching, tired feeling, loss of appetite, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
signs of a stroke - sudden numbness or weakness (especially on one side of the body), sudden severe headache, slurred speech, problems with speech or balance;
-
signs of a blood clot in the lung - chest pain, sudden cough, wheezing, rapid breathing, coughing up blood; or
-
signs of a blood clot in your leg - pain, swelling, warmth, or redness in one or both legs.
Common progesterone side effects may include:
-
drowsiness, dizziness;
-
breast pain;
-
mood changes;
-
headache;
-
constipation, diarrhea, heartburn;
-
bloating, swelling in your hands or feet;
-
joint pain;
-
hot flashes; or
-
vaginal discharge.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect progesterone?
There may be other drugs that can interact with progesterone. Tell your doctor about all medications you use. This includes prescription, over-the-counter, vitamin, and herbal products. Do not start a new medication without telling your doctor.
Popular FAQ
What are my birth control options and how effective are they?
Birth control refers to any behavioral, hormonal, spermicidal, or physical device that is used to prevent pregnancy. Unfortunately for most, human error ("Oops the condom broke", or "I forgot to take my pill") is the reason most forms of birth control (also called contraception) fail; and this has resulted in most manufacturers rating their product's effectiveness on a dual scale: perfect use (PU) and typical use (TU). Continue reading
References
More about progesterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (78)
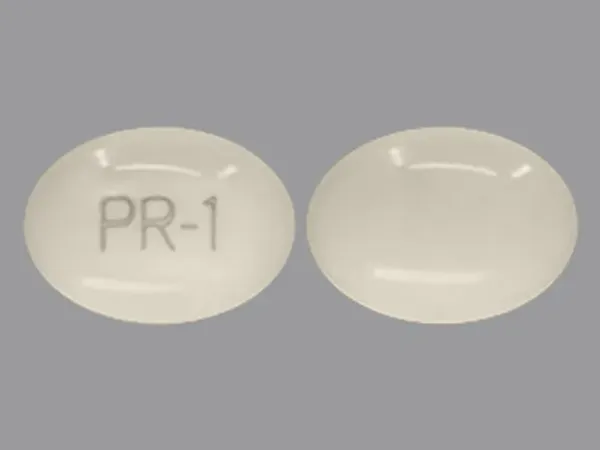
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Progestogens
- Breastfeeding
Patient resources
Other brands
Prometrium, Endometrin, Prochieve
Professional resources
- Progesterone monograph
- Progesterone (Advanced Reading)
- Progesterone (FDA)
- Progesterone Capsule (FDA)
- Progesterone Injection (FDA)
Other brands
Prometrium, Endometrin, Milprosa
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use progesterone only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 11.01.