Progesterone (Monograph)
Brand names: Crinone, Endometrin, Prometrium
Drug class: Progestins
ATC class: G03DA04
VA class: HS800
CAS number: 57-83-0
Introduction
Naturally occurring progestin.
Uses for Progesterone
Amenorrhea
Treatment of secondary amenorrhea.
Assisted Reproductive Technology
Used to support embryo implantation and early pregnancy as part of assisted reproductive technology (ART) treatment of infertile women.
Prevention of Endometrial Changes Associated with Estrogens
Reduction of the incidence of endometrial hyperplasia and the attendant risk of endometrial carcinoma in postmenopausal women receiving estrogen replacement therapy.
Uterine Bleeding
Treatment of abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology such as fibroids or uterine cancer.
Progesterone Dosage and Administration
Administration
Administer orally, parenterally, or intravaginally as a gel or insert.
Oral Administration
Administer once daily at bedtime. Administration at bedtime may alleviate some adverse effects (e.g., dizziness, blurred vision).
If difficulty swallowing the capsule is experienced, administer in an upright position with adequate amounts of fluid (e.g., a glass of water).
IM Administration
Administer by IM injection.
Vaginal Administration
Progesterone vaginal gel (Crinone): Administer intravaginally every other day, every day, or twice daily. Do not administer concurrently with other vaginal preparations. If therapy with another agent administered intravaginally is needed, administer the other agent 6 hours before or after progesterone vaginal gel.
Progesterone vaginal insert (Endometrin): Administer intravaginally 2–3 times daily. Concomitant use with other preparations administered intravaginally is not recommended.
Dosage
Individualize dosage according to the condition being treated and therapeutic response of the patient.
Progesterone 4% vaginal gel (Crinone): Each prefilled applicator delivers approximately 1.125 g of gel (45 mg of progesterone).
Progesterone 8% vaginal gel (Crinone): Each prefilled applicator delivers approximately 1.125 g of gel (90 mg of progesterone).
Progesterone vaginal insert (Endometrin): Appropriate dose for women ≥35 years of age not established.
Adults
Amenorrhea
Oral
400 mg daily for 10 days.
IM
5–10 mg daily for 6–8 consecutive days.
Withdrawal bleeding usually occurs within 48–72 hours after discontinuing therapy. Spontaneous normal cycles may occur in some patients after a single course of therapy.
Vaginal
Progesterone 4% vaginal gel (Crinone): Administer contents of one prefilled applicator every other day for a total of 6 doses.
For patients who do not respond to the 4% gel, administer the contents of one prefilled applicator of progesterone 8% vaginal gel (Crinone) every other day for a total of 6 doses. Women who require the higher dose should receive Crinone 8% vaginal gel; increasing the volume of the 4% gel will not achieve the same progesterone concentrations as the 8% gel.
Assisted Reproductive Technology
Progesterone Supplementation/Replacement
VaginalProgesterone 8% vaginal gel (Crinone): For women who require progesterone supplementation, administer contents of one prefilled applicator once daily. If pregnancy occurs, continue until placenta autonomy is achieved, up to 10–12 weeks.
Progesterone 8% vaginal gel (Crinone): For women who require progesterone replacement, administer contents of one prefilled applicator twice daily. If pregnancy occurs, continue until placenta autonomy is achieved, up to 10–12 weeks.
Progesterone vaginal insert (Endometrin): One insert 2–3 times daily. Start at oocyte retrieval; continue for up to 10 weeks.
Prevention of Endometrial Changes Associated with Estrogens
Oral
200 mg daily for 12 continuous days per 28-day cycle.
Uterine Bleeding
IM
5–10 mg daily for 6 days. When used concomitantly with estrogen therapy, initiate progesterone therapy after 2 weeks of estrogen therapy. Discontinue progesterone if menses occurs during the series of injections.
Cautions for Progesterone
Contraindications
-
Undiagnosed vaginal bleeding.
-
Known or suspected breast or genital cancer; history of breast cancer.
-
Active DVT or pulmonary embolism; history of DVT or pulmonary embolism.
-
Active or recent arterial thromboembolic disease (e.g., stroke, MI), thrombophlebitis, or cerebral apoplexy.
-
Liver disease or dysfunction.
-
Missed abortion or ectopic pregnancy.
-
Use as a pregnancy test.
-
Progesterone capsules are contraindicated in pregnant women and those with suspected pregnancy. Not effective for any purpose during pregnancy.
-
Known hypersensitivity to progesterone or any ingredient in the formulation.
-
Progesterone capsules (Prometrium): Known hypersensitivity to peanuts because the capsules contain peanut oil.
Warnings/Precautions
Warnings
Cardiovascular or Cerebrovascular Disorders
Possible cardiac disorders (MI) or thromboembolic and thrombotic disorders (e.g., thrombophlebitis, pulmonary embolism, cerebrovascular disorders, retinal thrombosis). Observe patients for these effects; discontinue immediately and do not readminister if these disorders occur or are suspected. (See Contraindications under Cautions.)
Progesterone capsules (Prometrium): Syncope and hypotension reported.
Ocular Effects
If unexplained, sudden or gradual, partial or complete loss of vision; proptosis or diplopia; papilledema; migraine; or retinal vascular lesions occur, discontinue and initiate appropriate diagnostic and therapeutic measures. Do not reinitiate therapy if ocular examination reveals evidence of papilledema or retinal vascular lesions.
Sensitivity Reactions
Peanut Hypersensitivity
Progesterone capsules (Prometrium) contain peanut oil. Do not use in patients with peanut allergy. (See Contraindications under Cautions.)
General Precautions
Fluid Retention
May cause some degree of fluid retention. Use with caution and careful monitoring in patients with conditions (e.g., asthma, seizure disorders, migraine headache, cardiac or renal impairment) that might be aggravated by fluid retention.
Bleeding Irregularities
Possible breakthrough or irregular vaginal bleeding. Perform adequate diagnostic tests in patients with undiagnosed vaginal bleeding.
Depression
Possible depression. Exercise caution in women with a history of depression; discontinue if severe depression recurs during use.
Physical Examination and Follow-up
Physical examination prior to initiation of therapy advised. Physical examination should include special attention to the breasts and pelvic organs and should include a Papanicolaou test (Pap smear) and relevant laboratory tests.
Carcinoma of the Breast
Addition of progesterone to estrogen replacement therapy may increase the risk of breast cancer beyond that associated with estrogen use alone.
Metabolic Effects
Possible adverse effects on carbohydrate and lipid metabolism. Monitor patients with hyperlipidemias or diabetes mellitus carefully.
Prolonged Therapy
Effect of long-term therapy on pituitary, ovarian, adrenal, hepatic, or uterine function not determined.
Climacteric
Onset of climacteric may be masked in women.
Estrogen Therapy
When used in combination with an estrogen, consider the cautions, precautions, and contraindications associated with estrogens.
CNS Effects
Progesterone capsules (Prometrium): Transient dizziness reported. Use caution when driving or operating machinery.
Progesterone capsules (Prometrium): Extreme dizziness and/or drowsiness, blurred vision, slurred speech, difficulty walking, loss of consciousness, vertigo, confusion, disorientation, and shortness of breath reported; women who experience these adverse effects should consult their healthcare provider.
Specific Populations
Pregnancy
Used to support embryo implantation and maintain pregnancy as a component of ART treatment in infertile women. Such use is associated with increased ongoing pregnancy rates.
Progesterone capsules (Prometrium): Category B.
Lactation
Progestins are distributed into milk. Caution advised.
Pediatric Use
Safety and efficacy not established. Not indicated in pediatric patients.
Adult Use
Vaginal inserts (Endometrin): Efficacy not established in women ≥35 years of age.
Geriatric Use
Progesterone injection, vaginal inserts, and gel: Safety and efficacy not established in patients >65 years of age.
Progesterone capsules (Prometrium): Insufficient experience in those ≥65 years of age to determine whether they respond differently than younger adults. Select dose with caution; start at the lower end of the dosing range due to the greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy.
Hepatic Impairment
Contraindicated in patients with liver dysfunction or disease.
Progesterone capsules (Prometrium): If indicated in patients with mild to moderate hepatic dysfunction, monitor patient closely.
Renal Impairment
Progesterone injection and capsules: Safety and efficacy not established in patients with renal impairment. Use with caution; carefully monitor patients with renal impairment.
Common Adverse Effects
Menstrual abnormalities (amenorrhea; breakthrough bleeding and/or spotting; changes in menstrual flow), weight changes, dizziness, headache, abdominal pain and/or distention, breast tenderness and/or pain, fatigue, musculoskeletal pain, joint pain.
Injection site pain.
Drug Interactions
Drugs Affecting Hepatic Microsomal Enzymes
Pharmacokinetic interaction possible with drugs that are inhibitors of CYP3A4.
Vaginal Preparations
Progesterone vaginal gel (Crinone): Do not administer concurrently with other vaginal preparations. If therapy with another agent administered intravaginally is needed, administer the other agent 6 hours before or after progesterone vaginal gel.
Progesterone vaginal insert (Endometrin): Concomitant administration with another vaginal preparation may alter release and absorption of progesterone. Concomitant use with other preparations administered intravaginally is not recommended.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Conjugated estrogens |
Progesterone capsules: Decreased estradiol AUC, increased estrone and equilin AUCs |
Progesterone Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract; peak plasma concentrations achieved within 3 hours.
Peak plasma concentrations attained in 8–9 hours following IM administration.
Peak plasma concentrations attained in 5–7 hours following administration of progesterone vaginal gel. Absorption is prolonged due to sustained-release properties of this preparation.
Peak plasma concentrations reached in 17–24 hours following administration of progesterone vaginal insert.
Food
Food increases bioavailability of progesterone capsules.
Distribution
Extent
Distributed into human milk.
Plasma Protein Binding
96–99% (mainly albumin).
Elimination
Metabolism
Metabolized in the liver to pregnanediols and pregnanolones, followed by glucuronide and sulfate conjugation. Further metabolism may occur in the GI tract.
Elimination Route
Excreted in urine and bile, mainly as metabolites.
Following administration of progesterone injection, 50-60% of metabolites are excreted by the kidneys, while approximately 10% are excreted by the bile and feces. A small portion is excreted in the bile unchanged.
Half-life
IM doses: 20–30 hours.
Vaginal gel: 30–60 hours.
Stability
Storage
Oral
Capsules
Tight, light-resistant containers at 25°C (may be exposed to 15–30°C).
Parenteral
Injection
15–30°C.
Vaginal
Gel and Inserts
25°C (may be exposed to 15–30°C).
Actions
-
Formed from steroid precursors in the ovary, testis, adrenal cortex, and placenta; secreted mainly from the corpus luteum of the ovary during the latter half of the menstrual cycle.
-
Required for implantation of the ovum and for maintenance of pregnancy.
-
Transforms a proliferative endometrium into a secretory one.
-
Stimulates growth of mammary alveolar tissue and relaxes uterine smooth muscle.
-
Minimal estrogenic and androgenic activity.
Advice to Patients
-
Importance of reading the manufacturer's patient information.
-
Importance of advising patients of anticipated menstrual effects.
-
Progesterone capsules (Prometrium): Importance of using caution when driving or operating machinery, especially during the initiation of therapy.
-
Progesterone vaginal gel (Crinone): Importance of following special instructions if the gel is used at altitudes >2500 feet.
-
Importance of discontinuing therapy and contacting clinician if sudden partial or complete vision loss, blurred vision, bulging of the eyes, double vision, or migraine occur.
-
Importance of discontinuing therapy and contacting clinician if any symptoms of thromboembolic and thrombotic disorders occurs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.
-
Advise women using the vaginal gel or insert not to use other vaginal preparations. If therapy with another agent administered intravaginally is needed in a women using the gel, administer the other agent 6 hours before or after progesterone vaginal gel.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder |
|||
|
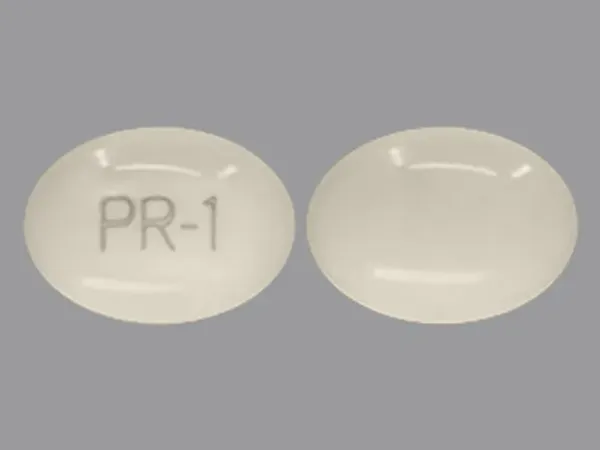
Oral |
Capsules |
100 mg |
Prometrium (with peanut oil) |
Abbott |
|
200 mg |
Prometrium (with peanut oil) |
Abbott |
||
|
Parenteral |
Injection |
50 mg/mL* |
Progesterone Injection (with benzyl alcohol 10% and sesame oil) |
|
|
Vaginal |
Gel |
4% |
Crinone (available in prefilled, disposable applicators) |
Watson |
|
8% |
Crinone (available in prefilled, disposable applicators) |
Watson |
||
|
Insert |
100 mg |
Endometrin (with disposable applicators) |
Ferring |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 2, 2012. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about progesterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (78)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Progestogens
- Breastfeeding
Patient resources
Professional resources
- Progesterone product monographs
- Progesterone (FDA)
- Progesterone Capsule (FDA)
- Progesterone Injection (FDA)
Other brands
Prometrium, Endometrin, Milprosa