Progesterone
Medically reviewed by Drugs.com. Last updated on Jan 22, 2025.
Clinical Overview
Use
Topical progesterone is used to manage menopause-related symptoms, such as hot flashes, low libido, and mood swings. Clear evidence of a progesterone benefit in management of cyclic breast pain, for improving bone density or cardiovascular markers, and in preventing endometrial proliferation is lacking. Topical progesterone has also been used to increase skin elasticity and firmness in peri- and postmenopausal females. However, quality clinical trial data are lacking to recommend use.
Dosing
Most trials evaluated topically applied progesterone 40 mg daily either as a single dose or 20 mg twice daily for treatment of menopausal symptoms; duration of treatment varied (range, 3 months to 3 years).
Contraindications
Contraindications have not been identified.
Pregnancy/Lactation
Information regarding safety and efficacy of topically applied progesterone in pregnancy and lactation is lacking.
Interactions
None well documented.
Adverse Reactions
Clinical trials report few adverse events, with most no different from those of the placebo comparator. A higher incidence of headache and postmenopausal bleeding has been reported.
Toxicology
No data.
Source
Progesterone, a principle of corpus luteum, is the primary endogenous progestational substance. Progestins (progesterone and derivatives) transform proliferative endometrium into secretory endometrium. Progesterone is necessary to increase endometrial receptivity for implantation of an embryo.(Teh 2016)
Progesterone receptors have been identified in whole skin, keratinocytes, and fibroblasts.(Elshafie 2007)
Phytoestrogens, structurally similar to human estrogen and progesterone, are synthesized by more than 5,000 plants. Progesterone can be converted from the sterol diosgenin found in plants such as soybeans and wild yam.(Elshafie 2007) This monograph is limited to evidence for progesterone cream and does not include references to wild yam or soy. (See Wild Yam or Soy monographs for more information.) Despite claims that natural progesterone is plant-based and therefore from a natural source, many synthesized progesterones are also plant-derived and are chemically identical to progesterone of the ovarian origin.(Natural progesterone 2001)
History
"Natural" progesterone cream has been available in the United States for at least 20 years as an over-the-counter preparation and is not regulated by the US Food and Drug Administration.(Elshafie 2007, Hermann 2005, Lee 1998) Transdermal delivery was proposed as an alternative to the oral route because approximately 90% of progesterone is enzymatically inactivated in the gut and liver and results in production of undesirable metabolites.(Elshafie 2007)
Claims for the use of topical natural progesterone include the prevention and treatment of osteoporosis and low libido, as well as the management of menopausal symptoms, including hot flashes and enhancement of mood and psychological well-being.(Elshafie 2007, Hermann 2005)
Chemistry
Progesterone is a 20-oxo steroid, a 3-oxo-Delta(4) steroid, and a C21-steroid hormone that derives from a hydride of a pregnane; a pregnane skeleton carries oxo substituents at positions 3 and 20 and is unsaturated at C(4) to C(5). The molecular formula of progesterone is C21H30O2, and the molecular weight is 314.5.(NLM 2004)
Uses and Pharmacology
Clinical studies have been conducted to describe the pharmacokinetics of topical progesterone, with most studies finding major increases in salivary progesterone and only moderate increases in serum progesterone levels. Wide variations in measured progesterone levels are also a feature of these studies.(Carey 2000, Elshafie 2007, Gambrell 2003, Lewis 2002, O'Leary 2000, Wren 2003) In a crossover study, topical progesterone 40 mg twice daily showed no difference compared with oral progesterone 200 mg in 24-hour AUC for whole blood progesterone,(Hermann 2005) while another kinetic study using a daily progesterone 60 mg cream achieved serum progesterone levels similar to luteal levels (greater than 3 ng/mL).(Burry 1999) In a clinical trial evaluating the effect of progesterone on bone density, increased serum progesterone for up to 6 months was observed, with no further accumulation; at 3 years, mean serum progesterone level was 3.54 nmol/L.(Benster 2009a)
Various mechanisms have been proposed to explain the observed low plasma levels of progesterone following topical application. These include uptake by red blood cells, rapid conversion to 5-alpha-reduced progestin, and rapid clearance from the serum by salivary and hepatic excretion, combined with slow transdermal absorption.(Carey 2000, Elshafie 2007, Lewis 2002) A "priming" effect of the skin resulting in increased absorption after a few days of administration has also been suggested.(Carey 2000, Holzer 2005)
In a study investigating transdermal uptake and tissue distribution of progesterone cream in a rat model, topical progesterone was found to be effectively and biologically actively absorbed. Patterns of distribution in tissues and metabolism were similar to those following intravascular administration.(Waddell 2002)
Genital lichen sclerosus
Clinical data
A systematic review and meta-analysis of randomized controlled trials that investigated use of topical interventions for genital lichen sclerosus found no evidence to support the use of topical progesterone as a treatment option. Of the 7 studies that met inclusion criteria, only 1 evaluated topical progesterone (2% cream) and showed no significant difference compared with placebo after 3 months of application.(Chi 2012)
Mastalgia
Clinical data
Topical natural progesterone was no better than placebo for the management of cyclic breast pain in a small clinical trial.(McFadyen 1989)
Menopause/Menopausal symptoms
Clinical data
Debate exists regarding relevance of plasma and salivary progesterone as surrogate indicators of clinical efficacy in menopausal-related symptoms.(Elshafie 2007, Lee 1998, Lewis 2002, O'Leary 2000) Clear evidence of a progesterone benefit in improving bone density or cardiovascular markers, or in preventing endometrial proliferation is lacking.(Cooper 1998, Gambrell 2003, Leonetti 2003, Scant evidence 1999, Stevenson 1998)
In an open-label study, topical progesterone 40 mg daily applied for more than 1 year did not provide adequate opposition to endometrial hyperplasia as determined by endometrial histology and bleeding patterns in 41 postmenopausal females.(Vashisht 2005a, Vashisht 2005b) In a small clinical crossover trial (N=26), topical progesterone 40 mg daily exerted a similar effect on the endometrium as standard oral progesterone.(Leonetti 2005) In a large, double-blind, randomized trial (N=223), topical progesterone (Progestelle) applied for more than 6 months showed no difference compared with placebo for psychological, somatic, or vasomotor menopause-related symptoms. Dosages of progesterone 5 mg, 20 mg, 40 mg, and 60 mg daily were tested. A string placebo effect was observed. No histological effect of topical progesterone on the endometrium was demonstrated.(Benster 2009b)
In a randomized clinical study, results with topical progesterone 32 mg daily for 3 months did not differ from those with placebo for vasomotor symptoms, mood, or libido, and results showed no effect on blood lipids or bone metabolic markers.(Wren 2003)
In a randomized clinical trial in postmenopausal females (N=102), topical progesterone 20 mg daily showed no protective effect on bone density at 1 year and no change in lipid profile versus placebo. However, an improvement in vasomotor symptoms was recorded.(Leonetti 1999) A 2-year study evaluating the effect of soy and transdermal progesterone on bone mineral density in postmenopausal females found progesterone alone to have protective effects on the lumbar spine but not hip bone; however, the positive effect was attenuated when used in combination with soy milk.(Lydeking-Olsen 2004) No effect on bone density or plasma lipids was found for topical progesterone 40 mg daily in a large, double-blind, randomized, 3-year clinical trial (N=131) of postmenopausal females.(Benster 2009a)
A progesterone 2% cream applied nightly for 16 weeks increased the elasticity and firmness of skin in peri- and postmenopausal females in a small study (N=40).(Holzer 2005)
Dosing
Commercial progesterone creams vary in concentration but are generally in the range of 1.5% to 3% progesterone.
Most trials evaluated topically applied progesterone 40 mg daily either as a single dose or 20 mg twice daily for treatment of menopausal symptoms; duration of treatment varied (range, 3 months to 3 years).(Benster 2009a, Benster 2009b, Vashisht 2005a, Vashisht 2005b)
Pregnancy / Lactation
Information regarding safety and efficacy of topically applied progesterone in pregnancy and lactation is lacking.
Interactions
Interactions have primarily occurred with progesterone prescription products.
Antidiabetic agents: Hyperglycemia-associated agents may diminish the therapeutic effect of antidiabetic agents. Monitor therapy.(Accretropin January 2008, Amaryl October 2013, Diuril June 2009, Niaspan February 2013, Novolog January 2015, Reyataz June 2014, Symlin June 2014, Torisel February 2015)
Antifungal agents (vaginal): Antifungal agents (vaginal) may diminish the therapeutic effect of progesterone. This interaction only applies to vaginal progesterone products and vaginal antifungal products. Avoid combination.(Endometrin February 2008, Endometrin May 2015, Milprosa April 2020)
Metyrapone: Progestins may diminish the diagnostic effect of metyrapone. Consider therapy modification.(Meikle 1969, Meikle 1970, Metopirone September 2022, Papaleo 1984, Plonk 1976, Sprunt 1968, Werk 1967)
Sincalide: Drugs that affect gallbladder function may diminish the therapeutic effect of sincalide. Consider therapy modification.(Kinevac December 2018)
Ulipristal: Ulipristal may diminish the therapeutic effect of progestins. Progestins may diminish the therapeutic effect of ulipristal. Avoid combination.(Brache 2015, ella June 2021)
Adverse Reactions
Clinical trials report few adverse events, with most no different from those of the placebo comparator.(Benster 2009a, Burry 1999) A higher incidence of headache and postmenopausal bleeding was associated with topical progesterone in one large clinical study.(Benster 2009b) Water retention, breast engorgement, increased body weight, and mild to moderate depression have been documented in case reports following long-term use.(Ilyia 1998)
While progesterone may be beneficial in females with proven low progesterone levels, or those experiencing symptoms due to relative progesterone deficits (more or less normal progesterone levels but with estrogen excess), progesterone may increase the hormonal load in the body. Aromatase enzymes in adipose cells below the dermis convert androgens, including progesterone, into estrogen. Therefore, females with hyperestrogenism may not benefit and may even be harmed by progesterone supplementation if it is not prescribed appropriately.(Pasqualini 2009, Reed 1994)
Related/similar drugs
Toxicology
Research reveals no information regarding toxicity of topical progesterone.
References
Disclaimer
This information relates to an herbal, vitamin, mineral or other dietary supplement. This product has not been reviewed by the FDA to determine whether it is safe or effective and is not subject to the quality standards and safety information collection standards that are applicable to most prescription drugs. This information should not be used to decide whether or not to take this product. This information does not endorse this product as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this product. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this product. This information is not specific medical advice and does not replace information you receive from your health care provider. You should talk with your health care provider for complete information about the risks and benefits of using this product.
This product may adversely interact with certain health and medical conditions, other prescription and over-the-counter drugs, foods, or other dietary supplements. This product may be unsafe when used before surgery or other medical procedures. It is important to fully inform your doctor about the herbal, vitamins, mineral or any other supplements you are taking before any kind of surgery or medical procedure. With the exception of certain products that are generally recognized as safe in normal quantities, including use of folic acid and prenatal vitamins during pregnancy, this product has not been sufficiently studied to determine whether it is safe to use during pregnancy or nursing or by persons younger than 2 years of age.
Frequently asked questions
More about progesterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (78)
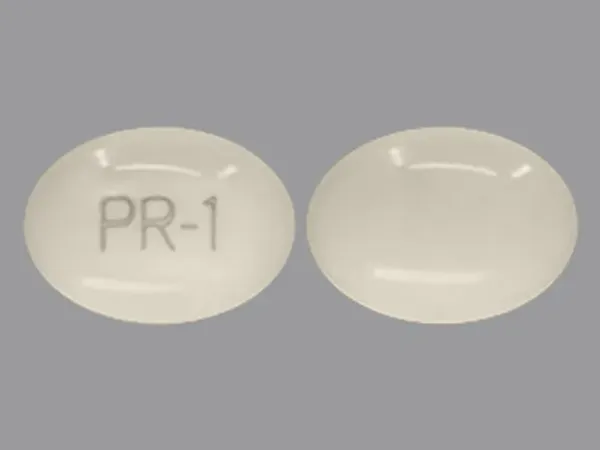
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Progestogens
- Breastfeeding
Patient resources
Professional resources
Other brands
Prometrium, Endometrin, Milprosa
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright © 2025 Wolters Kluwer Health