The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Albuterol (Monograph)
Brand names: AccuNeb, ProAir HFA, Proventil, Proventil HFA, Ventolin HFA,
... show all 8 brands
Drug class: Selective beta-2-Adrenergic Agonists
VA class: RE102
CAS number: 18559-94-9
Introduction
Bronchodilator; relatively selective, short-acting β2-adrenergic agonist.
Uses for Albuterol
Bronchospasm in Asthma
Symptomatic management or prevention of bronchospasm in patients with reversible, obstructive airway disease (e.g., asthma).
Exercise-induced Bronchospasm
Prevention of exercise-induced bronchospasm.
Chronic Obstructive Pulmonary Disease
Albuterol sulfate in fixed combination with ipratropium bromide: Symptomatic management of reversible bronchospasm associated with COPD in patients who continue to have evidence of bronchospasm despite regular use of an orally inhaled bronchodilator and who require a second bronchodilator.
Albuterol sulfate: Symptomatic management of reversible bronchospasm associated with COPD† [off-label] when given on an as-needed or regular (e.g., 4 times daily) basis, either alone or concomitantly with other inhaled bronchodilators. Regular use of a selective, short-acting inhaled β2-adrenergic agonist (e.g., albuterol) in the management of COPD, in contrast to that in asthma, does not appear to be detrimental.
Albuterol Dosage and Administration
General
-
Albuterol sulfate: Administer by oral inhalation via metered-dose inhaler or nebulizer or orally.
-
Albuterol sulfate in fixed combination with ipratropium bromide: Administer by oral inhalation via metered-dose aerosol inhaler or nebulizer.
-
Adjust dosage carefully according to individual requirements and response.
Administration
Oral Inhalation
Metered-dose Aerosol Inhaler
Administer inhalation aerosol only with the actuator provided by the manufacturer.
Shake inhaler well before use.
Test-spray inhalation aerosol (3 times for ProAir HFA, 4 times for Ventolin HFA or Proventil HFA) into the air (away from the face) before first use and whenever the inhaler not used for prolonged periods (i.e., >2 weeks). Test spray Ventolin HFA aerosol inhaler whenever dropped.
Avoid spraying aerosols into the eyes.
Exhale slowly and completely and place the mouthpiece of the inhaler well into the mouth with the lips closed around it. Inhale slowly and deeply through the mouth. Actuate aerosol inhaler, hold breath for as long as possible, withdraw mouthpiece, and exhale slowly.
Allow 1 minute to elapse between subsequent inhalations from aerosol inhaler.
Clean the albuterol sulfate inhalation aerosol (ProAir HFA, Proventil HFA, Ventolin HFA) inhaler by removing the metal canister and running warm water through the plastic mouthpiece of the actuator for 30 seconds at least once a week. Dry thoroughly the mouthpiece before replacing the metal canister and mouthpiece cap. If the inhaler is to be used before it is completely dry, shake off excess water, replace the canister, and test the inhaler by spraying once (Ventolin HFA) or twice (ProAir HFA, Proventil HFA) away from the face before administering the dose. After such use, rewash the mouthpiece and allow to air dry. Proper cleaning of the albuterol sulfate inhaler (ProAir HFA, Proventil HFA, Ventolin HFA) mouthpiece will prevent medication build-up and blockage.
Discard canister after the labeled number of actuations used.
Nebulization
When administering via nebulization, use proper aseptic technique to avoid microbial contamination.
For administration of albuterol sulfate solution for nebulization in single-use units, empty the entire contents of a single-use unit into the nebulizer reservoir and use immediately to avoid microbial contamination. For administration of single-use units of albuterol sulfate 0.5% concentrate solution for nebulization, empty the entire contents of the plastic vial into the nebulizer reservoir and add 2.5 mL of 0.9% sodium chloride solution into the nebulizer reservoir to provide a final volume of 3 mL.
Attach the reservoir to the mouthpiece or face mask and to the compressor according to the manufacturer’s instructions.
Place the mouthpiece of the nebulizer in the mouth or put on the nebulizer face mask and turn on the compressor. Breathe as calmly, deeply, and evenly as possible until the nebulizer stops producing mist (flow rate of nebulizer should be adjusted to provide the full dose over about 5–15 minutes).
Clean the nebulizer after use according to the manufacturer’s instructions.
Continue nebulization therapy as necessary to control recurrent bronchospasm. Optimum benefit is obtained when nebulization is used regularly.
Oral Administration
Albuterol sulfate extended-release tablets should not be chewed or crushed.
Dosage
Available as albuterol sulfate; dosage expressed in terms of albuterol.
Pediatric Patients
Bronchospasm in Asthma
Oral Inhalation Aerosol
Children ≥4 years of age: 180 mcg (2 inhalations) every 4–6 hours (ProAir HFA, Proventil HFA, Ventolin HFA). Do not increase dosage or dosage frequency. Alternatively, 90 mcg (1 inhalation) every 4 hours may be sufficient.
Oral Nebulization Solution
0.042% Inhalation solution for nebulization in children 2–12 years of age: 0.63 or 1.25 mg 3 or 4 times daily. Dosage of 1.25 mg 3 or 4 times daily may improve initial response in children 6–12 years of age with more severe asthma (baseline FEV1 <60% of predicted), patients weighing >40 kg, or children 11–12 years of age. For acute exacerbations, a 0.083% solution containing 2.5 mg of albuterol per 3 mL may be more appropriate, particularly in children ≥6 years of age.
0.083% Inhalation solution for nebulization in children 2–12 years of age: 2.5 mg 3 or 4 times daily in children weighing ≥15 kg. Do not increase dosage or dosage frequency. In children 2–12 years of age weighing<15 kg who require <2.5 mg per dose, the 0.5% inhalation solution should be used to prepare the appropriate dose for nebulization.
0.083% Inhalation solution for nebulization in adolescents ≥12 years of age: 2.5 mg 3 or 4 times daily (Proventil single-use inhalation solution).
0.5% Inhalation solution for nebulization in adolescents ≥12 years of age: 2.5 mg 3–4 times daily.
Oral Conventional Tablets
Children 6–12 years of age: Initially, 2 mg 3 or 4 times daily. If necessary, increase dosage cautiously and gradually as tolerated to a maximum of 6 mg 4 times daily (maximum 24 mg total daily dosage).
Adolescents ≥12 years of age: Initially, 2 or 4 mg 3 or 4 times daily. If necessary, increase dosage cautiously and gradually as tolerated to a maximum of 8 mg 4 times daily (maximum 32 mg total daily dosage).
Oral Extended-release Tablets
Children 6–12 years of age: Initially, 4 mg every 12 hours (VoSpire ER). If necessary, increase dosage cautiously and gradually as tolerated to a maximum of 12 mg twice daily (maximum 24 mg total daily dosage).
Adolescents ≥12 years of age: Initially, 8 mg every 12 hours. In some patients, 4 mg every 12 hours may be sufficient (e.g., low body weight). If necessary, increase dosage cautiously and gradually as tolerated to a maximum of 16 mg twice daily (maximum 32 mg total daily dosage). When transferring from conventional tablets to extended-release tablets, each 2 mg administered every 6 hours as conventional tablets is approximately equivalent to 4 mg every 12 hours as extended-release tablets.
Oral Solution
Children 2–6 years of age: Initially, 0.1 mg/kg (up to 2 mg) 3 times daily. If necessary, increase dosage cautiously and gradually as tolerated to 0.2 mg/kg (up to 4 mg) 3 times daily (maximum 12 mg total daily dosage).
Children or adolescents >6–14 years of age: Initially, 2 mg 3 or 4 times daily. If necessary increase dosage cautiously and gradually as tolerated to a maximum of 24 mg daily in divided doses.
Adolescents >14 years of age: 2 or 4 mg 3–4 times daily. If necessary, increase dosage cautiously and gradually to a maximum of 8 mg 4 times daily.
Prevention of Exercise-induced Bronchospasm
Oral Inhalation Aerosol
Children ≥4 years of age: 180 mcg (2 inhalations) administered 15–30 minutes before exercise via metered-dose inhaler (ProAir HFA, Proventil HFA, Ventolin HFA).
Adults
Bronchospasm in Asthma
Oral Inhalation Aerosol
180 mcg (2 inhalations) every 4–6 hours. Do not increase dosage or dosage frequency of orally inhaled albuterol aerosol. Alternatively, 90 mcg (1 inhalation) every 4 hours.
Oral Nebulization Solution
2.5 mg 3 or 4 times daily. Do not increase dosage or dosage frequency.
Oral Conventional Tablets or Solution
Initially, 2 or 4 mg 3 or 4 times daily. If necessary, increase dosage cautiously and gradually as tolerated to a maximum of 8 mg 4 times daily.
Oral Extended-release Tablets
Initially, 4 or 8 mg every 12 hours. In some patients (e.g., low body weight), 4 mg every 12 hours may be sufficient. If necessary, increase dosage cautiously and gradually as tolerated to maximum of 16 mg twice daily.
Prevention of Exercise-induced Bronchospasm
Oral Inhalation Aerosol
180 mcg (2 inhalations) administered 15–30 minutes before exercise via the metered-dose inhaler (ProAir HFA, Proventil HFA, Ventolin HFA).
Chronic Obstructive Pulmonary Disease
Oral Inhalation Aerosol
Initially, 180 mcg (2 inhalations) 4 times daily in fixed combination with ipratropium bromide (18 mcg per inhalation). If necessary, additional inhalations may be used, with dosage not >12 inhalations in 24 hours.
Oral Nebulization Solution
Initially, 2.5 mg 4 times daily in fixed combination with ipratropium bromide (0.5 mg per dose) (DuoNeb). If necessary, may administer 2.5 mg in fixed combination with ipratropium bromide (0.5 mg per dose) up to 6 times daily.
Prescribing Limits
Pediatric Patients
Bronchospasm in Asthma
Oral Nebulization Solution
Children 2–12 years of age: Maximum 2.5 mg 4 times daily in children weighing at least 15 kg.
Adolescents ≥12 years of age: Maximum 2.5 mg 4 times daily.
Oral Conventional Tablets
Children 6–12 years of age: Maximum 24 mg daily (in divided doses).
Adolescents ≥12 years of age: Maximum 8 mg 4 times daily.
Oral Extended-release Tablets
Children 6–12 years of age: Maximum 12 mg twice daily.
Adolescents >12 years of age: Maximum 16 mg twice daily.
Oral Solution
Children 2–6 years of age: Maximum 4 mg 3 times daily.
Children or adolescents >6 to 14 years of age: Maximum 24 mg daily in divided doses.
Adolescents >14 years of age: Maximum 8 mg 4 times daily.
Adults
Bronchospasm in Asthma
Oral Nebulization Solution
Maximum 2.5 mg 4 times daily.
Oral Conventional Tablets or Solution
Maximum 8 mg 4 times daily.
Oral Extended-release Tablets
Maximum 16 mg twice daily.
Chronic Obstructive Pulmonary Disease
Oral Inhalation Aerosol
Maximum 180 mcg (2 inhalations) 4 times daily in fixed combination with ipratropium bromide (18 mcg per inhalation).
Oral Nebulization Solution
Maximum 2.5 mg 6 times daily in fixed combination with ipratropium bromide (0.5 mg per dose).
Special Populations
Geriatric Patients
Oral Conventional Tablets or Solution
Initially, 2 mg 3 or 4 times daily. May increase gradually as tolerated up to a maximum of 8 mg 3 or 4 times daily (conventional tablets).
Oral Inhalation Aerosol
Initiate therapy with dosages at the lower end of the usual range.
Patients Sensitive to Sympathomimetic Amines
Oral Conventional Tablets or Solution
Initially, 2 mg 3 or 4 times daily. May increase gradually as tolerated up to 8 mg 3 or 4 times daily.
Cautions for Albuterol
Contraindications
-
Known hypersensitivity to albuterol or any ingredients in the formulations.
-
Known history of hypersensitivity to soya lecithin or related food products such as soybeans or peanuts; atropine and its derivatives; or any other ingredient in the specific formulation (albuterol sulfate in fixed combination with ipratropium bromide).
Warnings/Precautions
Warnings
Acute or Worsening Asthma
Oral inhalation therapy is intended for the acute symptomatic relief of bronchospasm. If control of mild asthma deteriorates such that regular (i.e., exceeding 4 times daily) use of a short-acting β2-agonist becomes necessary, institute maintenance therapy (e.g., inhaled corticosteroids) and discontinue regular use of short-acting β2-agonists in such patients; instead, use short-acting β2-agonists only as a supplement for relief of acute asthma symptoms. Contact a clinician for reevaluation if control of mild asthma deteriorates.
Failure to respond to a previously effective dosage of albuterol may indicate seriously worsening asthma. Reevaluate asthma therapy and institute alternative regimens or therapy. Discontinue and contact a clinician if decreased effectiveness occurs; do not increase the dose or frequency of administration.
Excessive Doses
Possible fatalities associated with excessive use of inhaled sympathomimetic drugs. The safety of concomitant use of >8 inhalations per day of a short-acting β2-adrenergic agonist with a long-acting β2-agonist (e.g., salmeterol) oral inhalation therapy has not been established. (See Sympathomimetic Agents under Interactions.)
Paradoxical Bronchospasm
Possible life-threatening, acute paradoxical bronchospasm. Frequently occurs with the first use of a new canister or vial (oral inhalation aerosol), but also may occur with orally administered conventional or extended-release tablets.
Discontinue therapy immediately if bronchoconstriction occurs and institute alternative therapy.
Cardiovascular Effects
Possible clinically important cardiovascular effects, including cardiac arrhythmias (e.g., atrial fibrillation, supraventricular tachycardia, extrasystoles) , increased or decreased BP, and related symptoms.
Cautious use recommended in patients with cardiovascular disorders (e.g., coronary insufficiency, cardiac arrhythmias), hypertension, and those with sensitivity to sympathomimetic amines. May require drug discontinuance.
Sensitivity Reactions
Immediate hypersensitivity reactions (e.g., urticaria, angioedema, rash, bronchospasm, anaphylaxis, oropharyngeal edema) have been reported. Possible acute bronchospasm. (See Paradoxical Bronchospasm under Cautions.)
General Precautions
Nervous System Effects
Possible CNS stimulation and adverse nervous system effects.
Cautious use recommended in patients with seizure disorders and in those with sensitivity to sympathomimetic amines.
Metabolic Effects
Possible hypokalemia, which may increase risk of adverse cardiovascular effects. (See Cardiovascular Effects under Cautions.) Serum potassium decrease generally is transient and usually does not require supplementation.
Diabetes mellitus or increased blood glucose in patients receiving orally inhaled or nebulized albuterol.
Cautious use recommended in patients with diabetes mellitus or hyperthyroidism.
GI Effects
Possible GI obstruction when extended-release tablets are used in patients with preexisting GI narrowing; cautious use recommended.
Use of Fixed Combination
When used in fixed combination with other agents, consider the cautions, precautions, and contraindications associated with the concomitant agents.
Specific Populations
Pregnancy
Category C.
Lactation
Not known whether albuterol is distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of orally inhaled albuterol sulfate inhalation aerosols (ProAir HFA, Proventil HFA, Ventolin HFA) not established in children <4 years of age. Safety and efficacy of orally inhaled racemic albuterol sulfate inhalation solution (Proventil) not established in children <12 years of age. Safety and efficacy of some albuterol inhalation solutions for nebulization (e.g., AccuNeb, albuterol sulfate 0.083%) not established in children <2 years of age. Safety and efficacy of albuterol sulfate in fixed combination with ipratropium bromide not established in pediatric patients <18 years of age.
Safety and efficacy of albuterol conventional and extended-release tablets not established in children <6 years of age. Safety and efficacy of albuterol sulfate oral solutions not established in children younger <2 years of age.
Geriatric Use
No overall differences in safety and efficacy observed between geriatric and younger patients for albuterol sulfate in fixed combination with ipratropium bromide inhalation solution.
Special caution should be used in geriatric patients who have cardiovascular disease. (See Cautions: Cardiovascular Effects.) Cannot rule out possibility that some geriatric patients may exhibit increased sensitivity to the drug.
Substantially eliminated by kidneys; assess renal function periodically since geriatric patients more likely to have decreased renal function. Risk of toxicity greater in patients with renal impairment, including geriatric patients.
Common Adverse Effects
Albuterol sulfate: Tremor, asthma exacerbation, bronchospasm, nervousness, shakiness, otitis media, nausea, cough, bronchitis, headache, tachycardia/palpitations, muscle cramps, hypokinesia, insomnia, weakness, dizziness, excitement, hyperactivity, increased appetite, flu syndrome, lymphadenopathy, skin/appendage infection, urticaria.
Albuterol sulfate in fixed combination with ipratropium bromide: Bronchitis, upper respiratory tract infection, lung disease, headache, dyspnea, pharyngitis, coughing, chest pain, pain, respiratory disorder, sinusitis, nausea, diarrhea, urinary tract infection, influenza, pneumonia, leg cramps, dyspepsia, constipation, voice alterations, bronchospasm.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β-Adrenergic blocking agents |
Antagonism of pulmonary effects resulting in severe bronchospasm in asthmatic patients |
If concomitant therapy required, consider cautious use of cardioselective β-adrenergic blocking agents |
|
Digoxin |
Decreased serum digoxin concentrations |
Careful evaluation of serum digoxin concentrations recommended |
|
Diuretics, nonpotassium-sparing |
Decreased serum potassium concentrations and/or ECG changes, especially when the recommended β-agonist dose is exceeded |
Cautious use recommended |
|
MAO inhibitors |
Increased effect on vascular system |
Extreme caution recommended with concomitant therapy or in patients receiving albuterol within 2 weeks of discontinuance of these agents |
|
Sympathomimetic agents (e.g., epinephrine) |
Increased cardiovascular adverse effects |
Avoid concomitant use of inhaled albuterol and other short-acting inhaled sympathomimetic amine bronchodilators or oral albuterol and other oral sympathomimetic agents Concomitant oral albuterol and inhaled sympathomimetic agent may be used on individualized basis If such concomitant use regularly required, consider alternative therapy |
Albuterol Pharmacokinetics
Absorption
Single-dose oral bioavailability of extended-release albuterol sulfate tablets is about 80% that of conventional tablets.
Efficacy of orally inhaled drug appears to result from local action rather than systemic absorption. Drug plasma concentrations do not predict therapeutic effect.
Onset
Oral conventional tablets or solution: Within 30 minutes.
Oral inhalation aerosol: Within 5–15 minutes.
Oral nebulization solution: Within 5 minutes.
Duration
Oral inhalation aerosol: 3–6 hours.
Oral nebulization solution: 2–4 hours, occasionally ≥6 hours.
Oral conventional tablets: Up to 8 hours.
Oral extended-release tablets: Up to 12 hours.
Oral solution: Up to 6 hours.
Food
Reduces the rate of absorption of albuterol sulfate extended-release tablets.
Distribution
Extent
Albuterol crosses the placenta. Not known whether albuterol distributes into milk.
Elimination
Metabolism
Extensively metabolized in the intestinal wall and liver to inactive metabolites.
Elimination Route
Substantially eliminated by kidneys. Approximately 72% of a dose (oral inhalation) excreted in urine as unchanged drug and metabolites within 24 hours. About 76% of a single dose (oral administration) excreted in urine over 3 days; about 4% is excreted in feces.
Half-life
Oral inhalation: 3.8–6 hours in healthy adults, 1.7–7.1 hours in patients with asthma.
Conventional tablets: 5–7.2 hours.
Extended-release tablets: 9.3 hours.
Oral solution: 5 hours in healthy individuals.
Stability
Storage
Oral
Extended-release tablets: 20–25°C; protect from light.
Conventional tablets: 20–25°C; protect from light.
Oral solution: 2–30°C or 20–25°C, depending on manufacturer; protect from light.
Oral Inhalation
Albuterol sulfate inhalation aerosol: 15–25°C (ProAir HFA, Proventil HFA, Ventolin HFA). Failure to use inhalers within these respective temperature ranges could result in delivery of improper doses.
Albuterol sulfate in fixed combination with ipratropium bromide inhalation aerosol: 25°C (may be exposed to 15–30°C); protect from excessive humidity.
Albuterol sulfate oral inhalation solution: 2–25°C or 15–30°C depending on manufacturer. Discard albuterol sulfate oral inhalation concentrate solution if the solution changes color or becomes cloudy. Discard albuterol sulfate solution for nebulization (in single-use units) if it becomes discolored.
Albuterol sulfate in fixed combination with ipratropium bromide oral inhalation solution: 2–25°C.
Actions
-
Stimulates β-adrenergic receptors with little or no effect on α-adrenergic receptors.
-
Stimulates the production of cyclic adenosine-3′,5′-monophosphate (AMP), which mediates numerous cellular responses, including smooth muscle relaxation and inhibiting the release of mediators from mast cells in the airways.
-
Relaxes smooth muscles from the trachea to the terminal bronchial tree.
Advice to Patients
-
Importance of providing patient with a copy of the manufacturer’s patient information.
-
Importance of adequate understanding of proper storage, preparation, and inhalation techniques, including use of the nebulization delivery system.
-
Importance of adherence to dosing schedules of albuterol and concomitant therapy, including not exceeding the recommended dose or frequency of use unless otherwise instructed by a clinician.
-
Importance of administering albuterol at least 15–30 minutes prior to exercise for prevention of exercise-induced bronchospasm.
-
If decreased effectiveness occurs, discontinue albuterol and contact a clinician; do not increase the dose or frequency of administration.
-
Advise that the outer coating of albuterol extended-release tablets may be excreted in feces where it may be noticeable.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2 mg (of albuterol) per 5 mL* |
Albuterol Sulfate Syrup |
|
|
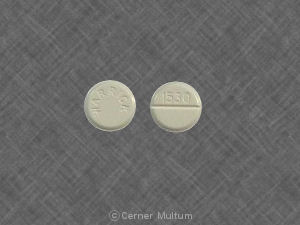
Tablets |
2 mg (of albuterol)* |
Albuterol Sulfate Tablets |
||
|
4 mg (of albuterol)* |
Albuterol Sulfate Tablets |
|||
|
Tablets, extended-release |
4 mg (of albuterol)* |
VoSpire ER |
Dava |
|
|
Albuterol Sulfate Extended-Release Tablets |
||||
|
8 mg (of albuterol)* |
VoSpire ER |
Dava |
||
|
Albuterol Sulfate Extended-Release Tablets |
||||
|
Oral Inhalation |
Aerosol |
90 mcg (of albuterol) per metered spray |
ProAir HFA (with hydrofluoroalkane propellant) |
Teva |
|
Proventil HFA (with hydrofluoroalkane propellant) |
Schering |
|||
|
Ventolin+ HFA (with hydrofluoroalkane propellant) |
GlaxoSmithKline |
|||
|
Solution, for nebulization |
0.021% (of albuterol)* |
AccuNeb (available as TwistFlex polyethylene vials) |
Dey |
|
|
Albuterol Sulfate Inhalation Solution |
||||
|
0.042% (of albuterol)* |
AccuNeb (available as TwistFlex polyethylene vials) |
Dey |
||
|
Albuterol Sulfate Inhalation Solution |
||||
|
0.083% (of albuterol)* |
Albuterol Sulfate Inhalation Solution |
|||
|
Proventil |
Schering |
|||
|
Solution, concentrate, for nebulization |
0.5% (of albuterol)* |
Albuterol Sulfate Inhalation Solution |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Aerosol |
90 mcg (of albuterol) with Ipratropium Bromide 18 mcg per metered spray |
Combivent (with chlorofluorohydrocarbon propellants) |
Boehringer Ingelheim |
|
Solution, for nebulization |
2.5 mg (of albuterol) with Ipratropium Bromide 0.5 mg per 3 mL |
DuoNeb |
Dey |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution, for nebulization |
0.103 mg (of levalbuterol) per mL (0.31 mg) |
Xopenex (available as polyethylene vials) |
Sepracor |
|
0.21 mg (of levalbuterol) per mL (0.63 mg) |
Xopenex (available as polyethylene vials) |
Sepracor |
||
|
0.417 mg (of levalbuterol) per mL (1.25 mg) |
Xopenex (available as polyethylene vials) |
Sepracor |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Aerosol |
45 mcg (of levalbuterol) per metered spray |
Xopenex HFA (with hydrofluoroalkane propellant) |
Sepracor |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 13, 2012. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Can asthma inhalers cause a sore throat?
- Can you use an expired albuterol inhaler?
- Does either Ventolin or albuterol contain steroids?
- Does coffee help with asthma?
- What is albuterol sulfate and can I take it if I'm allergic to sulfa?
- How do you use the ProAir Digihaler?
More about albuterol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (389)
- Drug images
- Latest FDA alerts (6)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: adrenergic bronchodilators
- Breastfeeding
- En español
Patient resources
Professional resources
- Albuterol Sulfate, Levalbuterol Hydrochloride, Levalbuterol Tartrate (Systemic, Oral Inhalation) monograph
- Albuterol (FDA)
- Albuterol Aerosol (FDA)
- Albuterol Extended-Release Tablets (FDA)
- Albuterol Inhalation Solution (FDA)
Other brands
Ventolin, ProAir HFA, Proventil HFA, ProAir RespiClick, ProAir Digihaler