Naltrexone (Monograph)
Brand name: Vivitrol
Drug class: Opiate Antagonists
Introduction
Opioid antagonist.
Uses for Naltrexone
Opioid Use Disorder
Management of opioid use disorder as part of a comprehensive program that includes psychosocial support.
Blocks the effects of exogenously administered opioids to prevent relapse to opioid dependence in individuals who have undergone detoxification.
Naltrexone hydrochloride has been designated an orphan drug by FDA for blockade of the pharmacological effects of exogenously administered opioids as an adjunct to the maintenance of the opioid-free state in detoxified formerly opioid-dependent individuals.
Available as oral tablets and extended-release injectable IM suspension for this use.
Current evidence does not support use of oral naltrexone for prevention of opioid use disorder, except in specific situations (e.g., highly motivated patients who are able to adhere to daily dosing).
Extended-release injectable naltrexone is considered an effective treatment for patients who are able to give consent, are fully withdrawn from opioids, and have no contraindications to therapy.
Medications used in the treatment of opioid use disorder (e.g., methadone, buprenorphine, naltrexone) have been associated with reduced risk of overdose and deaths. Evidence-based treatment with these drugs should be offered to all patients who meet criteria for opioid use disorder.
When determining whether to use methadone, buprenorphine, or naltrexone, clinicians should consider the patient's preferences, past treatment history, current clinical condition, and treatment setting.
Compared with the other treatments, naltrexone is a long-acting opioid antagonist that does not produce euphoria and does not have addictive properties; however, adherence rates with naltrexone treatment are historically low.
Has been used for rapid or ultrarapid detoxification in the management of opioid withdrawal.† [off-label]. Due to high risk for adverse events or death, ultrarapid opioid detoxification currently not recommended. Naltrexone-facilitated opioid withdrawal can be a safe and effective approach, but should only be administered by experienced clinicians and in cases where anesthesia or conscious sedation are not employed.
Alcohol Use Disorder
Management of alcohol dependence in conjunction with a comprehensive program that includes counseling and other psychosocial support.
Blocks opiate receptors that are involved in the rewarding effects of drinking and craving for alcohol.
Available as oral tablets and extended-release injectable IM suspension for this use. Oral formulation is indicated for treatment of alcohol dependence; injectable formulation is indicated for treatment of alcohol dependence in patients who are able to abstain from alcohol in an outpatient setting.
Has not been shown to be effective in patients who are drinking at treatment initiation.
Behavior modification is an integral component in maintaining alcohol cessation; naltrexone has not been shown to provide any therapeutic benefit except as part of an appropriate plan of addiction management.
When used in conjunction with a comprehensive management program, naltrexone has been reported to decrease alcohol craving, reduce alcohol consumption, decrease the number of drinking days, maintain abstinence from alcohol ingestion, and prevent relapse.
Oral naltrexone is most effective for patients who are highly motivated and/or supported with observed daily dosing and who are abstinent at the time of treatment initiation. Extended-release injectable naltrexone is also most effective when prescribed to patients who are abstinent at treatment initiation. Both formulations have greatest benefit in patients who discontinue drinking on their own for several days before treatment initiation.
Medications for management of alcohol use disorder include disulfiram, acamprosate, and naltrexone. Clinicians should consider prescribing one of these agents for patients who are dependent on alcohol or who have stopped drinking but continue to experience cravings or relapses, particularly in those with moderate or severe alcohol use disorder.
When selecting a treatment, consider patient preferences, past treatment history, level of motivation for abstinence, clinical condition, contraindications, and history of medication adherence.
Patients seeking treatment for both alcohol use disorder and concurrent opioid use disorder may benefit from naltrexone.
Patients with a family history of alcohol use disorder may benefit more from naltrexone treatment than those without such a history.
Individuals with intense craving for alcohol versus low levels of craving may derive greater benefit from naltrexone therapy.
Naltrexone Dosage and Administration
General
Pretreatment Screening
-
Prior to naltrexone treatment, verify that the opioid-dependent patient (including those being treated for alcohol dependence) is opioid-free to prevent precipitating withdrawal. Before initiating naltrexone, an opioid-free interval of at least 7–10 days is recommended by the manufacturers for patients previously dependent on short-acting opioids. Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as 2 weeks.
-
In every case, always be prepared to manage withdrawal symptomatically with nonopioid medications because there is no completely reliable method for determining whether a patient has had an adequate opioid-free period. If it is uncertain whether the patient is opioid-free, a naloxone challenge test may be helpful; however, in some cases, patients may experience precipitated withdrawal despite having a negative urine toxicology screen or tolerating a naloxone challenge test.
- Naloxone Challenge Test
-
Test should not be performed in patients who are exhibiting signs and/or symptoms of opioid withdrawal, those whose urine shows evidence of opiates, or those in whom there is a high degree of suspicion that opioids are still being used, since naloxone may precipitate potentially severe opioid withdrawal.
-
Naloxone may be administered IV or sub-Q in the challenge test.
-
IV challenge test: Administer 0.2 mg naloxone hydrochloride initially; observe the patient for 30 seconds for evidence of opioid withdrawal. If no evidence of withdrawal is observed, inject the remaining 0.6-mg dose and observe the patient for an additional 20 minutes for evidence of withdrawal.
-
Sub-Q challenge test: Administer 0.8-mg dose of naloxone hydrochloride and observe the patient for 20 minutes for evidence of opioid withdrawal.
-
If signs and symptoms of opioid withdrawal occur or there is any doubt about the test result, delay naltrexone therapy and repeat the naloxone challenge test in 24 hours with the 0.8-mg dose. If there is any doubt about the test result, hold naltrexone and repeat the test in 24 hours.
Patient Monitoring
-
Monitor for the emergence of depression or suicidal thinking.
-
Perform liver function tests prior to and during therapy in patients with preexisting hepatic impairment.
-
Monitor patients with psychiatric disorders during therapy since depression and suicidal ideation have been reported with naltrexone therapy.
Dispensing and Administration Precautions
-
Healthcare providers administering naltrexone should always be prepared to manage opioid withdrawal.
Administration
Administer orally or by IM injection. Do not administer parenteral preparation by IV or sub-Q injection.
Therapy may be initiated with parenteral preparation; not necessary to initiate therapy with oral naltrexone and then switch to parenteral preparation.
Oral Administration
Administer orally.
Supervised administration of daily oral dosing is recommended to improve compliance.
IM Administration
Administer onlyby deep IM injection into the upper outer quadrant of the gluteal muscle every 4 weeks (or once a month); alternate buttocks for subsequent injections. Administer only with needle and other components of dose pack supplied by manufacturer.
Allow the drug to reach room temperature prior to reconstitution. To reconstitute, inject 3.4 mL of the provided diluent into the vial containing 380 mg of naltrexone microsphere powder; vigorously shake the vial for approximately 1 minute. See the manufacturer's prescribing information for complete preparation instructions.
Visually inspect the suspension for particulate matter and discoloration prior to administration. A properly mixed suspension will be milky white, will not contain clumps, and will move freely down the wall of the vial.
Immediately after suspension, withdraw 4.2 mL of the suspension. Evaluate the patient's body habitus prior to each injection to determine whether the 1.5-inch or the 2-inch needle (both supplied by the manufacturer) is more appropriate for gluteal IM injection in that patient. Replace the preparation needle with the appropriate needle for administration. Consider alternative treatment for any patient whose body habitus (i.e., gluteal fat thickness) precludes IM injection with one of the provided needles.
Use aspiration to avoid inadvertent injection into a blood vessel.
Do not administer by IV or sub-Q injection; do not inadvertently administer into fatty tissue. Inadvertent sub-Q injection may increase likelihood of severe injection site reactions.
Dosage
Available for oral administration as naltrexone hydrochloride; dosage is expressed in terms of the salt.
Available for IM administration as naltrexone base anhydrous; dosage is expressed in terms of naltrexone.
The following dosage recommendations are usual dosages recommended by the manufacturer; alternative flexible dosing schedules in which the dose and/or frequency of administration are altered have also been suggested.
Adults
Opioid Use Disorder
Oral
Initially, 25 mg; if no evidence of withdrawal, begin 50 mg daily.
IM
380 mg every 4 weeks or once a month.
Alcohol Use Disorder
Oral
Recommended dosage is 50 mg once daily for most patients.
In clinical studies establishing efficacy, patients were treated for up to 12 weeks; other dose or durations of therapy were not evaluated.
IM
380 mg every 4 weeks or once a month.
Special Populations
Hepatic Impairment
The manufacturer of naltrexone hydrochloride tablets makes no specific dosage recommendations for patients with hepatic impairment. Dosage adjustment not required for naltrexone extended-release injection in patients with mild or moderate hepatic impairment. Not evaluated in patients with severe hepatic impairment.
Renal Impairment
The manufacturer of naltrexone hydrochloride tablets makes no specific dosage recommendations for patients with renal impairment. Dosage adjustment not required for naltrexone extended-release injection in patients with mild renal impairment. Caution recommended in patients with moderate to severe renal impairment.
Cautions for Naltrexone
Contraindications
-
Patients receiving opioid analgesics.
-
Patients with current physiologic opioid dependence, including those currently maintained on opiate agonists (e.g., methadone) or partial agonists (e.g., buprenorphine).
-
Patients in acute opioid withdrawal.
-
Patients who have failed the naloxone challenge test or who have a positive urine screen for opioids.
-
Patients with known hypersensitivity to naltrexone or any components of the products.
Warnings/Precautions
Vulnerability to Opioid Overdose
After opioid detoxification, patients are likely to have reduced tolerance to opioids and may respond to lower doses of opioids than previously used. May result in potentially life-threatening opioid overdose (e.g., respiratory compromise or arrest, circulatory collapse) if previously tolerated doses of opioids are used.
Cases of overdosage with fatal outcomes reported after patients discontinued treatment with naltrexone.
Self-administration of large doses of opioids in an attempt to overcome the antagonist activity of naltrexone may cause life-threatening opioid intoxication or overdosage.
Inform patients of this increased sensitivity to opioids and risk of overdosage as well as consequence of attempting to overcome the opioid blockade. It is important that patients inform family members and the people closest to the patient of this increased sensitivity to opioids and the risk of overdose.
Advise patients and caregivers of the importance of having access to naloxone for emergency treatment of opioid overdose. Educate patients and caregivers on how to recognize signs and symptoms of opioid overdose and how to treat with naloxone.
Emphasize importance of calling 911 or seeking emergency medical help in all cases of known or suspected opioid overdose, even if naloxone is administered.
Precipitated Opioid Withdrawal
May precipitate withdrawal in patients physically dependent on opioids.
Opioid-dependent individuals who are candidates for naltrexone therapy should remain free of opioids for a minimum of 7–10 days for patients previously dependent on short-acting opioids; up to 14 days may be required for those transitioning from methadone or buprenorphine.
Monitor patients closely in an appropriate medical setting where precipitated withdrawal can be managed if a decision is made by the healthcare provider for a more rapid transition from agonist to antagonist therapy.
There is no completely reliable method for determining whether a patient has had an adequate opioid-free period; healthcare providers should always be prepared to manage withdrawal.
Patients may sometimes experience precipitated withdrawal despite a negative urine toxicology screen or tolerating a naloxone challenge test (usually in the setting of transitioning from buprenorphine treatment).
Patients treated for alcohol dependence with extended-release naltrexone suspension should also be assessed for underlying opioid dependence and for any recent use of opioids prior to initiation of treatment.
Hepatotoxicity
Hepatitis and clinically significant liver dysfunction reported. Transient, asymptomatic hepatic transaminase elevations also observed but may be due to other causes.
Opioid withdrawal that is precipitated abruptly may lead to systemic sequelae, including acute liver injury.
Advise patients of risk of hepatic injury and to seek medical attention if they experience symptoms of acute hepatitis. Discontinue naltrexone if signs and symptoms of hepatotoxicity occur.
Some experts recommend against use of naltrexone in patients with serum aminotransferase concentrations >5 times the ULN unless benefits outweigh risks.
Conduct liver function tests prior to and during therapy in patients with preexisting hepatic impairment.
Depression and Suicidality
Depression, suicide, attempted suicide, and suicidal ideation reported in patients receiving naltrexone for opioid use disorder or alcohol use disorder. No causal relationship demonstrated, but endogenous opioids may be a contributing factor.
Monitor patients for depression or suicidal thinking. If any such symptoms occur, advise patient to inform their healthcare provider.
Ultrarapid Opioid Withdrawal
Safe use of naltrexone in ultrarapid opioid detoxification programs not established and not recommended.
Injection-site Reactions
Injection-site reactions (e.g., pain, tenderness, induration, swelling, erythema, bruising, pruritus) reported with the injectable suspension; some cases were severe and required surgical intervention.
Evaluate patients exhibiting signs of abscess, cellulitis, necrosis, or extensive swelling to determine if referral to a surgeon is warranted.
Naltrexone injections must be prepared and administered by a healthcare professional. Administer injections only as a deep IM gluteal injection. Inadvertent sub-Q injections may increase likelihood of severe injection site reactions.
Consider alternate treatment for patients whose body habitus precludes IM gluteal injection with one of the manufacturer-provided needles.
Reversal of Naltrexone Blockade for Pain Management
In an emergency situation in patients receiving naloxone, options for pain management include regional analgesia or use of non-opioid analgesics.
Continuously monitor patients if opioid therapy is required in an anesthesia care setting. Care should be provided by persons not involved in the conduct of the surgical or diagnostic procedure and by individuals specifically trained in the use of anesthetic drugs and management of the respiratory effects of potent opioids.
Monitor patients closely by appropriately trained personnel in a setting equipped and staffed for cardiopulmonary resuscitation.
Eosinophilic Pneumonia
Eosinophilic pneumonia, sometimes requiring hospitalization, reported with use of extended-release injectable suspension.
Consider diagnosis of eosinophilic pneumonia if dyspnea and hypoxemia develops, particularly in patients who do not respond to antibiotics. Advise patients of this risk and to seek medical attention if they develop symptoms of pneumonia.
Hypersensitivity Reactions
Hypersensitivity reactions (urticaria, angioedema, and anaphylaxis) observed with use of extended-release injectable suspension.
If a hypersensitivity reaction occurs, advise patient to seek immediate medical attention in a healthcare setting prepared to treat anaphylaxis; discontinue naltrexone therapy.
Administration Precautions
Administer IM injections of naltrexone with caution to patients with thrombocytopenia or any coagulation disorder (e.g., hemophilia, severe hepatic failure).
Alcohol Withdrawal
Use of naltrexone does not eliminate nor diminish alcohol withdrawal symptoms.
Laboratory Test Interferences
Naltrexone may be cross-reactive with certain immunoassay methods for the detection of drugs of abuse (specifically opioids) in urine. Refer to specific immunoassay instructions for more information.
Specific Populations
Pregnancy
In animal reproduction studies, oral naltrexone increased the incidence of early fetal loss. No adequate and well-controlled studies in pregnant women. Use during pregnancy only if potential benefits justify potential risk to fetus.
Untreated opioid addiction in pregnancy is associated with adverse obstetrical outcomes. Alcohol use is associated with fetal harm including growth restriction, facial abnormalities, CNS abnormalities, behavioral disorders, and impaired intellectual development.
Lactation
Naltrexone and its major metabolite, 6β-naltrexol, are present in human milk. There are no data on the effects on the breastfed infant or on milk production.
Pediatric Use
Use in pediatric patients <18 years of age not established.
Geriatric Use
Clinical studies of injectable naltrexone did not include sufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger patients.
Naltrexone is substantially excreted by the kidney; risk of adverse reactions may be greater in patients with impaired renal function. Elderly patients are more likely to have decrease renal function. Monitor renal function.
Hepatic Impairment
Patients with severe hepatic impairment not adequately studied.
Pharmacokinetics in patients with mild to moderate hepatic impairment are not altered; dosage adjustment not required.
Patients with compensated and decompensated liver cirrhosis have been reported to have approximately 5- and 10-fold higher naltrexone AUC, respectively, compared with subjects with normal liver function. Alterations in naltrexone bioavailability are related to liver disease severity.
Renal Impairment
Patients with severe renal impairment not adequately studied.
Caution is advised in patients with renal impairment as the drug and its primary metabolite are excreted primarily in the urine.
Common Adverse Effects
Extended-release injectable suspension in patients with opioid use disorder (≥2% and at least twice as frequent as with placebo): hepatic enzyme abnormalities, injection site pain, nasopharyngitis, insomnia, toothache.
Oral tablets in patients with opioid use disorder (≥10%): difficulty sleeping, anxiety, nervousness, abdominal pain/cramps, nausea and/or vomiting, low energy, joint and muscle pain, headache.
Extended-release injectable suspension in patients with alcohol use disorder (≥5% and at least twice as frequent as with placebo): nausea, vomiting, injection site reactions (including induration, pruritus, nodules and swelling), muscle cramps, dizziness or syncope, somnolence or sedation, anorexia, decreased appetite or other appetite disorders.
Oral tablets in patients with alcohol use disorder (≥2%): depression, nausea, headache, dizziness, nervousness, fatigue, insomnia, vomiting, anxiety, somnolence.
Drug Interactions
Concomitant administration with drugs other than opioid agonists not studied; therefore, use caution when coadministering naltrexone with other drugs.
CYP isoenzyme system not involved in naltrexone metabolism.
Does not inhibit or induce major CYP enzymes.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Disulfiram |
Both drugs are potentially hepatotoxic |
Manufacturers recommend concomitant use only if the potential benefits justify the possible risks |
|
Glyburide |
May increase serum concentrations of naltrexone |
Monitor for increased toxicity of naltrexone |
|
Opioid agonists |
Patients receiving naltrexone may not benefit therapeutically from opiate-containing preparations, including those used for the management of cough and cold, diarrhea, and pain |
Avoid use of opiate-containing preparations during naltrexone therapy when alternative nonopiate therapy is available Avoid use of naltrexone in patients receiving opiates or in nondetoxified patients physically dependent on opiates |
|
Opioid antagonists, peripherally acting |
Do not use naltrexone concomitantly with methylnaltrexone or naloxegol |
|
|
Tests, urinary opiates |
Possible interference with some enzymatic assays for opiates No interference reported with thin-layer (TLC), gas-liquid (GLC), or high-performance liquid (HPLC) chromatography assays for methadone or morphine |
|
|
Thioridazine |
Possible increased lethargy and somnolence |
|
|
Tests, urinary quinine |
No interference reported with TLC, GLC, or HPLC methods |
Naltrexone Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely (about 96%) absorbed following oral administration.
Plasma Concentrations
Peak plasma levels of both naltrexone and 6β-naltrexol occur within 1 hour of oral dosing.
After IM administration of extended-release injection, plasma concentration time profile characterized by a transient initial peak approximately 2 hours after injection, followed by a second peak approximately 2-3 days later.
Beginning approximately 14 days after dosing with extended-release injection, concentrations slowly decline, with measurable levels beyond 1 month.
Distribution
Plasma Protein binding
Low (21%) binding over the therapeutic range.
Elimination
Metabolism
CYP isoenzyme system not involved in metabolism.
Extensively metabolized and produces primary metabolite, 6β-naltrexol. Less 6β-naltrexol is generated following IM administration compared with oral administration due to a reduction in first-pass hepatic metabolism.
Profile of oral administration suggests that naltrexone and its metabolites may undergo enterohepatic recycling. Profile also suggests that naltrexone and its metabolites may appears to have extra-hepatic sites of drug metabolism and its major metabolite undergoes active tubular secretion.
Elimination
Primarily in the urine, with minimal unchanged drug.
Half-life
Elimination half life of extended-release injectable suspension is 5-10 days and is dependent on the erosion of the polymer. Elimination half life of 6β-naltrexol following extended-release injectable suspension administration is 5-10 days.
Mean elimination half-life after oral administration for naltrexone and 6β-naltrexol are 4 hours and 13 hours, respectively.
Stability
Storage
Oral
Tablets
Store at 20–25°C.
Parenteral
Extended-release injectable suspension
Store carton in refrigerator (2–8°C). Do not freeze.
May store unrefrigerated at ≤25°C for ≤7 days prior to administration. Do not expose unrefrigerated product to temperatures >25°C.
Actions
-
Opioid antagonist with little or no agonist activity.
-
Thought to act as a competitive antagonist at the µ, κ, and δ opioid receptors in the CNS; appears to have highest affinity for the μ receptor. Major metabolite, 6β-naltrexol, is also an opioid antagonist and may contribute to antagonist activity.
-
In usual doses in patients who have not recently received opioids, naloxone exerts little or no pharmacologic effect, but may produce pupillary constriction by an unknown mechanism.
-
In patients who have received single or repeated large doses of opioid agonists, naltrexone attenuates or produces a complete but reversible block of the pharmacologic effects (e.g., physical dependence, analgesia, euphoria, tolerance) of the opioid.
-
Blocks the effects of opioids by competitive binding at opioid receptors. This makes the blockade produced potentially surmountable, but overcoming full naltrexone blockade by administration of opioids may result in non-opioid receptor-mediated symptoms such as histamine release.
-
Does not produce physical or psychologic dependence, and tolerance to the drug’s opioid antagonist activity reportedly does not develop. May precipitate mild to potentially severe withdrawal in individuals physically dependent on opioids.
-
Alcohol ingestion stimulates release of endogenous opioid agonists, which may increase rewarding effects associated with alcohol ingestion through agonist activity at opioid (e.g., μ) receptors. By competitively binding to opioid receptors, naltrexone may reduce alcohol consumption by blocking the effects of endogenous opioids and thus making alcohol ingestion less pleasurable.
-
Does not cause disulfiram-like reactions following ingestion of alcohol as a result of opioid or alcohol use.
Advice to Patients
-
Advise patients that if they previously used opioids, they may be more sensitive to lower doses of opioids and at risk of accidental overdose should they use opioids when their next naltrexone dose is due, if they miss a dose, or after naltrexone treatment is discontinued. It is important that patients inform family members and the people closest to the patient of this increased sensitivity to opioids and the risk of overdose. Educate patients and caregivers on how to recognize the signs and symptoms of an opioid overdose.
-
Advise patients that because naltrexone can block the effects of opioids, patients will not perceive any effect if they attempt to self-administer heroin or any other opioid drug in small doses while on naltrexone. Caution that administration of large doses of heroin or any other opioid to try to bypass the blockade and get high while on naltrexone may lead to serious injury, coma, or death.
-
Discuss with the patient and caregiver the importance of having access to naloxone. Inform them of options for obtaining it, as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program). Educate patients and caregivers on how to recognize the signs and symptoms of an opioid overdose and how to use naloxone in the event of a suspected overdose. Explain to patients and caregivers that naloxone’s effects are temporary, and that they must call 911 or get emergency medical help right away in all cases of known or suspected opioid overdose, even if naloxone is administered.
-
Inform patients that they may not experience the expected effects from opioid containing analgesic, antidiarrheal, or antitussive medications while they are on naltrexone therapy.
-
Patients should be free of all opioids, including opioid-containing medicines, for a minimum of 7 to 10 days before starting naltrexone in order to avoid precipitation of opioid withdrawal. Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as two weeks. Ensure that patients understand that withdrawal precipitated by administration of an opioid antagonist may be severe enough to require hospitalization if they have not been opioid-free for an adequate period of time, and is different from the experience of spontaneous withdrawal that occurs with discontinuation of opioid in a dependent individual. Advise patients that they should not take naltrexone if they have any symptoms of opioid withdrawal. Advise all patients, including those with alcohol dependence, that it is imperative to notify healthcare providers of any recent use of opioids or any history of opioid dependence before starting naltrexone to avoid precipitation of opioid withdrawal.
-
Advise patients that naltrexone may cause liver injury. Patients should immediately notify their physician if they develop symptoms and/or signs of liver disease.
-
Advise patients that they may experience depression while taking naltrexone. Inform family members and the people closest to the patient that they are taking naltrexone and that they should call a doctor right away should they become depressed or experience symptoms of depression.
-
Advise patients that naltrexone has been shown to be effective only when used as part of a treatment program that includes counseling and support.
-
Advise patients that dizziness may occur with naltrexone treatment, and they should avoid driving or operating heavy machinery until they have determined how naltrexone affects them.
-
Advise patient to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
- Extended-release Injection
-
Instruct patients that naltrexone extended-release injectable suspension must be prepared and administered by a healthcare provider.
-
Advise patients that a reaction at the administration site of naltrexone extended-release injectable suspension may occur. Reactions include pain, tenderness, induration, swelling, erythema, bruising, or pruritus. Serious injection site reactions including necrosis may occur. Some of these injection site reactions have required surgery. Patients should be advised to seek medical attention for worsening skin reactions.
-
Advise patients to carry documentation to alert medical personnel to the fact that they are taking naltrexone extended-release injectable suspension. This will help to ensure that patients obtain adequate medical treatment in an emergency.
-
Advise patients that naltrexone extended-release injectable suspension may cause an allergic pneumonia. Patients should immediately notify their physician if they develop signs and symptoms of pneumonia, including dyspnea, coughing, or wheezing.
-
Advise patients that they should not take naltrexone extended-release injectable suspension if they are allergic to naltrexone or any of the microsphere or diluent components.
-
Advise patients that they may experience nausea following the initial injection of naltrexone . Patients are less likely to experience nausea in subsequent injections. Patients should be advised that they may also experience tiredness, headache, vomiting, decreased appetite, painful joints and muscle cramps.
-
Advise patients that because naltrexone extended-release injectable suspension is an intramuscular injection and not an implanted device, once it is injected, it is not possible to remove it from the body.
-
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injectable suspension, extended-release, for IM use |
380 mg |
Vivitrol (available as a dose pack containing a single-dose vial of naltrexone microspheres, diluent, needles, and syringe) |
Alkemes |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
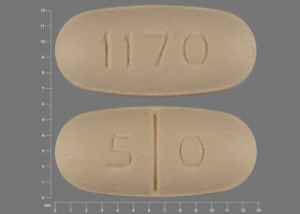
Oral |
Tablets, film-coated |
50 mg* |
Naltrexone Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What is low dose naltrexone (LDN)?
- What happens if you drink alcohol while taking naltrexone?
- What to avoid when taking naltrexone?
- Should I take naltrexone in the morning or at night?
- Does naltrexone cause weight gain?
- Acamprosate vs naltrexone: How do they compare?
- How long does naltrexone take to work?
- How does naltrexone make you feel?
- What is the mechanism of action for naltrexone?
More about naltrexone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (604)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antidotes
- Breastfeeding