Ketamine Hydrochloride (Monograph)
Brand name: Ketalar
Drug class: Non-barbiturates
Warning
Notice: On October 10, 2023, FDA issued a warning to patients and health care providers about potential risks associated with compounded ketamine products, including oral formulations, for the treatment of psychiatric disorders.Ketamine is not FDA approved for the treatment of any psychiatric disorder. In addition, compounded drugs, including compounded ketamine products, are not FDA approved and have not been evaluated for safety, effectiveness, or quality prior to marketing. Home use of compounded ketamine products presents additional risk because onsite monitoring by a health care provider is not available. FDA has identified potential safety concerns associated with the use of compounded ketamine products from compounders and telemedicine platforms, including abuse and misuse, psychiatric events, increases in blood pressure, respiratory depression, and lower urinary tract and bladder symptoms. For additional information see [Web].825
Introduction
General anesthetic that also has analgesic and antidepressant properties;1 3 4 5 an N-methyl-d-aspartate (NMDA) receptor antagonist.1 3 4 5 9 10 26 35
Uses for Ketamine Hydrochloride
Induction and Maintenance of Anesthesia
Used IV or IM for induction of anesthesia prior to administration of other general anesthetic agents.1 3 9 10
Used as the sole anesthetic agent for diagnostic and surgical procedures that do not require skeletal muscle relaxation.1
Also may be used as a supplement to other anesthetic agents.1
Produces dissociative anesthesia (i.e., a trance-like cataleptic state characterized by profound analgesia and amnesia, with retention of protective airway reflexes, spontaneous respirations, and cardiopulmonary stability), which differs markedly from the anesthetic state produced by other general anesthetics (e.g., barbiturates, benzodiazepines, propofol, inhalation anesthetics).1 5 11 35
Due to risk of emergence reactions and availability of other anesthetic agents, current use generally limited to certain patient populations (e.g., hemodynamically compromised patients) and settings (e.g., prehospital environments that lack appropriate monitoring and respiratory support) where the drug's unique pharmacologic properties may be particularly advantageous.3 9 44 51
Produces sympathomimetic effects and may be particularly useful in hemodynamically unstable patients (e.g., those with traumatic injury or septic shock).3 9 10
Because of its bronchodilating effects, generally considered the induction agent of choice in patients with reactive airway disease (e.g., asthma) or active bronchospasm.3 9 10
Manufacturer states that safety and effectiveness not established in patients <16 years of age;1 however, the drug has been used widely in pediatric patients† [off-label].3 9 23
Procedural Sedation
Used as a procedural sedation agent to facilitate short painful or emotionally disturbing procedures (e.g., fracture reduction, laceration repair, abscess drainage, emergency cardioversion, chest tube insertion, central line placement) in the emergency department and other clinical settings.1 3 4 9 10 11 14 79 89 106 109 214 821 823
Administration of a single IV or IM dose can effectively provide dissociative sedation for approximately 5–10 or 20–30 minutes, respectively, while maintaining cardiovascular stability, spontaneous respiration, and protective airway reflexes.1 11
In contrast to other procedural sedation agents, ketamine does not follow usual sedation continuum; once the dissociative threshold has been reached, additional administration of ketamine will not enhance or deepen sedation.11 824
Widely used for procedural sedation in pediatric patients† [off-label]; used less frequently in adults because of increased risk of emergence delirium.3 9 11 78 79 89 106 821 823
Has a well-established role in burn patients undergoing painful procedures (e.g., dressing changes, debridement, grafts).3 9 10 23
Availability of the IM route is advantageous in patients in whom IV administration may be difficult (e.g., severely agitated or combative patients, young children, patients with extensive burns).3 9 11 23 821
Commonly administered in combination with propofol to provide deep sedation for painful procedures.9 10 89 107 108
Postoperative Pain
Has been used in low (i.e., subanesthetic or subdissociative) doses as part of a multimodal regimen for postoperative pain† [off-label] in adults and pediatric patients.3 10 25 27 28 29 30 34 75 76 82 97 98 99 100 101 102 103
Efficacy of low-dose ketamine in the postoperative setting is well established; clinical studies have demonstrated reduced opiate requirements and, in some cases, additional reductions in pain.3 10 27 29 33 34 75 76 82
Appears to provide most benefit for patients undergoing procedures associated with severe postoperative pain (e.g., thoracic, abdominal, orthopedic surgeries).25 27 31 32 76 82 Some experts state that benefit not demonstrated in patients undergoing procedures associated with mild postoperative pain (e.g., tonsillectomy, head and neck surgery);25 for such procedures, standard analgesia with low dosages of opiates, NSAIAs, and local anesthetics can usually provide adequate pain relief.27 76
May be particularly useful in the management of opiate-tolerant or opiate-dependent patients undergoing surgery.25 82 Also may be considered as an adjunct to reduce postoperative opiate requirements in patients with increased risk of opiate-related respiratory depression (e.g., those with obstructive sleep apnea).25
Acute Pain
Has been used (in subanesthetic doses) alone or as an adjunct to other analgesics (e.g., opiates) for relief of acute pain† [off-label] in emergency department or prehospital settings.3 9 10 14 15 16 17 18 19 20 21 22 24 25 83 84 Reported to provide comparable reduction in pain scores to IV morphine.14 21 22
When used as an adjunct to opiate analgesics, ketamine may reduce pain scores and/or decrease opiate requirements.14 16 17 18 19 20 84
Studies evaluating subanesthetic ketamine for acute pain generally conducted in the adult population.16 17 18 19 20 21 22 24 However, low or subanesthetic doses of ketamine also have been used for analgesia in pediatric patients ≥3 months of age presenting to the emergency department.11 84
Although evidence is limited, ketamine may be useful in opiate-dependent patients with acute exacerbations of chronic pain conditions (e.g., sickle cell disease)† [off-label].25
Chronic Pain
Has been used as an adjunct analgesic for management of chronic pain of various etiologies, including complex regional pain syndrome (CRPS)†, neuropathic pain associated with spinal cord injury†, phantom limb pain†, fibromyalgia†, ischemic pain†, cancer pain†, and migraine†.3 9 10 26 42 43 44 45 46 47 48 52 53 54 86 87
Evidence of efficacy varies depending on specific chronic pain condition; some evidence supports short-term benefits of ketamine infusions for certain conditions associated with a neuropathic component.3 10 26 31 42 43 44 46 48 49 50 86 87
There is weak to moderate evidence supporting use for CRPS.26 47 85 There is weak evidence supporting use for neuropathic pain associated with spinal cord injury.26 49 86 87 Evidence remains inconclusive for cancer-related pain, mixed neuropathic pain, phantom limb pain, postherpetic neuralgia, fibromyalgia, ischemic pain, migraine, and low-back pain.3 4 26 46 54
Additional study needed to establish role of ketamine in patients with chronic pain, and to determine optimum dosages, durability of response, and long-term benefits and risks.10 26 31 43 48 52 53 54
Treatment-resistant Depression and Suicidality
Has been used in low (i.e., subanesthetic) doses for the treatment of severe and treatment-resistant depression associated with major depressive disorder or bipolar disorder†.300 301 302 303 304 305 306 307 309 311 312 313 314 315 317 320 326 327
In controlled studies, single, low-dose IV infusions of ketamine resulted in approximately 37–71% response rates in patients with treatment-resistant depression.300 317 Limited clinical experience in patients with bipolar disorder; not known if such patients respond differently to ketamine than patients with major depressive disorder.314
Multiple-infusion regimens of ketamine (i.e., weekly, biweekly, 3 times weekly) appear to be more effective in depressed patients than single infusions and can prolong remission.303 306 307 312 313 314 315 However, long-term efficacy and safety of repeated doses not fully determined.300 306 307 312 314 Although not observed to date, multiple-infusion regimens potentially may cause long-term cognitive impairment and/or neurotoxicity.307 312 314 Some clinicians suggest that short-term use of ketamine to produce rapid antidepressant and antisuicidal effects until a less invasive relapse prevention strategy can be implemented may be optimal.312
Has been used in the short-term treatment of suicidal ideation†.304 307 310 314 317 323 324 325 326 In a systematic review and meta-analysis, suicidal ideation rapidly decreased following IV infusions of ketamine even among patients whose depression did not fully respond to ketamine therapy, suggesting the drug may have a partially independent antisuicidal effect.307 310
Preliminary evidence suggests that intranasal† ketamine can rapidly improve depressive symptoms in patients with major depressive disorder and is generally well tolerated; however, further studies are needed to more clearly determine the efficacy, tolerability, and optimal dosing of this alternative route of administration.305 314 317 Pending further accumulation of safety data from controlled settings, the APA's Council of Research Task Force on Novel Biomarkers and Treatments currently advises against the prescription of self-administration of ketamine at home and recommends medical supervision whenever the drug is used.302
Despite the increasing use of ketamine to treat patients with treatment-resistant depression and suicidality and the rapid increase in the number of facilities offering ketamine therapy (e.g., ketamine infusion centers and psychiatric clinics), some clinicians currently recommend limiting ketamine's use to controlled settings under the care of skilled clinicians.302 308 316 If ketamine is used outside of a controlled setting, careful screening, monitoring during treatment, and follow-up of patients are necessary.302 314 316
When considering the use of ketamine for mood disorders, the APA's Council of Research Task Force on Novel Biomarkers and Treatments recommends balancing the potential benefits of ketamine infusion therapy with the potential risks of long-term exposure (e.g., neurotoxicity, cystitis, abuse potential).302 314 320
Some clinicians consider electroconvulsive therapy (ECT) to be first-line therapy for patients with refractory depression and are concerned that a trial of ketamine might delay patients from being referred for an ECT consultation.308 Preliminary experience with the adjunctive use of ketamine in the course of ECT for depression does not suggest improved efficacy or tolerability.314
Sedation and Analgesia in Critical Care Settings
Has been used by continuous IV infusion to provide ICU sedation†; there is limited but increasing experience describing such use.9 12 116 117 800
Also has been used for pain management in critically ill patients†.12 25 111 800 Although evidence is limited, some experts suggest the use of low-dose ketamine as an adjunct to opiates when attempting to reduce opiate requirements in postsurgical ICU patients.800
Ketamine Hydrochloride Dosage and Administration
General
Pretreatment Screening
-
Obtain baseline liver function tests, including alkaline phosphatase and gamma glutamyl transferase, in patients receiving ketamine as part of a treatment plan that utilizes recurrent dosing.1
Patient Monitoring
-
Continuously monitor vital signs and cardiac function during administration of ketamine.1 Maintain adequate oxygenation and ventilation.1
Dispensing and Administration Precautions
-
When used for general anesthesia, administer by or under supervision of clinicians experienced in the use and complications of general anesthetics.1 23 26 When used in anesthetic doses, administer in a monitored setting in the presence of personnel trained in advanced airway management and cardiovascular life support; resuscitative equipment should be readily available.1 11 23 26
-
When used in subanesthetic doses in the emergency department, adverse effects generally are mild and self-limiting; therefore, some experts state that ketamine administration may follow the same procedures and policies used for other analgesics in this setting.83 84 Consult local protocols since expectations may differ.84
-
When used for procedural sedation in the emergency department, administer by appropriately trained individuals who can safely administer and manage complications of the drug.11 Experts recommend the presence of 2 individuals during procedure (one to perform procedure and one to monitor patient).11 Patients should be continuously observed by a dedicated healthcare professional until recovery is well established.11
-
When used by IV infusion for mood disorders (e.g., treatment-resistant depression, suicidality)†, administer by experienced clinicians in a facility where adequate monitoring for and management of possible adverse reactions (e.g., altered cardiovascular and respiratory function, acute dissociative and psychotomimetic effects) are possible.302
Other General Considerations
-
May administer benzodiazepines (e.g., diazepam, midazolam) concomitantly to reduce risk of psychotomimetic effects during emergence in adults receiving ketamine anesthesia.1 11 26 Routine benzodiazepine prophylaxis is not recommended in pediatric patients because of uncertain benefit.11
-
Administer anticholinergic agents (e.g., atropine, glycopyrrolate) prior to or concomitantly with ketamine to reduce hypersalivation and risk of laryngospasm.1 10 11 Because of uncertain benefit, some experts state that such prophylaxis should be reserved for patients with clinically important hypersalivation or impaired ability to mobilize secretions.11
-
Consider the risk of aspiration and vomiting; the manufacturer states that ketamine is not recommended in patients who have not followed “nothing by mouth (NPO)” guidelines.1 11 Although protective laryngeal and pharyngeal reflexes generally are preserved with ketamine, coadministered anesthetics and muscle relaxants may impair such reflexes.1 11
-
Because nausea and vomiting may occur following ketamine administration,1 11 14 16 25 prophylactic use of antiemetics (e.g., ondansetron) may be beneficial, particularly in patients at higher risk (e.g., early adolescents receiving ketamine for procedural sedation).11 14 93 94 95
Administration
Usually administered by slow (e.g., over 60 seconds) IV injection, IV infusion, or IM injection.1 3 4 5 10 35 51 Also has been administered by oral†,3 5 25 35 52 intranasal†,3 5 10 25 35 302 305 314 317 rectal†,3 5 35 sub-Q†,3 53 54 56 intraosseous (IO)†,3 5 10 epidural†, and intrathecal† routes.3 5 35 Because of concerns about potential neurotoxicity, some experts recommend that neuraxial administration be avoided.9 23 26 27 51 82
Also been used in IV patient-controlled analgesia (PCA), either as the sole analgesic or in combination with opioids to improve pain control and reduce opioid-related adverse effects.25
IV administration is preferred when access can be obtained readily;11 IV access can permit convenient administration of additional doses for longer procedures and allow for rapid treatment of adverse effects (e.g., IV benzodiazepines for emergence reactions).11
IM administration is associated with a higher rate of vomiting and longer recovery times compared with IV administration, but may be useful in certain patients (e.g., severely agitated or uncooperative patients, young children).3 9 11 35
IV Administration
Dilution
Do not administer ketamine 100 mg/mL IV without proper dilution; must dilute the commercially available injection concentrate with an equal volume of sterile water for injection, 0.9% sodium chloride injection, or 5% dextrose injection prior to IV injection.1
To prepare a solution containing 1 mg/mL for IV infusion, add 500 mg of ketamine (10 mL from a vial containing 50 mg/mL or 5 mL from a vial containing 100 mg/mL) to an infusion bag containing 500 mL of 0.9% sodium chloride injection or 5% dextrose injection.1 In patients requiring fluid restriction, may prepare a solution containing 2 mg/mL for IV infusion by adding 500 mg of ketamine (10 mL from a vial containing 50 mg/mL or 5 mL from a vial containing 100 mg/mL) to an infusion bag containing 250 mL of 0.9% sodium chloride injection or 5% dextrose injection.1 Manufacturer states that dilutions using the 10-mg/mL concentration of ketamine not recommended.1
Use immediately after dilution.1
Rate of Administration
For induction of anesthesia, administer slowly (e.g., over 60 seconds); rapid IV administration can cause respiratory depression and enhanced vasopressor response.1 11 12 Induction dose may be administered by IV infusion at rate of 0.5 mg/kg per minute.1
For maintenance of anesthesia, repeat one-half to full induction dosages as needed; may be given by slow microdrip infusion technique at a dosage of 0.1–0.5 mg/minute.1
For dissociative sedation in emergency department settings, IV administration over 30–60 seconds has been recommended.11
When ketamine is used in subanesthetic doses for acute pain†, some clinicians recommend that the drug be administered as a short IV infusion over 15 minutes.15
When ketamine is used for severe and treatment-resistant depression and/or suicidality†, the drug is usually given as an IV infusion over 40 minutes.300 301 302 303 304 306 307 312 315 326 327 Clinical experience with shorter and longer infusion rates is too limited302 322 to recommend their use at this time.302
Standardize 4 Safety
Standardized concentrations for ketamine have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see[Web]. 249 250 251
Ketamine is not included in the adult continuous infusion standards250
|
Patient Population |
Concentration standard |
Dosing units |
|---|---|---|
|
Pediatric patients (<50 kg) |
2 mg/mL 10 mg/mL |
mg/kg/hr |
|
Patient Population |
Concentration standard |
Dosing units |
|---|---|---|
|
Pediatric patients (<50 kg) |
2 mg/mL |
mg/kg/hr |
|
10 mg/mL |
||
|
Adults |
5 mg/mL |
mg/kg/hr |
|
10 mg/mL |
Dosage
Available as ketamine hydrochloride; dosage expressed in terms of ketamine.1
Dosage depends on intended use and desired pharmacologic effect.10 37 Ketamine produces analgesia and sedation at low doses and a state of dissociative anesthesia at higher doses.23 26 37
Doses at or above the dissociative threshold are referred to as “dissociative” or “anesthetic,” and doses below the threshold are referred to as “subdissociative” or “subanesthetic.”11 35 Although specific dosing ranges have not been established,14 25 31 dissociation generally appears at an IV dose of approximately 1–1.5 mg/kg or an IM dose of approximately 3–5 mg/kg.11 14 25 34 37 Once the dissociative threshold is reached, additional administration of ketamine will not enhance or deepen sedation.11
Pediatric Patients
Anesthesia
When used for anesthesia, individual response is variable and can depend on factors such as dosage, route of administration, patient age, or concomitant drugs; individualize dosage based on therapeutic response and patient's anesthetic requirements.1 10
Higher doses generally correspond with longer anesthesia recovery times.1
Purposeless and tonic-clonic movements of extremities may occur during the course of anesthesia; such movements do not imply a light plane of consciousness and are not indicative of the need for additional doses or anesthesia.1
Rapid induction of anesthesia occurs following IV injection; the patient should be in a supported position during administration.1
In general, pediatric patients require higher doses of ketamine compared with adults, although there is considerable interpatient variability.23
Induction and Maintenance of Anesthesia
IVSome experts recommend an initial dose of 1–3 mg/kg for induction of anesthesia in pediatric patients†; may give supplemental IV doses of 0.5–1 mg/kg if clinically indicated.23
Because of possible airway complications, some experts state that ketamine is contraindicated in infants <3 months of age.11
IMSome experts recommend a dose of 5–10 mg/kg for induction of anesthesia in pediatric patients†.23 11
Because of possible airway complications, some experts state that ketamine is contraindicated in infants <3 months of age.11
Procedural Sedation
Because dissociation occurs rapidly, administer ketamine just prior to initiating procedure.11
IV
Dissociative sedation in pediatric patients† ≥3 months3 11 of age undergoing short painful or emotionally disturbing procedures in the emergency department: 1.5–2 mg/kg administered by IV injection over 30–60 seconds.11 Although single dose usually sufficient, may administer additional incremental doses of 0.5–1 mg/kg every 5–15 minutes as needed if initial sedation is inadequate or additional doses are needed for longer procedures.11
Although some experts state that minimum IV dose that will reliably elicit the dissociative state is 1.5 mg/kg,11 lower doses (e.g., 0.25–1 mg/kg) also have been used, particularly if a dissociative effect is not required for the procedure.11 23 78
IM
Dissociative sedation in pediatric patients† ≥3 months3 11 of age undergoing short painful or emotionally disturbing procedures in the emergency department: 4–5 mg/kg.11 37 Although single dose usually sufficient, may administer additional IM doses of 2–5 mg/kg after 5–10 minutes if initial sedation is inadequate or additional doses are needed for longer procedures.11
Although some experts state that minimum IM dose that will reliably elicit the dissociative state is 4–5 mg/kg,11 lower doses (e.g., 1–2 mg/kg) also have been used, particularly if a dissociative effect is not required for the procedure.11 23
Sedation and Analgesia in Critical Care Settings†
IV
ICU sedation: Optimal dosage not known.12 116 117 800 Although dosages have varied, they generally fall within the range associated with analgosedative effects (0.02–3 mg/kg per hour by continuous IV infusion); the desired target level of sedation and concomitant use of other sedative/analgesic agents may influence dose variability.116 117
Postoperative Pain†
IV
Bolus doses of 0.1–0.5 mg/kg with or without continuous IV infusion (at rates usually ranging from 0.1–0.6 mg/kg per hour) commonly used in clinical studies in adults and pediatric patients; however, dosages and timing of administration in relation to surgical procedure varied widely and optimum dosage regimen not known.9 10 25 25 27 30 31 33 34 82 97 98 99 100 101 102 103
Some experts state there is moderate evidence supporting use of IV bolus doses up to 0.35 mg/kg and IV infusions up to 1 mg/kg per hour as an adjunct to opiates for perioperative analgesia.25
In several studies, administration of a single IV dose of ketamine 0.5 mg/kg (alone or in combination with other analgesics) was effective in achieving postoperative pain control in children undergoing tonsillectomy.9 97 98 100 102 103
Because of possible airway complications, some experts state that ketamine is contraindicated in infants <3 months of age.11
IM
IM administration of analgesic agents for postoperative pain not recommended because of substantial pain and unreliable absorption.82
Acute Pain†
IV
Acute pain in emergency department or prehospital settings: Usually, 0.1–0.3 mg/kg administered as a slow IV injection or short IV infusion over 10–15 minutes based on studies conducted principally in adults; although longer infusions are rare in this setting, continuous IV infusions of 0.1–0.3 mg/kg per hour have been given.9 10 14 16 18 20 21 22 84
Acute pain in settings without intensive monitoring: Some experts state that IV bolus doses generally should not exceed 0.35 mg/kg and infusion rates generally should not exceed 1 mg/kg per hour.25
Because of possible airway complications, some experts state that ketamine is contraindicated in infants <3 months of age.11
IM
Dosage range not definitively established; analgesic effects are less predictable when administered IM.84
Chronic Pain†
IV
There is no consensus on dosages or administration protocols; the drug generally is administered in subanesthetic doses by IV infusion.26 35 42 43 44 45 48
Some evidence suggests that administration of higher dosages over longer periods and more frequent infusions may provide more benefit.26 43 44
In a study in children and adolescents 12–17 years of age with chronic pain conditions (e.g., chronic headache, fibromyalgia, CRPS), ketamine was administered by continuous IV infusion at a rate of 0.1–0.3 mg/kg per hour for 4–8 hours each day up to a maximum of 16 hours (in total, up to a maximum of 3 consecutive days).45
Children with severe cancer-related pain have received IV infusions of ketamine at 0.1–1 mg/kg per hour.53
Because of possible airway complications, some experts state that ketamine is contraindicated in infants <3 months of age.11
Adults
Anesthesia
When used for anesthesia, individual response is variable and can depend on factors such as dosage, route of administration, patient age, or concomitant drugs; individualize dosage based on therapeutic response and patient's anesthetic requirements.1 10
Higher doses generally correspond with longer anesthesia recovery times.1
Purposeless and tonic-clonic movements of extremities may occur during the course of anesthesia; such movements do not imply a light plane of consciousness and are not indicative of the need for additional doses or anesthesia.1
Induction and Maintenance of Anesthesia
IVInitially, 1–4.5 mg/kg by slow IV injection over 60 seconds.1 On average, a dose of 2 mg/kg will produce 5–10 minutes of surgical anesthesia within 30 seconds of injection.1 51
May administer additional IV doses of 0.5–4.5 mg/kg as needed.1 A continuous IV infusion of 1–6 mg/kg per hour also has been recommended for maintenance of anesthesia.26 Adjust dosage based on patient's anesthetic requirements and concomitant use of other anesthetic agents.1
May use a slow microdrip IV infusion of 0.1–0.5 mg/minute to maintain general anesthesia after induction with ketamine.1
Emergence reactions may be reduced by using lower dosages of ketamine augmented with an IV benzodiazepine, such as diazepam, for induction and maintenance anesthesia.1
IMInitially, 6.5–13 mg/kg.1 A dose of 10 mg/kg will usually produce 12–25 minutes of surgical anesthesia within 3–4 minutes of injection.1 51
May administer additional IM doses of 3.25–13 mg/kg as needed.1 Adjust dosage based on patient's anesthetic requirements and concomitant use of other anesthetic agents.1
Procedural Sedation
Because dissociation occurs rapidly, administer ketamine just prior to initiating procedure.11
IV
Dissociative sedation in adults undergoing short painful or emotionally disturbing procedures in the emergency department: 1 mg/kg administered by IV injection over 30–60 seconds.11 Although single dose usually sufficient, may administer additional doses of 0.5–1 mg/kg every 5–15 minutes if initial sedation is inadequate or additional doses are needed for longer procedures.11
Lower IV doses (e.g., 0.2–0.75 mg/kg) have been used, particularly if a dissociative effect is not required for the procedure.11 26
IM
Although IM route not preferred in adults, may administer 4–5 mg/kg.11 Single dose usually sufficient; however, may administer additional IM doses of 2–5 mg/kg after 5–10 minutes if initial sedation is inadequate or additional doses are needed for longer procedures.11
Lower IM doses (e.g., 0.4–2 mg/kg) have been used, particularly if a dissociative effect is not required for the procedure.11 26
Sedation and Analgesia in Critical Care Settings†
IV
ICU sedation: Optimal dosage not known.12 116 117 800 Although dosages have varied, they generally fall within the range associated with analgosedative effects (0.02–3 mg/kg per hour by continuous IV infusion); the desired target level of sedation and concomitant use of other sedative/analgesic agents may influence dose variability.116 117 Lower dosages have been more commonly used when ketamine is used as part of patient-controlled analgesia.116 117 Use of initial bolus IV injections (range 0.3–0.5 mg/kg) and continuous infusion titration based on sedation or pain scores have also been reported.116 117
Pain management in the ICU: Some experts suggest low-dose ketamine (e.g., 0.5 mg/kg by IV injection followed by IV infusion of 0.06–0.12 mg/kg per hour) as an adjunct to opioid therapy in postsurgical adults in the ICU; other dosage regimens also have been used.12 116 800
Postoperative Pain†
IV
Bolus doses of 0.1–0.5 mg/kg with or without continuous IV infusion (at rates usually ranging from 0.1–0.6 mg/kg per hour) commonly used in clinical studies; however, dosages and timing of administration in relation to surgical procedure varied widely and optimum dosage regimen not known.9 25 27 30 31 33 34 82
Some experts state there is moderate evidence supporting use of IV bolus doses up to 0.35 mg/kg and IV infusions up to 1 mg/kg per hour as an adjunct to opiates for perioperative analgesia.25
IM
IM administration of analgesic agents for postoperative pain not recommended because of substantial pain and unreliable absorption.82
Acute Pain†
IV
Acute pain in emergency department or prehospital settings: Usually, 0.1–0.3 mg/kg administered as a slow IV injection or short IV infusion over 10–15 minutes; although longer infusions are rare in this setting, continuous IV infusions of 0.1–0.3 mg/kg per hour (1.67–5 mcg/kg per minute) have been given.9 10 16 18 20 21 22 84
Acute pain in settings without intensive monitoring: Some experts state that IV bolus doses generally should not exceed 0.35 mg/kg and infusion rates generally should not exceed 1 mg/kg per hour (16.67 mcg/kg per minute).25
IM
Dosage range not definitively established; analgesic effects are less predictable when administered IM.84
Chronic Pain†
IV
There is no consensus on dosages or administration protocols; the drug generally is administered in subanesthetic doses by IV infusion.26 35 42 43 44 48
Some evidence suggests that administration of higher dosages over longer periods and more frequent infusions may provide more benefit.26 43 44
Some experts state that it is reasonable to initiate with a single outpatient infusion at a minimum dose of 80 mg for at least 2 hours and then reassess before initiating further treatments.26 IV bolus doses up to 0.35 mg/kg or infusions of 0.5–2 mg/kg per hour have been recommended; however, higher (e.g., up to 7 mg/kg per hour for refractory pain) or lower (e.g., 0.1–0.5 mg/kg per hour) infusion rates also have been used successfully.26 43 50
Treatment-resistant Depression and Suicidality†
IV
Usually given in subanesthetic doses of 0.5 mg/kg by IV infusion over 40 minutes.300 301 302 303 304 306 307 312 315 326 Although a higher infusion dosage (e.g., 0.75 mg/kg) has been used in a limited number of chronically ill and/or severely treatment-resistant patients, further studies are needed to determine efficacy and safety of higher-dosage regimens.322
Obese patients (i.e., body mass index [BMI] ≥30) may be at increased risk for adverse hemodynamic effects and may benefit from adjusting dosage to calculated ideal body weight rather than actual body weight; further clinical experience to determine optimal dosing in such patients is needed.300 302 315
Limited experience with longer-term (multiple-dose) ketamine infusion therapy; however, IV infusions have been given once, twice, or 3 times weekly for 2 weeks during the acute treatment phase in some patients300 302 303 306 307 312 313 315 and sometimes have been continued once or twice weekly for another 2–4 weeks during the continuation phase for a total of 4–6 weeks of therapy or gradually tapered.302 313 315 Patients not responding to several initial infusions appear unlikely to respond to subsequent infusions.302 Some experts recommend discontinuing therapy if the interval between infusions cannot be extended to 1 week or longer by the second month of treatment; these experts state that the goal should be to eventually taper and discontinue treatment until additional long-term safety data are available.302
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations.1
Renal Impairment
Manufacturer makes no specific dosage recommendations.1
Geriatric Patients
Select dosage with caution because of greater frequency of decreased hepatic, renal, and/or cardiac function, and of concomitant disease or other drug therapy in geriatric patients.1
Cautions for Ketamine Hydrochloride
Contraindications
-
Patients in whom substantial BP elevation would constitute a serious hazard.1
-
Known hypersensitivity to ketamine or any ingredient in the formulation.1
-
Some experts state that relative contraindications may include history of airway instability, tracheal surgery, or tracheal stenosis; active pulmonary infection or disease; known or suspected cardiovascular disease (e.g., angina, CHF, hypertension); CNS masses, abnormalities, or hydrocephalus; elevated IOP (e.g., glaucoma, acute globe injury); and porphyria, hyperthyroidism, or concomitant thyroid replacement therapy.11
Warnings/Precautions
Cardiovascular Effects
Transient mild to moderate increases in BP, heart rate, and cardiac output may occur as a result of ketamine's sympathomimetic effects.1 3 11 26 40 Hypotension, bradycardia, arrhythmias, and cardiac decompensation reported.1
When used for treatment-resistant depression and suicidality, elevated BP and/or heart rate may occur during IV infusions of ketamine; these hemodynamic effects usually are transient and subside following completion of the infusion.300 302 307 312 313 326 Short-term antihypertensive therapy sometimes has been used to treat ketamine infusion-associated BP elevations in some patients.300 315
Monitor vital signs and cardiac function during ketamine administration.1 Generally avoid use in patients with known or suspected cardiac conditions (e.g., unstable angina, CAD, MI, CHF, hypertension) that may be exacerbated by sympathomimetic effects of the drug.11 25 26
Contraindicated in patients in whom a substantial elevation of BP would constitute a serious hazard; monitor cardiac function continuously in patients who experience hypertension or cardiac decompensation during ketamine anesthesia.1
Emergence Reactions
Emergence reactions may occur during recovery period in patients receiving ketamine anesthesia; duration is generally a few hours.1 Reported more frequently in adults than pediatric patients.11 51
Emergence manifestations vary in severity from pleasant to unpleasant dream-like states, vivid imagery, hallucinations, alterations in mood and body image, floating sensations, extracorporeal (out-of-body) experiences, and emergence delirium; in some cases, these states have been accompanied by confusion, excitement, and irrational behavior, which some patients recall as an unpleasant experience.1 5 10 11 51 Manufacturer states that no residual psychologic effects reported with ketamine use during induction and maintenance of anesthesia.1
IM administration associated with reduced incidence of emergence reactions.1
Incidence of psychological manifestations during emergence may be reduced if verbal, tactile, and visual stimulation of the patient is minimized during the recovery period (should not preclude appropriate monitoring of vital signs), or with prophylactic administration of benzodiazepines (e.g., diazepam, midazolam) in conjunction with lower than recommended dosages of ketamine.1 11 26
Benzodiazepines may be used to terminate severe or unpleasant emergence reactions.11 26
Respiratory Effects
Adverse respiratory effects are rare with ketamine;11 however, respiratory depression may occur following rapid IV administration or overdosage of the drug.1
Maintain adequate oxygenation and ventilation.1 Administer IV injections slowly (e.g., over 60 seconds).1
When used in subanesthetic doses for the treatment of depression in otherwise healthy individuals, ketamine is unlikely to cause clinically important adverse respiratory effects.302
Risks with Pharynx, Larynx, or Bronchial Tree Procedures
Avoid use as a sole anesthetic for procedures of the pharynx, larynx, or bronchial tree; ketamine does not suppress pharyngeal and laryngeal reflexes.1 Muscle relaxants may be required for successful completion of these procedures.1
Pediatric Neurotoxicity
Prolonged use of general anesthetics and sedation drugs, including ketamine, in children younger than 3 years of age or during the third trimester of pregnancy may affect brain development.1 750 753 In animal studies, use of anesthetic and sedation drugs that block N-methyl-d-aspartic acid (NMDA) receptors and/or potentiate γ-aminobutyric acid (GABA) activity for >3 hours led to widespread neuronal and oligodendrocyte cell loss and alterations in synaptic morphology and neurogenesis in the developing brain, resulting in long-term deficits in cognition and behavior.1 750 752 753 Across animal species, vulnerability to these neurodevelopmental changes occurs during the period of rapid brain growth thought to correlate with the third trimester of pregnancy through the first year of life in humans, but may extend to approximately 3 years of age.1 750 Clinical relevance to humans is not known.1 750
Some clinical evidence available demonstrating that a single, relatively brief exposure to general anesthesia in generally healthy children is unlikely to cause clinically detectable deficits in global cognitive function or serious behavioral disorders;750 751 752 however, further research is needed to fully characterize the effects of exposure to general anesthetics in early life, particularly for prolonged or repeated exposures and in more vulnerable populations (e.g., less healthy children).750
No specific general anesthetic or sedation drug is less likely to cause neurocognitive deficits than any other such drug.1 750 When procedures requiring the use of general anesthetics or sedation drugs are considered for young children or pregnant women, discuss the benefits, risks (including potential risk of adverse neurodevelopmental effects), and appropriate timing and duration of the procedure with the patient, parent, or caregiver.750 753 No need to delay or avoid medically necessary procedures.750 753
Hepatic Injury
Recurrent use (e.g., misuse/abuse or medically supervised unapproved indications) associated with hepatobiliary dysfunction, most often a cholestatic pattern.1 Obtain baseline liver function tests, including alkaline phosphatase and gamma glutamyl transferase, in patients who receive recurrent doses of ketamine as part of a treatment plan.1 Monitor patients receiving recurrent therapy at periodic intervals.1
Elevated hepatic enzyme concentrations reported,26 particularly following prolonged infusion and/or repeated doses within a short time frame.27 44 Hepatotoxicity has been reported following longer-term use (e.g., more than 3–4 days).3 4 26 38 44 Hepatic enzyme concentrations generally return to baseline over several months.26 44
Increased Intracranial Pressure
Increased intracranial pressure may occur;1 11 however, there is evidence that ketamine can be safely and effectively used in patients with head injuries or risk of intracranial hypertension.3 4 12 14 67
Studies suggest that intracranial pressure increases are minimal in patients with normal ventilation11 12 and are associated with concomitant elevations in cerebral perfusion.12
Manufacturer states that patients with elevated intracranial pressure should be in a monitored setting with frequent neurologic assessments;1 some experts state that ketamine should be avoided in such patients.25
Use with caution or avoid use in patients with CNS masses, abnormalities, or hydrocephalus.11
Other Warnings and Precautions
Laryngospasm
Laryngospasm and airway obstruction may occur with ketamine.1 11
Risk of laryngospasm is low with minor oropharyngeal procedures typically performed in the emergency department; avoid vigorous stimulation of posterior pharynx and accumulation of secretions or blood during these procedures.11
Ocular Effects
Elevation of IOP may occur.1 23 Use with caution or avoid use in patients with elevated IOP (e.g., glaucoma, acute globe injury).11 25 26
Genitourinary Effects
Urinary tract complications, including dysuria, urinary frequency, urgency, urge incontinence, cystitis, hematuria, postmicturition pain, and secondary renal failure, reported, generally in association with chronic ketamine use or abuse.1 3 4 26 27 35 38 44 51 57 302
In patients experiencing urinary symptoms without evidence of infection, consider interruption of ketamine therapy and evaluation by a specialist.4 Manufacturer states to consider discontinuance of ketamine if genitourinary pain continues in the setting of other genitourinary symptoms.1 Some experts advise that patients receiving long-term ketamine therapy for mood disorders be assessed for urinary symptoms (e.g., discomfort) during therapy.302
Schizophrenia/Psychosis
May exacerbate schizophrenia;11 35 generally avoid use in patients with schizophrenia or active psychosis.11 25 26 Caution advised when used for procedural sedation or acute pain in patients with other psychiatric disorders,11 including substance abuse-induced psychosis.15
Abuse, Tolerance, and Dependence
Ketamine is a known drug of abuse1 3 4 35 41 44 51 and is subject to control under the Federal Controlled Substances Act of 1970 as a schedule III drug.1 41
Most commonly abused by nasal insufflation (i.e., snorting) of the evaporated powder, although IV, IM, and oral routes also used.35 41 Most cases of ketamine abuse reported in the context of multidrug or polysubstance abuse.51
Pharmacologic and behavioral effects of ketamine are similar to, but somewhat less intense and shorter in duration than those of phencyclidine (PCP).41
Reported desired effects include feelings of dissociation and unreality, altered state of consciousness, enhanced sensory perception, hallucinations, intoxication, mild euphoria, and sensation of floating.3 35 44 51
Although brief exposure in a hospital setting is not likely to cause addiction, the possibility exists and patients should be assessed for their risk.25
Long-term abuse associated with urinary tract complications, hepatobiliary toxicity, neuropsychiatric effects (e.g., hallucinatory flashbacks, inability to concentrate, memory impairment), and MRI abnormalities.1 2 3 4 26 27 35 38 39 41 44 51 57
Tolerance and dependence may develop following prolonged administration.1 35 51
Cases of ketamine abuse resulting in physical or psychologic dependence have been reported.41 Withdrawal symptoms (e.g., craving, fatigue, poor appetite, anxiety) reported following discontinuation of frequent (more than weekly) use of large doses of ketamine for long periods.1
Specific Populations
Pregnancy
No adequate and well-controlled studies in pregnant women.1 Not recommended for use during pregnancy or delivery; safety not established.1
Respiratory depression and low Apgar scores requiring resuscitation reported in some neonates exposed to ketamine at maternal IV doses of ≥1.5 mg/kg during delivery.2 Marked increases in maternal BP and uterine tone observed at IV doses >2 mg/kg.2
Based on animal data, repeated or prolonged use of general anesthetics and sedative drugs, including ketamine, during the third trimester of pregnancy may result in adverse neurodevelopmental effects in the fetus.750 753
Lactation
Not known whether ketamine is distributed into milk.69 70 Because the drug should be undetectable in plasma approximately 11 hours after administration, nursing after this time period should not expose infant to clinically relevant amounts of ketamine.70
Pediatric Use
Manufacturer states that safety and efficacy not established in patients <16 years of age;1 however, ketamine has been used widely in pediatric patients in a variety of settings for anesthesia, procedural sedation and analgesia, postoperative pain, and chronic pain management.3 9 11 23 25 45
Frequently used in children to facilitate painful procedures in the emergency department and is considered a drug of choice for this use.3 11 14 May be particularly useful in pediatric patients because the drug may be administered IM.3
Generally should not be used in infants <3 months of age because of potential increased risk of airway complications, including airway obstruction, laryngospasm, and apnea.3 11 14
Repeated or prolonged use of general anesthetics and sedation drugs, including ketamine, in children <3 years of age or during the third trimester of pregnancy may adversely affect neurodevelopment.750 753 In animals, use for >3 hours of anesthetic and sedation drugs that block NMDA receptors and/or potentiate GABA activity leads to widespread neuronal apoptosis in the brain and long-term deficits in cognition and behavior;750 751 752 753 clinical relevance to humans is unknown.750
Ketamine may be preferred for induction of anesthesia in children with congenital heart disease with right-to-left shunt† because of its sympathomimetic effects and hemodynamic stability.3 9 10 23
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients; other reported clinical experience has not identified any age-related differences in response.1 A reduced risk of emergence reactions has been observed in geriatric patients >65 years of age relative to younger adults.1
Hepatic Impairment
Prolonged effects of ketamine may occur in patients with cirrhosis or hepatic impairment.2
Some experts state to avoid or limit use in patients with severe hepatic disease or cirrhosis, and to use caution (with monitoring of liver function tests) in patients with moderate hepatic disease.25
Renal Impairment
Ketamine concentrations have been reported to be 20% higher in individuals with acute renal failure than in those with normal renal function.5 68
Common Adverse Effects
Most common adverse reactions are emergence reactions and elevated blood pressure and pulse.1
Drug Interactions
Metabolized mainly by CYP2B6 and CYP3A4, and to a lesser extent by other CYP enzymes.2 3 5 6 35
Drugs and Foods Affecting Hepatic Microsomal Enzymes
Drugs that inhibit or induce CYP3A4 and CYP2B6 may increase or decrease, respectively, the systemic exposure of ketamine or norketamine.2 3 5 6
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Barbiturates |
Long-term treatment: Decreased half-life and plasma concentrations of ketamine observed in patients receiving long-term therapy with barbiturates, likely due to hepatic enzyme induction62 68 |
|
|
Benzodiazepines (e.g., clorazepate, diazepam, lorazepam) |
Possible additive CNS depression and increased risk of profound sedation, respiratory depression, coma, or death2 51 Possible antagonism of antidepressant effect of ketamine based on limited evidence and mechanisms of action318 327 328 Clorazepate: Ketamine metabolism not substantially altered in patients who received IV clorazepate prior to anesthesia62 Diazepam: Increased half-life of ketamine reported in patients receiving diazepam rectally (as a single dose) prior to anesthesia; however, half-life of ketamine was decreased in patients receiving long-term oral diazepam2 62 |
Closely monitor neurological status and respiratory parameters, including respiratory rate and pulse oximetry; consider dosage adjustment based on the individual clinical situation1 When ketamine is used to treat mood disorders, consider avoiding benzodiazepines within 8–12 hours prior to ketamine infusion327 |
|
CNS depressants (e.g., alcohol, benzodiazepines, opiate agonists, skeletal muscle relaxants) |
Additive CNS depression and increased risk of profound sedation, respiratory depression, coma, or death1 2 3 51 |
Closely monitor neurological status and respiratory parameters, including respiratory rate and pulse oximetry; consider dosage adjustment based on the individual clinical situation1 |
|
Ergonovine |
||
|
Grapefruit juice |
Increased peak plasma concentration and AUC of orally administered S-ketamine by twofold and threefold, respectively6 |
May be clinically important if ketamine is administered orally6 |
|
Itraconazole |
||
|
Lamotrigine |
Possible reduced effects of ketamine, including reduced anesthetic efficacy6 8 |
|
|
Macrolide antibiotics (e.g., azithromycin, clarithromycin, erythromycin) |
Clarithromycin: Increased peak plasma concentration and AUC of orally administered S-ketamine by 3.6- and 2.6-fold, respectively, and decreased ratio of norketamine to ketamine by 54%;6 66 increased pharmacologic effects of ketamine reported6 66 Erythromycin, but not azithromycin, expected to have similar effects6 |
|
|
Neuromuscular blocking agents (e.g., atracurium) |
Atracurium: May potentiate neuromuscular blocking effects and result in respiratory depression and apnea2 63 Not known whether ketamine affects duration of other neuromuscular blocking agents63 |
|
|
Opiate agonists |
Concomitant use of opiate agonists with ketamine during anesthesia may prolong recovery time1 |
|
|
Rifampin |
Decreased AUC of orally administered S-ketamine and S-norketamine by 10 and 50%, respectively6 7 |
|
|
St. John's wort (Hypericum perforatum) |
Decreased peak plasma concentration and AUC of orally administered S-ketamine by 66 and 58%, respectively, and of S-norketamine by 18 and 23%, respectively6 |
|
|
Sympathomimetics or vasopressin |
Possible enhanced sympathomimetic effect of ketamine |
Closely monitor vital signs; consider dosage adjustments based on individual clinical situation1 |
|
Theophyllines (e.g., aminophylline, theophylline) |
Possible lowering of seizure threshold and increased risk of tonic seizures2 64 |
Consider use of an alternative to ketamine |
|
Thyroid agents |
||
|
Ticlopidine |
Increased AUC of orally administered S-ketamine by 2.4-fold6 65 and decreased ratio of norketamine to ketamine65 |
Ketamine Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Oral: 16–30%; higher relative concentrations of norketamine due to extensive first-pass metabolism.3 4 14 35
Rectal: 11–30%; higher relative concentrations of norketamine due to extensive first-pass metabolism.3 4 14 35
Intranasal: Reported up to 45–50%3 4 35 but can vary substantially.3 14
Onset
Following IV injection of 2 mg/kg, anesthesia occurs within 30 seconds.1
Following IM injection of 9–13 mg/kg, anesthesia occurs within 3–4 minutes.1
Following a single IV infusion, improvement in depression usually occurs within several hours to a day post-infusion.300 301 303 304 307
Duration
Following IV injection of 2 mg/kg, duration of anesthesia is 5–10 minutes.1
Following IM injection of 9–13 mg/kg, duration of anesthesia is usually 12–25 minutes.1
Plasma Concentrations
Following IV injection of 2 mg/kg, plasma ketamine concentrations are about 1.8–2 mcg/mL at 5 minutes.2
Following IM injection of 6 mg/kg, plasma ketamine concentrations are about 1.7–2.2 mcg/mL at 15 minutes.2
Major active metabolite, norketamine, appears in blood 2–3 minutes following IV administration of ketamine and reaches peak plasma concentration around 30 minutes.5
Following oral administration, peak plasma ketamine concentrations occur within 20–120 minutes.35
Plasma ketamine concentrations associated with dissociative anesthesia range from approximately 1.2–3 mcg/mL23 35 and are typically around 0.5–1.1 mcg/mL during awakening.23 35 51
Plasma ketamine concentrations associated with analgesia range from 0.07–0.2 mcg/mL.23 25 35 51 Following oral administration, analgesia occurs at plasma ketamine concentrations of 0.04 mcg/mL, possibly due to higher ratio of norketamine.51
Psychotomimetic effects may occur at plasma concentrations as low as 0.05 mcg/mL; more severe effects (e.g., anxiety, paranoid feelings) occur around plasma concentrations of 0.5 mcg/mL.5 51
Following IV infusion of 0.5 mg/kg over 40 minutes, peak plasma ketamine concentrations of 0.07–0.2 mcg/mL are achieved; these concentrations are usually associated with antidepressant effects but not general anesthetic effects.35 302
Special Populations
Lower IM bioavailability reported in children.35
In children 4–10 years of age, plasma ketamine concentrations are similar to those observed in adults.5 Plasma norketamine concentrations are higher in children than adults following equivalent weight-adjusted doses.5
Distribution
Extent
Rapidly and widely distributed into highly perfused tissues, including the CNS, with a distribution half-life of 10–15 minutes.2 3 5 14 Highly concentrated in body fat, liver, and lung in animal studies.2
Termination of anesthetic effect occurs partly via redistribution from CNS to peripheral tissues and partly by hepatic biotransformation.1 2
Crosses placenta.2 Following IM injection of 250 mg (approximately 4.2 mg/kg) in parturient patients, placental transfer rate from maternal artery to umbilical vein was 47% at an average of 12 minutes from the time of injection to vaginal delivery.2
Plasma Protein Binding
<50% (to α1-acid glycoprotein or albumin).5 12
Elimination
Metabolism
Metabolized extensively in the liver,2 4 9 35 principally undergoing N-demethylation by CYP2B6 and CYP3A4 and to a lesser extent by other CYP enzymes.1 Norketamine demonstrates approximately one-third the anesthetic activity of the parent drug.3 4 5 6 12
Also undergoes hydroxylation of the cyclohexone ring,1 9 conjugation with glucuronic acid, and dehydration of the hydroxylated metabolites to form a cyclohexene derivative.1
Norketamine is further metabolized to hydroxynorketamines and dehydronorketamine.35
Elimination Route
About 90% of a parenteral dose is excreted in the urine, mostly as conjugates of hydroxylated metabolites;2 3 4 10 <5% of a dose is excreted unchanged in feces and urine.4
Half-life
Ketamine: Approximately 2–4 hours.2 3 5 35
Norketamine: 12 hours.4
Special Populations
Half-life of ketamine is shorter in children (approximately 100 minutes) than in adults.5
In individuals with acute renal failure, 20% higher ketamine concentrations reported compared with those with normal renal function.5 68
Not appreciably removed by hemodialysis or hemofiltration (10 or 4%, respectively).68
Stability
Storage
Parenteral
Injection
20–25°C (excursions permitted between 15–30°C); protect from light.1
Actions
-
Nonbarbiturate general anesthetic that produces analgesia and sedation at low doses and a state of dissociative anesthesia at higher doses.1 3 4 5 23 26 37
-
Structurally and pharmacologically related to PCP.1 3 4 5 9 35
-
Pharmacologic effects are principally a result of the drug's action as a noncompetitive NMDA receptor antagonist.1 3 4 5 9 10 26 35 NMDA receptor plays an important role in excitatory glutamate-mediated neurotransmission, which can affect cognition, chronic pain, opiate tolerance, and mood regulation.26 NMDA receptor also is closely involved in the development of opiate tolerance, opiate-induced hyperalgesia, and central sensitization.4
-
Binds to the PCP binding site of the NMDA receptor channel, decreasing frequency of channel opening and duration of time in the open active state.3 4 5 26 35
-
Also acts on a wide range of other targets, including opiate, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), GABAA, cholinergic, nicotinic, and muscarinic receptors; hyperpolarization-activated cyclic nucleotide (HCN), calcium, sodium, and potassium channels; and the monoaminergic system.3 4 5 26 35
-
Produces dissociative anesthesia as a result of a functional and electrophysiologic dissociation between the thalamocortical and limbic systems.5 11 35 Anesthetic state is characterized by profound analgesia and amnesia, with retention of protective airway reflexes, spontaneous respirations, and cardiopulmonary stability.1 5 11 35 Appears to disrupt frontal-to-posterior corticocortical connectivity while maintaining thalamocortical somatosensory pathways at anesthetic doses.3
-
Produces analgesia and sedation at doses and plasma concentrations lower than those used for anesthesia.4 11 25 26 At subanesthetic doses, alters functional connectivity between the subgenual anterior cingulate cortex and a network cluster involving the thalamus, hippocampus, and the retrosplenial cortex without reported loss of consciousness.3
-
Precise mechanism(s) of ketamine's antidepressant activity not clearly established.303 304 317 320 321 Considerable preclinical research suggests that the NMDA class of glutamate receptors plays a role in the pathophysiology of depression as well as in the mechanism of action of antidepressant treatments.304 320 321 NMDA receptor antagonists, including ketamine, have been shown to be effective in animal models of depression and in models that predict antidepressant activity in many studies.304 320 321 Antidepressant effects of ketamine may be mediated by an increase in glutamate, which leads to a cascade of events that results in synaptogenesis and reversal of the negative effects of chronic stress and depression, particularly in the prefrontal cortex.320 321
-
Inhibits reuptake of catecholamines and has other direct and indirect sympathomimetic effects (e.g., increased heart rate, BP, myocardial and cerebral oxygen consumption, cerebral blood flow, intracranial and intraocular pressure).3 9 11 40
Advice to Patients
-
May cause residual anesthetic effects and drowsiness.1 Importance of advising patients not to operate hazardous machinery, including driving a motor vehicle, or engage in hazardous activities within 24 hours of receiving ketamine.1
-
When procedures requiring general anesthetics or sedation drugs, including ketamine, are considered for young children or pregnant women, importance of discussing with the patient, parent, or caregiver the benefits, risks (including potential risk of adverse neurodevelopmental effects), and appropriate timing and duration of the procedure.750 753
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.1
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Advise patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule III (C-III) drug.1 41
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
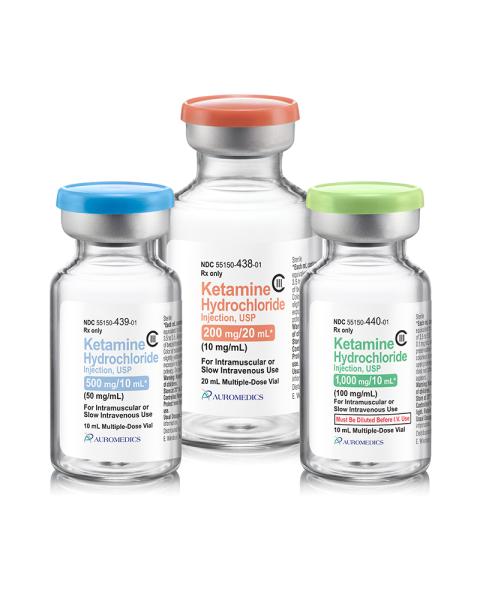
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
10 mg (of ketamine) per mL* |
Ketalar (C-III) |
Par |
|
Ketamine Hydrochloride Injection (C-III) |
||||
|
50 mg (of ketamine) per mL* |
Ketalar (C-III) |
Par |
||
|
Ketamine Hydrochloride Injection (C-III) |
||||
|
100 mg (of ketamine) per mL* |
Ketalar (C-III) |
Par |
||
|
Ketamine Hydrochloride Injection (C-III) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions January 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Par Pharmaceutical, Inc. Ketalar (ketamine hydrochloride) injection prescribing information. Chestnut Ridge, NY; 2022 Feb.
2. Pfizer Limited. Ketalar 100 mg/mL injection summary of product characteristics. Sandwich, Kent, United Kingdom; 2021 Apr. https://www.medicines.org.uk/emc/product/2231/smpc
3. Li L, Vlisides PE. Ketamine: 50 Years of Modulating the Mind. Front Hum Neurosci. 2016; 10:612. https://pubmed.ncbi.nlm.nih.gov/27965560
4. Quibell R, Fallon M, Mihalyo M et al. Ketamine. J Pain Symptom Manage. 2015; 50:268-78. https://pubmed.ncbi.nlm.nih.gov/26096492
5. Mion G, Villevieille T. Ketamine pharmacology: an update (pharmacodynamics and molecular aspects, recent findings). CNS Neurosci Ther. 2013; 19:370-80. https://pubmed.ncbi.nlm.nih.gov/23575437
6. Andrade C. Ketamine for Depression, 5: Potential Pharmacokinetic and Pharmacodynamic Drug Interactions. J Clin Psychiatry. 2017; 78:e858-e861. https://pubmed.ncbi.nlm.nih.gov/28858450
7. Noppers I, Olofsen E, Niesters M et al. Effect of rifampicin on S-ketamine and S-norketamine plasma concentrations in healthy volunteers after intravenous S-ketamine administration. Anesthesiology. 2011; 114:1435-45. https://pubmed.ncbi.nlm.nih.gov/21508826
8. Kornhall D, Nielsen EW. Failure of ketamine anesthesia in a patient with lamotrigine overdose. Case Rep Crit Care. 2014; 2014:916360. https://pubmed.ncbi.nlm.nih.gov/25114807
9. Kurdi MS, Theerth KA, Deva RS. Ketamine: Current applications in anesthesia, pain, and critical care. Anesth Essays Res. 2014 Sep-Dec; 8:283-90. https://pubmed.ncbi.nlm.nih.gov/25886322
10. Gao M, Rejaei D, Liu H. Ketamine use in current clinical practice. Acta Pharmacol Sin. 2016; 37:865-72. https://pubmed.ncbi.nlm.nih.gov/27018176
11. Green SM, Roback MG, Kennedy RM et al. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011; 57:449-61. https://pubmed.ncbi.nlm.nih.gov/21256625
12. Erstad BL, Patanwala AE. Ketamine for analgosedation in critically ill patients. J Crit Care. 2016; 35:145-9. https://pubmed.ncbi.nlm.nih.gov/27481750
14. Sheikh S, Hendry P. The Expanding Role of Ketamine in the Emergency Department. Drugs. 2018; 78:727-735. https://pubmed.ncbi.nlm.nih.gov/29651740
15. Todd KH. A Review of Current and Emerging Approaches to Pain Management in the Emergency Department. Pain Ther. 2017; 6:193-202. https://pubmed.ncbi.nlm.nih.gov/29127600
16. Johansson P, Kongstad P, Johansson A. The effect of combined treatment with morphine sulphate and low-dose ketamine in a prehospital setting. Scand J Trauma Resusc Emerg Med. 2009; 17:61. https://pubmed.ncbi.nlm.nih.gov/19943920
17. Jennings PA, Cameron P, Bernard S et al. Morphine and ketamine is superior to morphine alone for out-of-hospital trauma analgesia: a randomized controlled trial. Ann Emerg Med. 2012; 59:497-503. https://pubmed.ncbi.nlm.nih.gov/22243959
18. Galinski M, Dolveck F, Combes X et al. Management of severe acute pain in emergency settings: ketamine reduces morphine consumption. Am J Emerg Med. 2007; 25:385-90. https://pubmed.ncbi.nlm.nih.gov/17499654
19. Ahern TL, Herring AA, Stone MB et al. Effective analgesia with low-dose ketamine and reduced dose hydromorphone in ED patients with severe pain. Am J Emerg Med. 2013; 31:847-51. https://pubmed.ncbi.nlm.nih.gov/23602757
20. Beaudoin FL, Lin C, Guan W et al. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014; 21:1193-202. https://pubmed.ncbi.nlm.nih.gov/25377395
21. Miller JP, Schauer SG, Ganem VJ et al. Low-dose ketamine vs morphine for acute pain in the ED: a randomized controlled trial. Am J Emerg Med. 2015; 33:402-8. https://pubmed.ncbi.nlm.nih.gov/25624076
22. Motov S, Rockoff B, Cohen V et al. Intravenous Subdissociative-Dose Ketamine Versus Morphine for Analgesia in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2015; 66:222-229.e1. https://pubmed.ncbi.nlm.nih.gov/25817884
23. Coté CJ, Lerman J, Anderson BJ, eds. A Practice of anesthesia for infants and children. 6th ed. Philadelphia, PA: Elsevier, Inc; 2019: 140-2.
24. Ahern TL, Herring AA, Miller S et al. Low-Dose Ketamine Infusion for Emergency Department Patients with Severe Pain. Pain Med. 2015; 16:1402-9. https://pubmed.ncbi.nlm.nih.gov/25643741
25. Schwenk ES, Viscusi ER, Buvanendran A et al. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018; 43:456-466. https://pubmed.ncbi.nlm.nih.gov/29870457
26. Cohen SP, Bhatia A, Buvanendran A et al. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018; 43:521-546. https://pubmed.ncbi.nlm.nih.gov/29870458
27. Radvansky BM, Shah K, Parikh A et al. Role of ketamine in acute postoperative pain management: a narrative review. Biomed Res Int. 2015; 2015:749837. https://pubmed.ncbi.nlm.nih.gov/26495312
28. Wang L, Johnston B, Kaushal A et al. Ketamine added to morphine or hydromorphone patient-controlled analgesia for acute postoperative pain in adults: a systematic review and meta-analysis of randomized trials. Can J Anaesth. 2016; 63:311-25. https://pubmed.ncbi.nlm.nih.gov/26659198
29. Ye F, Wu Y, Zhou C. Effect of intravenous ketamine for postoperative analgesia in patients undergoing laparoscopic cholecystectomy: A meta-analysis. Medicine (Baltimore). 2017; 96:e9147. https://pubmed.ncbi.nlm.nih.gov/29390443
30. Guillou N, Tanguy M, Seguin P et al. The effects of small-dose ketamine on morphine consumption in surgical intensive care unit patients after major abdominal surgery. Anesth Analg. 2003; 97:843-7. https://pubmed.ncbi.nlm.nih.gov/12933413
31. Persson J. Ketamine in pain management. CNS Neurosci Ther. 2013; 19:396-402. https://pubmed.ncbi.nlm.nih.gov/23663314
32. Laskowski K, Stirling A, McKay WP et al. A systematic review of intravenous ketamine for postoperative analgesia. Can J Anaesth. 2011; 58:911-23. https://pubmed.ncbi.nlm.nih.gov/21773855
33. Himmelseher S, Durieux ME. Ketamine for perioperative pain management. Anesthesiology. 2005; 102:211-20. https://pubmed.ncbi.nlm.nih.gov/15618805
34. Jouguelet-Lacoste J, La Colla L, Schilling D et al. The use of intravenous infusion or single dose of low-dose ketamine for postoperative analgesia: a review of the current literature. Pain Med. 2015; 16:383-403. https://pubmed.ncbi.nlm.nih.gov/25530168
35. Zanos P, Moaddel R, Morris PJ et al. Ketamine and Ketamine Metabolite Pharmacology: Insights into Therapeutic Mechanisms. Pharmacol Rev. 2018; 70:621-660. https://pubmed.ncbi.nlm.nih.gov/29945898
36. Warner LL, Smischney N. Special K with No License to Kill: Accidental Ketamine Overdose on Induction of General Anesthesia. Am J Case Rep. 2018; 19:10-12. https://pubmed.ncbi.nlm.nih.gov/29295971
37. Green SM, Hummel CB, Wittlake WA et al. What is the optimal dose of intramuscular ketamine for pediatric sedation?. Acad Emerg Med. 1999; 6:21-6. https://pubmed.ncbi.nlm.nih.gov/9928972
38. Hong YL, Yee CH, Tam YH et al. Management of complications of ketamine abuse: 10 years' experience in Hong Kong. Hong Kong Med J. 2018; 24:175-181. https://pubmed.ncbi.nlm.nih.gov/29632275
39. Liao Y, Tang J, Liu J et al. Decreased Thalamocortical Connectivity in Chronic Ketamine Users. PLoS One. 2016; 11:e0167381. https://pubmed.ncbi.nlm.nih.gov/27977717
40. Liebe T, Li S, Lord A et al. Factors Influencing the Cardiovascular Response to Subanesthetic Ketamine: A Randomized, Placebo-Controlled Trial. Int J Neuropsychopharmacol. 2017; 20:909-918. https://pubmed.ncbi.nlm.nih.gov/29099972
41. Drug Enforcement Administration, Department of Justice. Schedules of controlled substances: placement of ketamine into schedule III. 21 CFR Part 1308. Final Rule. DEA-183F] Fed Regist. 1999; 64:37673-5. https://www.deadiversion.usdoj.gov/fed_regs/rules/1999/fr0713.htm
42. Kosharskyy B, Almonte W, Shaparin N et al. Intravenous infusions in chronic pain management. Pain Physician. 2013 May-Jun; 16:231-49. https://pubmed.ncbi.nlm.nih.gov/23703410
43. Maher DP, Chen L, Mao J. Intravenous Ketamine Infusions for Neuropathic Pain Management: A Promising Therapy in Need of Optimization. Anesth Analg. 2017; 124:661-674. https://pubmed.ncbi.nlm.nih.gov/28067704
44. Niesters M, Martini C, Dahan A. Ketamine for chronic pain: risks and benefits. Br J Clin Pharmacol. 2014; 77:357-67. https://pubmed.ncbi.nlm.nih.gov/23432384
45. Sheehy KA, Muller EA, Lippold C et al. Subanesthetic ketamine infusions for the treatment of children and adolescents with chronic pain: a longitudinal study. BMC Pediatr. 2015; 15:198. https://pubmed.ncbi.nlm.nih.gov/26620833
46. Alviar MJ, Hale T, Dungca M. Pharmacologic interventions for treating phantom limb pain. Cochrane Database Syst Rev. 2016; 10:CD006380. https://pubmed.ncbi.nlm.nih.gov/27737513
47. O'Connell NE, Wand BM, McAuley J et al. Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev. 2013; :CD009416. https://pubmed.ncbi.nlm.nih.gov/23633371
48. Michelet D, Brasher C, Horlin AL et al. Ketamine for chronic non-cancer pain: A meta-analysis and trial sequential analysis of randomized controlled trials. Eur J Pain. 2018; 22:632-646. https://pubmed.ncbi.nlm.nih.gov/29178663
49. Amr YM. Multi-day low dose ketamine infusion as adjuvant to oral gabapentin in spinal cord injury related chronic pain: a prospective, randomized, double blind trial. Pain Physician. 2010 May-Jun; 13:245-9. https://pubmed.ncbi.nlm.nih.gov/20495588
50. Connolly SB, Prager JP, Harden RN. A systematic review of ketamine for complex regional pain syndrome. Pain Med. 2015; 16:943-69. https://pubmed.ncbi.nlm.nih.gov/25586192
51. World Health Organization. Ketamine (INN) update review report agenda item 6.1. Expert committee on drug dependence 37th meeting. Geneva, Switzerland. 2015 November 16–20.
52. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Adult Cancer Pain. Version 1.2018. 2018 Jan 22. Available at https://www.nccn.org/ https://www.nccn.org
53. Bredlau AL, Thakur R, Korones DN et al. Ketamine for pain in adults and children with cancer: a systematic review and synthesis of the literature. Pain Med. 2013; 14:1505-17. https://pubmed.ncbi.nlm.nih.gov/23915253
54. Bell RF, Eccleston C, Kalso EA. Ketamine as an adjuvant to opioids for cancer pain. Cochrane Database Syst Rev. 2017; 6:CD003351. https://pubmed.ncbi.nlm.nih.gov/28657160
55. Fallon MT, Wilcock A, Kelly CA et al. Oral Ketamine vs Placebo in Patients With Cancer-Related Neuropathic Pain: A Randomized Clinical Trial. JAMA Oncol. 2018; 4:870-872. https://pubmed.ncbi.nlm.nih.gov/29621378
56. Hardy J, Quinn S, Fazekas B et al. Randomized, double-blind, placebo-controlled study to assess the efficacy and toxicity of subcutaneous ketamine in the management of cancer pain. J Clin Oncol. 2012; 30:3611-7. https://pubmed.ncbi.nlm.nih.gov/22965960
57. Jhang JF, Hsu YH, Kuo HC. Possible pathophysiology of ketamine-related cystitis and associated treatment strategies. Int J Urol. 2015; 22:816-25. https://pubmed.ncbi.nlm.nih.gov/26087832
58. Brown L, Christian-Kopp S, Sherwin TS et al. Adjunctive atropine is unnecessary during ketamine sedation in children. Acad Emerg Med. 2008; 15:314-8. https://pubmed.ncbi.nlm.nih.gov/18370983
59. Green SM, Roback MG, Krauss B et al. Predictors of emesis and recovery agitation with emergency department ketamine sedation: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009; 54:171-80.e1-4. https://pubmed.ncbi.nlm.nih.gov/19501426
60. Green SM, Roback MG, Krauss B et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009; 54:158-68.e1-4. https://pubmed.ncbi.nlm.nih.gov/19201064
61. Kim KW, Choe WJ, Kim JH et al. Anticholinergic premedication-induced fever in paediatric ambulatory ketamine anaesthesia. J Int Med Res. 2016; 44:817-23. https://pubmed.ncbi.nlm.nih.gov/27225859
62. Idvall J, Aronsen KF, Stenberg P et al. Pharmacodynamic and pharmacokinetic interactions between ketamine and diazepam. Eur J Clin Pharmacol. 1983; 24:337-43. https://pubmed.ncbi.nlm.nih.gov/6861847
63. Toft P, Helbo-Hansen S. Interaction of ketamine with atracurium. Br J Anaesth. 1989; 62:319-20. https://pubmed.ncbi.nlm.nih.gov/2930674
64. Hirshman CA, Krieger W, Littlejohn G et al. Ketamine-aminophylline-induced decrease in seizure threshold. Anesthesiology. 1982; 56:464-7. https://pubmed.ncbi.nlm.nih.gov/7081731
65. Peltoniemi MA, Saari TI, Hagelberg NM et al. Exposure to oral S-ketamine is unaffected by itraconazole but greatly increased by ticlopidine. Clin Pharmacol Ther. 2011; 90:296-302. https://pubmed.ncbi.nlm.nih.gov/21716267
66. Hagelberg NM, Peltoniemi MA, Saari TI et al. Clarithromycin, a potent inhibitor of CYP3A, greatly increases exposure to oral S-ketamine. Eur J Pain. 2010; 14:625-9. https://pubmed.ncbi.nlm.nih.gov/19897389
67. Zeiler FA, Teitelbaum J, West M et al. The ketamine effect on ICP in traumatic brain injury. Neurocrit Care. 2014; 21:163-73. https://pubmed.ncbi.nlm.nih.gov/24515638
68. Köppel C, Arndt I, Ibe K. Effects of enzyme induction, renal and cardiac function on ketamine plasma kinetics in patients with ketamine long-term analgosedation. Eur J Drug Metab Pharmacokinet. 1990 Jul-Sep; 15:259-63. https://pubmed.ncbi.nlm.nih.gov/2253657
69. Cobb B, Liu R, Valentine E et al. Breastfeeding after Anesthesia: A Review for Anesthesia Providers Regarding the Transfer of Medications into Breast Milk. Transl Perioper Pain Med. 2015; 1:1-7. https://pubmed.ncbi.nlm.nih.gov/26413558
70. Ketamine. In: Briggs GG, Freeman RK. Drug in pregnancy and lactation: a reference guide to fetal and neonatal risk. 10th ed. Philadelphia: Wolters Kluwer Health; 2015:756-7.
75. Bell RF, Dahl JB, Moore RA et al. Perioperative ketamine for acute postoperative pain. Cochrane Database Syst Rev. 2006; :CD004603. https://pubmed.ncbi.nlm.nih.gov/16437490
76. Subramaniam K, Subramaniam B, Steinbrook RA. Ketamine as adjuvant analgesic to opioids: a quantitative and qualitative systematic review. Anesth Analg. 2004; 99:482-95, table of contents. https://pubmed.ncbi.nlm.nih.gov/15271729
78. Bleiberg AH, Salvaggio CA, Roy LC et al. Low-dose ketamine: efficacy in pediatric sedation. Pediatr Emerg Care. 2007; 23:158-62. https://pubmed.ncbi.nlm.nih.gov/17413431
79. Coté CJ, Wilson S, AMERICAN ACADEMY OF PEDIATRICS et al. Guidelines for Monitoring and Management of Pediatric Patients Before, During, and After Sedation for Diagnostic and Therapeutic Procedures: Update 2016. Pediatrics. 2016; 138 https://pubmed.ncbi.nlm.nih.gov/27354454
80. Upchurch CP, Grijalva CG, Russ S et al. Comparison of Etomidate and Ketamine for Induction During Rapid Sequence Intubation of Adult Trauma Patients. Ann Emerg Med. 2017; 69:24-33.e2. https://pubmed.ncbi.nlm.nih.gov/27993308
81. Jabre P, Combes X, Lapostolle F et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009; 374:293-300. https://pubmed.ncbi.nlm.nih.gov/19573904
82. Chou R, Gordon DB, de Leon-Casasola OA et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016; 17:131-57. https://pubmed.ncbi.nlm.nih.gov/26827847
83. . Optimizing the Treatment of Acute Pain in the Emergency Department. Ann Emerg Med. 2017; 70:446-448. https://pubmed.ncbi.nlm.nih.gov/28844277
84. American College of Emergency Physicians. Sub-Dissociative ketamine for analgesia policy resource and education paper. From the ACEP website. https://www.acep.org/globalassets/new-pdfs/preps/prep---sub-dissociative-dose-ketamine-for-analgesia-120717.pdf
85. Schwartzman RJ, Alexander GM, Grothusen JR et al. Outpatient intravenous ketamine for the treatment of complex regional pain syndrome: a double-blind placebo controlled study. Pain. 2009; 147:107-15. https://pubmed.ncbi.nlm.nih.gov/19783371
86. Eide PK, Stubhaug A, Stenehjem AE. Central dysesthesia pain after traumatic spinal cord injury is dependent on N-methyl-D-aspartate receptor activation. Neurosurgery. 1995; 37:1080-7. https://pubmed.ncbi.nlm.nih.gov/8584148
87. Kvarnström A, Karlsten R, Quiding H et al. The analgesic effect of intravenous ketamine and lidocaine on pain after spinal cord injury. Acta Anaesthesiol Scand. 2004; 48:498-506. https://pubmed.ncbi.nlm.nih.gov/15025615
88. Hampton JP. Rapid-sequence intubation and the role of the emergency department pharmacist. Am J Health Syst Pharm. 2011; 68:1320-30. https://pubmed.ncbi.nlm.nih.gov/21719592
89. Godwin SA, Burton JH, Gerardo CJ et al. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2014; 63:247-58.e18. https://pubmed.ncbi.nlm.nih.gov/24438649
90. McEvoy GK, ed. Handbook on injectable drugs. 20th ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2018:698-700
91. Kaplan JA, Cooperman LH. Alarming reactions to ketamine in patients taking thyroid medication--treatment with propranolol. Anesthesiology. 1971; 35:229-30. https://pubmed.ncbi.nlm.nih.gov/5568143
92. Johnstone M. The cardiovascular effects of ketamine in man. Anaesthesia. 1976; 31:873-82. https://pubmed.ncbi.nlm.nih.gov/970587
93. Dunlop L. Ondansetron use in paediatric ketamine sedation. BestBETS: Best evidence topics. 6 June 2018. From BestBETS website. https://bestbets.org/bets/bet.php?id=3009
94. Bhatt M, Johnson DW, Chan J et al. Risk Factors for Adverse Events in Emergency Department Procedural Sedation for Children. JAMA Pediatr. 2017; 171:957-964. https://pubmed.ncbi.nlm.nih.gov/28828486
95. Langston WT, Wathen JE, Roback MG et al. Effect of ondansetron on the incidence of vomiting associated with ketamine sedation in children: a double-blind, randomized, placebo-controlled trial. Ann Emerg Med. 2008; 52:30-4. https://pubmed.ncbi.nlm.nih.gov/18353503
96. Lee JS, Jeon WC, Park EJ et al. Does ondansetron have an effect on intramuscular ketamine-associated vomiting in children? A prospective, randomised, open, controlled study. J Paediatr Child Health. 2014; 50:557-61. https://pubmed.ncbi.nlm.nih.gov/24612260
97. Honarmand A, Safavi M, Kashefi P et al. Comparison of effect of intravenous ketamine, peritonsillar infiltration of tramadol and their combination on pediatric posttonsillectomy pain: A double-blinded randomized placebo-controlled clinical trial. Res Pharm Sci. 2013; 8:177-83. https://pubmed.ncbi.nlm.nih.gov/24019827
98. DA Conceição MJ, Bruggemann DA Conceição D, Carneiro Leão C. Effect of an intravenous single dose of ketamine on postoperative pain in tonsillectomy patients. Paediatr Anaesth. 2006; 16:962-7. https://pubmed.ncbi.nlm.nih.gov/16918659
99. Kimiaei Asadi H, Nikooseresht M, Noori L et al. The Effect of Administration of Ketamine and Paracetamol Versus Paracetamol Singly on Postoperative Pain, Nausea and Vomiting After Pediatric Adenotonsillectomy. Anesth Pain Med. 2016; 6:e31210. https://pubmed.ncbi.nlm.nih.gov/27110529
100. Elshammaa N, Chidambaran V, Housny W et al. Ketamine as an adjunct to fentanyl improves postoperative analgesia and hastens discharge in children following tonsillectomy - a prospective, double-blinded, randomized study. Paediatr Anaesth. 2011; 21:1009-14. https://pubmed.ncbi.nlm.nih.gov/21575100
101. Pestieau SR, Finkel JC, Junqueira MM et al. Prolonged perioperative infusion of low-dose ketamine does not alter opioid use after pediatric scoliosis surgery. Paediatr Anaesth. 2014; 24:582-90. https://pubmed.ncbi.nlm.nih.gov/24809838
102. Yenigun A, Et T, Aytac S et al. Comparison of different administration of ketamine and intravenous tramadol hydrochloride for postoperative pain relief and sedation after pediatric tonsillectomy. J Craniofac Surg. 2015; 26:e21-4. https://pubmed.ncbi.nlm.nih.gov/25569408
103. Javid MJ, Hajijafari M, Hajipour A et al. Evaluation of a low dose ketamine in post tonsillectomy pain relief: a randomized trial comparing intravenous and subcutaneous ketamine in pediatrics. Anesth Pain Med. 2012; 2:85-9. https://pubmed.ncbi.nlm.nih.gov/24223344
104. Foy G, Poinsignon V, Mercier L et al. Microbiological and physico-chemical stability of ketamine solution for patient-controlled analgesia systems. Research & Reviews: Journal of Hospital and Clinical Pharmacy. 2015; 1:31-7.
105. Schmid R, Koren G, Klein J et al. The stability of a ketamine-morphine solution. Anesth Analg. 2002; 94:898-900, table of contents. https://pubmed.ncbi.nlm.nih.gov/11916793
106. Green SM, Rothrock SG, Lynch EL, et al. Intramuscular ketamine for pediatric sedation in the emergency department: safety profile in 1,022 cases. Ann Emerg Med. 1998;31(6):688-697. https://pubmed.ncbi.nlm.nih.gov/9624307
107. Grunwell JR, Travers C, Stormorken AG, et al. Pediatric Procedural Sedation Using the Combination of Ketamine and Propofol Outside of the Emergency Department: A Report From the Pediatric Sedation Research Consortium. Pediatr Crit Care Med. 2017;18(8):e356-e363. https://pubmed.ncbi.nlm.nih.gov/28650904
108. Ferguson I, Bell A, Treston G et al. Propofol or Ketofol for Procedural Sedation and Analgesia in Emergency Medicine-The POKER Study: A Randomized Double-Blind Clinical Trial. Ann Emerg Med. 2016;68(5):574-582.e1. https://pubmed.ncbi.nlm.nih.gov/27460905
109. Grunwell JR, Travers C, McCracken CE, et al. Procedural Sedation Outside of the Operating Room Using Ketamine in 22,645 Children: A Report From the Pediatric Sedation Research Consortium. Pediatr Crit Care Med. 2016;17(12):1109-1116. https://pubmed.ncbi.nlm.nih.gov/27505716
110. Umunna BP, Tekwani K, Barounis D et al. Ketamine for continuous sedation of mechanically ventilated patients. J Emerg Trauma Shock. 2015;8(1):11-15. https://pubmed.ncbi.nlm.nih.gov/25709246
111. Vincent JL, Shehabi Y, Walsh TS, et al. Comfort and patient-centred care without excessive sedation: the eCASH concept. Intensive Care Med. 2016;42(6):962-971. https://pubmed.ncbi.nlm.nih.gov/27075762
112. Heiberger AL, Ngorsuraches S, Olgun G, et al. Safety and utility of continuous ketamine infusion for sedation in mechanically ventilated pediatric patients. J Pediatr Pharmacol Ther. 2018;23(6):447-454. https://pubmed.ncbi.nlm.nih.gov/30697129
113. Park S, Choi AY, Park E, et al. Effects of continuous ketamine infusion on hemodynamics and mortality in critically ill children. PLoS One. 2019;14(10):e0224035. Published 2019 Oct 18. https://pubmed.ncbi.nlm.nih.gov/31626685
114. Garber PM, Droege CA, Carter KE et al. Continuous Infusion Ketamine for Adjunctive Analgosedation in Mechanically Ventilated, Critically Ill Patients. Pharmacotherapy. 2019;39(3):288-296. https://pubmed.ncbi.nlm.nih.gov/30746728
115. Pruskowski KA, Harbourt K, Pajoumand M et al. Impact of Ketamine Use on Adjunctive Analgesic and Sedative Medications in Critically Ill Trauma Patients. Pharmacotherapy. 2017;37(12):1537-1544. https://pubmed.ncbi.nlm.nih.gov/29023898
116. Chan K, Burry LD, Tse C, et al. Impact of Ketamine on Analgosedative Consumption in Critically Ill Patients: A Systematic Review and Meta-Analysis. Ann Pharmacother. 2022 Jan 26;10600280211069617.
117. Manasco AT, Stephens RJ, Yaeger LH, et al. Ketamine sedation in mechanically ventilated patients: A systematic review and meta-analysis. J Crit Care. 2020 Apr;56:80-88.
214. American College of Emergency Physicians. Policy statement: Procedural sedation in the emergency department. Approved June 2017. From the ACEP website. https://www.acep.org/globalassets/new-pdfs/policy-statements/procedural.sedation.in.the.ed.pdf
249. ASHP. Standardize 4 Safety: pediatric continuous infusion standards. Updated Mar 2024. From ASHP website. Updates may be available at ASHP website. https://www.www.ashp.org/pharmacy-practice/standardize-4-safety-initiative
250. ASHP. Standardize 4 Safety: adult continuous infusion standards. Updated Mar 2024. From ASHP website. Updates may be available at ASHP website. https://www.www.ashp.org/pharmacy-practice/standardize-4-safety-initiative
251. ASHP. Standardize 4 Safety: patient controlled analgesia (PCA) and epidural standards. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.www.ashp.org/pharmacy-practice/standardize-4-safety-initiative
300. Wan LB, Levitch CF, Perez AM et al. Ketamine safety and tolerability in clinical trials for treatment-resistant depression. J Clin Psychiatry. 2015; 76:247-52. https://pubmed.ncbi.nlm.nih.gov/25271445
301. Feifel D, Malcolm B, Boggie D et al. Low-dose ketamine for treatment resistant depression in an academic clinical practice setting. J Affect Dis. 2017; 221:283-8. https://pubmed.ncbi.nlm.nih.gov/28666206
302. Sanacora G, Frye MA, McDonald W et al. A Consensus Statement on the Use of Ketamine in the Treatment of Mood Disorders. JAMA Psychiatry. 2017; 74:399-405. https://pubmed.ncbi.nlm.nih.gov/28249076
303. Iadarola ND, Niciu MJ, Richards EM et al. Ketamine and other N-methyl-D-aspartate receptor antagonists in the treatment of depression: a perspective review. Ther Adv Chronic Dis. 2015; 6:97-114. https://pubmed.ncbi.nlm.nih.gov/25954495
304. Berman RM, Cappiello A, Anand A et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000; 47:351-4. https://pubmed.ncbi.nlm.nih.gov/10686270
305. Lapidus KAB, Levitch CF, Perez AM et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. 2014; 76:970-6. https://pubmed.ncbi.nlm.nih.gov/24821196
306. Rasmussen KG, Lineberry TW, Galardy CW et al. Serial infusions of low-dose ketamine for major depression. J Psychopharmacol. 2013; 27:444-50. https://pubmed.ncbi.nlm.nih.gov/23428794
307. Murrough JW, Perez AM, Pillemer S et al. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatry. 2013; 74:250-6. https://pubmed.ncbi.nlm.nih.gov/22840761
308. Kellner CH, Greenberg RM, Ahle GM et al. Electroconvulsive therapy is a standard treatment; ketamine is not (yet). Am J Psychiatry. 2014; 171:796. https://pubmed.ncbi.nlm.nih.gov/24980176
309. Hu YD, Xiang YT, Fang JX et al. Single i.v. ketamine augmentation of newly initiated escitalopram for major depression: results from a randomized, placebo-controlled 4-week study. Psychol Med. 2016; 46:623-35. https://pubmed.ncbi.nlm.nih.gov/26478208
310. Wilkinson ST, Ballard ED, Bloch MH et al. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry. 2018; 175:150-8. https://pubmed.ncbi.nlm.nih.gov/28969441
311. Arabzadeh S, Hakkikazazi E, Shahmansouri N et al. Does oral administration of ketamine accelerate response to treatment in major depressive disorder? Results of a double-blind controlled trial. J Affect Disord. 2018; 235:236-41. https://pubmed.ncbi.nlm.nih.gov/29660637
312. aan het Rot M, Collins KA, Murrough JW et al. Safety and efficacy of repeated-dose intravenous ketamine for treatment-related depression. Biol Psychiatry. 2010; 67:139-45. https://pubmed.ncbi.nlm.nih.gov/19897179
313. Vande Voort JL, Morgan RJ, Kung S et al. Continuation phase intravenous ketamine in adults with treatment-resistant depression.. J Affect Disord. 2016; 206:300-4. https://pubmed.ncbi.nlm.nih.gov/27656788
314. Bobo WV, Vande Voort JL, Croarkin PE et al. Ketamine for treatment-resistant unipolar and bipolar major depressions: critical review and implications for clinical practice. Depress Anxiety. 2016; 33:698-710. https://pubmed.ncbi.nlm.nih.gov/27062450
315. Shiroma PR, Johns B, Kuskowski M et al. Augmentation of response and remission to serial intravenous subanesthetic ketamine in treatment resistant depression. J Affect Disord. 2014; 155:123-9. https://pubmed.ncbi.nlm.nih.gov/24268616
316. Schak KM, Vande Voort JL, Johnson EK et al. Potential risks of poorly monitored ketamine use in depression treatment. Am J Psychiatry. 2016; 173:215-8. https://pubmed.ncbi.nlm.nih.gov/26926127
317. Rasmussen KG. Has psychiatry tamed the “ketamine tiger?” Considerations on its use for depression and anxiety. Prog Neuropsychopharmacol Biol Psychiatry. 2016; 64:218-24. https://pubmed.ncbi.nlm.nih.gov/25582770
318. Ford N, Ludbrook G, Galletly C. Benzodiazepines may reduce the effectiveness of ketamine in the treatment of depression. Aust N Z J Psychiatry. 2015; 49:12. https://pubmed.ncbi.nlm.nih.gov/26058787
319. Hashimoto K. The R-Stereoisomer of Ketamine as an Alternative for Ketamine for Treatment-resistant Major Depression. Clin Psychopharmacol Neurosci. 2014; 12:72-3. https://pubmed.ncbi.nlm.nih.gov/24851126
320. Newport DJ, Carpenter LL, McDonald WM et al. Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression. Am J Psychiatry. 2015; 172:950-66. https://pubmed.ncbi.nlm.nih.gov/26423481
321. Abdallah CG, Adams TG, Kelmendi B et al. Ketamine's mechanism of action: a path to rapid-acting antidepressants. Depress Anxiety. 2016; 33:689-97. https://pubmed.ncbi.nlm.nih.gov/27062302
322. Ionescu DF, Bentley KH, Eikermann M et al. Repeat-dose ketamine augmentation for treatment-resistant depression with chronic suicidal ideation: a randomized, double blind, placebo controlled trial. J Affect Disord. 2019; 243:516-24. https://pubmed.ncbi.nlm.nih.gov/30286416
323. Ionescu DF, Swee MB, Pavone KJ et al. Rapid and Sustained Reductions in Current Suicidal Ideation Following Repeated Doses of Intravenous Ketamine: Secondary Analysis of an Open-Label Study. J Clin Psychiatry. 2016; 77:e719-25. https://pubmed.ncbi.nlm.nih.gov/27232360
324. Reinstatler L, Youssef NA. Ketamine as a potential treatment for suicidal ideation: a systematic review of the literature. Drugs RD. 2015; 15:37-43. https://pubmed.ncbi.nlm.nih.gov/25773961
325. Andrade C. Ketamine for Depression, 6: Effects on Suicidal Ideation and Possible Use as Crisis Intervention in Patients at Suicide Risk. J Clin Psychiatry. 2018; 79:18f12242. https://pubmed.ncbi.nlm.nih.gov/29659211
326. Grunebaum MF, Galfalvy HC, Choo TH. Ketamine for Rapid Reduction of Suicidal Thoughts in Major Depression: A Midazolam-Controlled Randomized Clinical Trial. Am J Psychiatry. 2018; 175:327-35. https://pubmed.ncbi.nlm.nih.gov/29202655
327. Wilkinson ST, Katz RB, Toprak M et al. Acute and Longer-Term Outcomes Using Ketamine as a Clinical Treatment at the Yale Psychiatric Hospital. J Clin Psychiatry. 2018; 79:17m11731. https://pubmed.ncbi.nlm.nih.gov/30063304
328. Frye MA, Blier P, Tye SJ. Concomitant benzodiazepine use attenuates ketamine response: implications for large scale study design and clinical development. J Clin Psychopharmacol. 2015; 35:334-336. https://pubmed.ncbi.nlm.nih.gov/25928701
329. Janssen Pharmaceuticals Inc.. Spravato (esketamine hydrochloride) nasal spray prescribing information. 2019 Mar. http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d81a6a79-a74a-44b7-822c-0dfa3036eaed
750. US Food and Drug Administration. Drug safety communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. Silver Spring, MD; 2016 Dec 14. From FDA website. https://www.fda.gov/Drugs/DrugSafety/ucm532356.htm
751. Davidson AJ, Disma N, de Graaff JC et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016; 387:239-50. https://pubmed.ncbi.nlm.nih.gov/26507180
752. Sun LS, Li G, Miller TL et al. Association Between a Single General Anesthesia Exposure Before Age 36 Months and Neurocognitive Outcomes in Later Childhood. JAMA. 2016; 315:2312-20. https://pubmed.ncbi.nlm.nih.gov/27272582
753. US Food and Drug Administration. Drug safety communication: FDA approves labeling changes for use of general anesthetic and sedation drugs in young children. Silver Spring, MD; 2017 Apr 27. From FDA website. https://www.fda.gov/Drugs/DrugSafety/ucm554634.htm
754. McCann ME, de Graaff JC, Dorris L, et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomised, controlled equivalence trial. Lancet. 2019;393:664-77. https://pubmed.ncbi.nlm.nih.gov/30782342
800. Devlin JW, Skrobik Y, Gélinas C et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. 2018; 46:e825-e873. https://pubmed.ncbi.nlm.nih.gov/30113379
821. Godwin SA, Caro DA, Wolf SJ et al. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2005; 45:177-96. https://pubmed.ncbi.nlm.nih.gov/15671976
823. . Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018: A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018; 128:437-479. https://pubmed.ncbi.nlm.nih.gov/29334501
824. American Society of Anesthesiologists. Continuum of depth of sedation: definition of general anesthesia and levels of sedation/analgesia. Last amended Oct 23, 2019. From the ASA website. https://www.asahq.org/
825. .US Food and Drug Administration. FDA warns patients and health care providers about potential risks associated with compounded ketamine products, including oral formulations, for the treatment of psychiatric disorders (October 10, 2023). From FDA website https://www.fda.gov/drugs/human-drug-compounding/fda-warns-patients-and-health-care-providers-about-potential-risks-associated-compounded-ketamine. https://www.asahq.org/
Related/similar drugs
Frequently asked questions
More about ketamine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (168)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: general anesthetics
- Breastfeeding
- En español