Cefixime (Monograph)
Brand name: Suprax
Drug class: Third Generation Cephalosporins
Introduction
Antibacterial; β-lactam antibiotic; third generation cephalosporin.
Uses for Cefixime
Urinary Tract Infections
Treatment of adults and pediatric patients ≥6 months of age with uncomplicated UTIs caused by susceptible E. coli or Proteus mirabilis; also has been used for treatment of uncomplicated UTIs caused by susceptible Citrobacter spp.† [off-label], C. diversus† [off-label], C. freundii† [off-label], Enterobacter spp.† [off-label], E. aerogenes† [off-label], E. agglomerans†, Klebsiella spp.†, K. pneumoniae†, Morganella morganii†, Proteus spp.†, or Serratia†.
Has been used for treatment of uncomplicated UTIs caused by susceptible gram-positive bacteria, including Staphylococcus epidermidis†, Staphylococcus spp.†, Streptococcus agalactiae†, nonhemolytic streptococci†, or Enterococcus faecalis†. Consider that treatment failures have been reported and gram-positive bacteria (e.g., staphylococci, S. agalactiae, enterococci) have been isolated in urine during or after cefixime treatment and usually are resistant to cefixime.
Treatment of pyelonephritis† and other complicated UTIs† caused by susceptible Enterobacteriaceae, including E. coli.
Otitis Media
Treatment of adults and pediatric patients ≥6 months of age with otitis media caused by Haemophilus influenzae, Moraxella catarrhalis, or Streptococcus pyogenes (group A β-hemolytic streptococci). Has also been used for the treatment of otitis media caused by S. pneumoniae; however, overall response was approximately 10% lower for cefixime than for the comparator in clinical studies.
When anti-infectives indicated, AAP recommends high-dose amoxicillin or amoxicillin and clavulanate as drugs of choice for initial treatment of otitis media; certain cephalosporins (cefdinir, cefpodoxime, cefuroxime, ceftriaxone) recommended as alternatives for initial treatment in penicillin-allergic patients without a history of severe and/or recent penicillin-allergic reactions.
Pharyngitis and Tonsillitis
Treatment of adults and pediatric patients ≥6 months of age with pharyngitis and tonsillitis caused by susceptible S. pyogenes (group A β-hemolytic streptococci). Generally effective in eradicating S. pyogenes from nasopharynx; efficacy in prevention of subsequent rheumatic fever not established to date.
AAP, IDSA, AHA, and others recommend a penicillin regimen (10 days of oral penicillin V or oral amoxicillin or single dose of IM penicillin G benzathine) as treatment of choice for S. pyogenes pharyngitis and tonsillitis; other anti-infectives (oral cephalosporins, oral macrolides, oral clindamycin) recommended as alternatives in penicillin-allergic patients.
If an oral cephalosporin is used, 10-day regimen of first generation cephalosporin (cefadroxil, cephalexin) is preferred instead of other cephalosporins with broader spectrums of activity (e.g., cefaclor, cefdinir, cefixime, cefpodoxime, cefuroxime).
Acute Exacerbations of Chronic Bronchitis
Treatment of adults and pediatric patients ≥6 months of age with acute exacerbations of chronic bronchitis caused by S. pneumoniae, H. influenzae, or M. catarrhalis†.
Gonorrhea
Treatment of adults and pediatric patients ≥6 months of age with uncomplicated urethral, endocervical, or rectal infections† caused by susceptible Neisseria gonorrhoeae.
Because of concerns related to reports of N. gonorrhoeae with reduced susceptibility to cephalosporins, CDC states that oral cephalosporins no longer recommended as first-line treatment for uncomplicated gonorrhea. For treatment of uncomplicated urogenital, anorectal, or pharyngeal gonorrhea, CDC recommends a single dose of IM ceftriaxone. Add treatment for chlamydia if not excluded.
Cefixime recommended by CDC as an alternative in patients with urogenital or rectal† gonorrhea when ceftriaxone cannot be used or not available. Add treatment for chlamydia if not excluded.
Consider that N. gonorrhoeae with reduced susceptibility to cefixime, including some treatment failures, reported in US and other countries.
If infection persists (treatment failure), culture relevant clinical specimens and perform in vitro susceptibility tests. Also consult infectious disease specialist, STD/HIV Prevention Training Center ([Web]), or CDC (800-232-4636) for treatment advice and report the case to CDC through local or state health departments within 24 hours of diagnosis.
For all gonorrhea patients, ensure that their sex partners from preceding 60 days are evaluated promptly with culture and receive presumptive treatment with a recommended regimen.
Pneumonia
Has been used in adults or children for the treatment of mild to moderate pneumonia, including community-acquired pneumonia†. When used in hospitalized patients with community-acquired pneumonia, therapy was initiated with a parenteral third generation cephalosporin (e.g., ceftriaxone, cefotaxime) and then changed to oral cefixime, as appropriate, allowing therapy to be completed on an outpatient basis.
Other cephalosporins (e.g., ceftriaxone, cefotaxime, ceftaroline, ceftazidime, cefpodoxime, cefuroxime) are recommended by the American Thoracic Society/IDSA and others when a cephalosporin is used in the treatment of community-acquired pneumonia.
Lyme Disease
Has been used for treatment of disseminated Lyme disease†. Other cephalosporins (cefotaxime, ceftriaxone, cefuroxime axetil) usually recommended by IDSA, AAP, and others when a cephalosporin is used in the treatment of Lyme disease.
Shigellosis
Has been used for treatment of shigellosis† caused by susceptible Shigella; however, other drugs are listed as a first-line or alternative agents in IDSA and AAP guidelines.
Sinusitis
Has been used for the treatment of mild to moderate sinusitis† caused by S. pneumoniae, H. influenzae M. catarrhalis E. coli, H. parahaemolyticus, or H. parainfluenzae Because of variable activity against S. pneumoniae and H. influenzae, IDSA no longer recommends second or third generation oral cephalosporins for empiric monotherapy of acute bacterial sinusitis. Oral amoxicillin or amoxicillin and clavulanate usually recommended for empiric treatment. If an oral cephalosporin used as an alternative in children (e.g., in penicillin-allergic individuals), combination regimen that includes a third generation cephalosporin (cefixime or cefpodoxime) and clindamycin (or linezolid) recommended.
Typhoid Fever and Other Salmonella Infections
Has been used in pediatric patients for the treatment of typhoid fever (enteric fever) or septicemia caused by multidrug-resistant strains of Salmonella typhi†.
Multidrug-resistant strains of S.typhi (i.e., strains resistant to ampicillin, chloramphenicol, and/or co-trimoxazole) reported with increasing frequency; fluoroquinolones (e.g., ciprofloxacin, ofloxacin) and third generation cephalosporins (e.g., ceftriaxone, cefotaxime) have been considered agents of first choice for treatment of typhoid fever or other severe infections known or suspected to be caused by these strains.
Fluoroquinolones no longer recommended as empiric treatment for typhoid fever infections in US. Ceftriaxone considered a drug of choice for empiric treatment of enteric fever pending results of in vitro susceptibility tests. Consider travel history and regional antibiotic resistance patterns when selecting empiric antibiotic therapy for enteric fever; adjust treatment based on results of susceptibility testing.
Cefixime Dosage and Administration
General
Pretreatment Screening
-
Prior to initiation of therapy, careful inquiry should be made concerning previous hypersensitivity reactions to cephalosporins, penicillins, other β-lactam anti-infectives, or other drugs.
Patient Monitoring
-
Monitor patients for hypersensitivity reactions. If a severe hypersensitivity reaction occurs, immediately discontinue cefixime and institute appropriate therapy as indicated.
-
Carefully monitor patients receiving dialysis during treatment with cefixime.
-
Monitor prothrombin time in patients with impaired vitamin K synthesis or low vitamin K stores (e.g., chronic hepatic disease, malnutrition). Administer vitamin K when indicated.
Other General Considerations
-
To reduce the development of drug-resistant bacteria and maintain effectiveness of cefixime and other antibacterials, use cefixime only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
Administration
Oral Administration
Administer orally as capsules, conventional tablets, chewable tablets, or oral suspension.
Capsules and conventional tablets: Administer without regard to meals.
Chewable tablets: Must be chewed or crushed before swallowing.
Reconstitution
Reconstitute oral suspension at the time of dispensing by adding amount of water specified on the container in 2 equal portions; shake after each addition. The reconstituted suspension contains 100, 200, or 500 mg/5 mL.
Shake oral suspension well just prior to administration of each dose.
Dosage
Available as cefixime trihydrate; dosage expressed in terms of cefixime.
Capsules containing 400 mg of cefixime are bioequivalent to conventional 400-mg tablets when administered under fasting conditions.
Chewable tablets are bioequivalent to oral suspension.
Conventional tablets and oral suspension are not bioequivalent.
Pediatric Patients
General Pediatric Dosage
Oral
Children beyond neonatal period: AAP recommends 8 mg/kg daily in 1 or 2 equally divided doses for treatment of mild or moderate infections. AAP states the drug is inappropriate for treatment of severe infections.
Children weighing 5–7.5 kg: Oral suspension containing 100 mg/5 mL is preferred preparation.
Children weighing 7.6–10 kg: Oral suspension containing 100 or 200 mg/5 mL is preferred preparation.
Children weighing <10 kg: Chewable tablets not recommended.
Urinary Tract Infections (UTIs)
Uncomplicated UTIs
OralChildren 6 months to 12 years of age: 8 mg/kg once daily or 4 mg/kg every 12 hours for 5–10 days.
Children >12 years of age or weighing >45 kg: 400 mg once daily or 200 mg every 12 hours for 5–10 days.
Otitis Media
Oral
Children 6 months to 12 years of age: 8 mg/kg once daily or 4 mg/kg every 12 hours for 10–14 days.
Children >12 years of age or weighing >45 kg: 400 mg daily for 10–14 days.
Do not use capsules or conventional tablets for treatment of otitis media.
Pharyngitis and Tonsillitis
Oral
Children 6 months to 12 years of age: 8 mg/kg once daily or 4 mg/kg every 12 hours for ≥10 days.
Children >12 years of age or weighing >45 kg: 400 mg once daily or 200 mg every 12 hours for ≥10 days.
Acute Exacerbations of Chronic Bronchitis
Oral
Children 6 months to 12 years of age: 8 mg/kg once daily or 4 mg/kg every 12 hours for 10–14 days.
Children >12 years of age or weighing >45 kg: 400 mg once daily or 200 mg every 12 hours for 10–14 days.
Gonorrhea and Associated Infections
Uncomplicated Urethral, Endocervical, or Rectal† Gonorrhea
OralIn pediatric patients or adolescents weighing ≥45 kg when ceftriaxone is unavailable or cannot be used, CDC and AAP recommend a single oral cefixime dose of 800 mg.
Prepubertal children ≥6 months of age weighing <45 kg: 8 mg/kg recommended by manufacturer.
Children ≥12 years of age or weighing ≥45 kg: 400 mg as a single dose recommended by manufacturer.
Not recommended by CDC as first-line treatment. If chlamydia not excluded, also treat patient for chlamydia.
Shigellosis†
Oral
8 mg/kg daily for 5 days.
Acute Treatment of Acute Bacterial Sinusitis†
Oral
8 mg/kg daily in 2 equally divided doses for 10–14 days.
Typhoid Fever†
Oral
Children 6 months to 16 years of age: 5–10 mg/kg twice daily. Usually given for 14 days; high rate of treatment failure occurred when given for only 7 days.
Adults
Urinary Tract Infections (UTIs)
Uncomplicated UTIs
Oral400 mg once daily or 200 mg every 12 hours for 5–10 days.
Otitis Media
Oral
400 mg once daily or 200 mg every 12 hours for 10–14 days.
Do not use capsules or conventional tablets for treatment of otitis media.
Pharyngitis and Tonsillitis
Oral
400 mg once daily or 200 mg every 12 hours for ≥10 days.
Acute Exacerbations of Chronic Bronchitis
Oral
400 mg once daily or 200 mg every 12 hours for 10–14 days.
Gonorrhea and Associated Infections
Uncomplicated Urethral, Endocervical, or Rectal† Gonorrhea
Oral800 mg as a single dose recommended by CDC as alternative when ceftriaxone unavailable or cannot be used.
Use in conjunction with treatment for chlamydia if chlamydia not ruled out. Not recommended by CDC as first-line treatment.
Manufacturer recommends a single 400-mg dose of cefixime for treatment of uncomplicated cervical/urethral gonococcal infections.
Lyme Disease†
Oral
200 mg daily for 100 days (administered with oral probenecid).
Special Populations
Renal Impairment
Dosage adjustments necessary in patients with Clcr <60 mL/minute. Adults with Clcr 21–59 mL/minute: 260 mg daily as oral suspension, preferably as oral suspension containing 200 or 500 mg/5 mL; conventional tablets and chewable tablets not recommended.
Adults with Clcr ≤20 mL/minute: 200 mg daily as conventional tablets or chewable tablets, 172 mg daily as oral suspension containing 100 mg/5 mL, 176 mg daily as oral suspension containing 200 mg/5 mL, or 180 mg daily as oral suspension containing 500 mg/5 mL.
Adults undergoing hemodialysis: 260 mg daily as oral suspension, preferably as oral suspension containing 200 or 500 mg/5 mL; conventional tablets and chewable tablets not recommended.
Adults undergoing continuous peritoneal dialysis: 200 mg daily as conventional tablets or chewable tablets, 172 mg daily as oral suspension containing 100 mg/5 mL, 176 mg daily as oral suspension containing 200 mg/5 mL, or 180 mg daily as oral suspension containing 500 mg/5 mL.
Hepatic Impairment
The manufacturer makes no specific dosage recommendations for patients with hepatic impairment.
Geriatric Patients
No dosage adjustments except those related to renal impairment.
Cautions for Cefixime
Contraindications
-
Known hypersensitivity to cefixime or other cephalosporins.
Warnings/Precautions
Hypersensitivity Reactions
Hypersensitivity reactions such as anaphylaxis (including shock and fatalities), angioedema, serum sickness-like reactions, Stevens-Johnson syndrome, and toxic epidermal necrolysis have been reported.
If an allergic reaction occurs, discontinue cefixime.
Partial cross-allergenicity among cephalosporins and other β-lactam antibiotics, including penicillins and cephamycins. Use caution.
Prior to initiation of therapy, make careful inquiry concerning previous hypersensitivity reactions to cephalosporins, penicillins, or other drugs. Cefixime is contraindicated in individuals hypersensitive to cephalosporins. Avoid use in those who have had an immediate-type (anaphylactic) hypersensitivity reaction and administer with caution in those who have had a delayed-type (e.g., rash, fever, eosinophilia) reaction.
Clostridioides difficile-associated Diarrhea
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridioides difficile. C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including cefixime, and may range in severity from mild diarrhea to fatal colitis. C. difficile produces toxins A and B which contribute to development of CDAD; hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.
Consider CDAD if diarrhea develops during or after therapy and manage accordingly. Obtain careful medical history since CDAD may occur as late as 2 months or longer after anti-infective therapy is discontinued.
If CDAD is suspected or confirmed, discontinue anti-infectives not directed against C. difficile whenever possible. Initiate appropriate supportive therapy (e.g., fluid and electrolyte management, protein supplementation), anti-infective therapy directed against C. difficile (e.g., metronidazole, vancomycin), and surgical evaluation as clinically indicated.
Dose Adjustment in Renal Impairment
Serum concentrations of cefixime higher and more prolonged in patients with moderate or severe renal impairment than in patients with normal renal function; decrease dose and/or frequency of administration of cefixime in patients with impaired renal function, including those undergoing continuous ambulatory peritoneal dialysis (CAPD) or hemodialysis. Carefully monitor patients undergoing dialysis during cefixime therapy.
Coagulation Effects
Prolonged PT reported.
Patients with renal or hepatic impairment, poor nutritional status, prolonged anti-infective therapy, and previous anticoagulant therapy (stabilized) appear to be at risk. Monitor PT in such patients and administer exogenous vitamin K as indicated.
Development of Drug-resistant Bacteria
To reduce development of drug-resistant bacteria and maintain effectiveness of cefixime and other antibacterials, the drug should be used only for the treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria. When selecting or modifying anti-infective therapy, results of culture and in vitro susceptibility testing should be used. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Patients with Phenylketonuria
Chewable tablets containing 100, 150, and 200 mg of cefixime contain aspartame , which is metabolized in the GI tract to provide 3.3, 5, and 6.7 mg of phenylalanine, respectively. Phenylalanine can be harmful to patients with phenylketonuria; consider combined daily amount of phenylalanine from all sources before prescribing cefixime chewable tablets in such patients.
Specific Populations
Pregnancy
No adequate and controlled studies to date using cefixime in pregnant women; use drug during pregnancy only when clearly needed. Use of drug during labor and delivery also not studied to date; use in these circumstances only when clearly needed.
Lactation
Distributed into milk in rats; not known whether distributed into milk in humans. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <6 months of age. Frequency of adverse GI effects (e.g., diarrhea, loose stools) similar to that in adults.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Possible increased oral bioavailability; not considered clinically important.
Consider age-related decreases in renal function when selecting dosage and adjust dosage if necessary.
Hepatic Impairment
There is no evidence of metabolism of cefixime in vivo. Hepatic impairment is not expected to affect clearance of cefixime.
Renal Impairment
Increased serum half-life in patients with moderate or severe renal impairment. Dosage adjustments necessary if Clcr <60 mL/minute.
Common Adverse Effects
Diarrhea (16%), nausea (7%), loose stools (6%), abdominal pain (3%), dyspepsia (3%), vomiting.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
No clinically important effect on cefixime pharmacokinetics |
|
|
Anticoagulants, oral (warfarin) |
Possible increased PT (with or without bleeding) |
|
|
Carbamazepine |
Increased carbamazepine concentrations |
Monitor carbamazepine concentrations |
|
Coomb's test |
Possible false positive Coomb's test results with cephalosporins |
|
|
Nifedipine |
Possible increased plasma concentrations and AUC of cefixime |
|
|
Probenecid |
Increased cefixime plasma concentrations and AUC |
|
|
Salicylates |
Possible decreased plasma concentrations and AUC of cefixime |
Clinical importance unclear |
|
Tests for glucose |
Possible false-positive reactions in urine glucose tests using Clinitest, Benedict’s solution, or Fehling’s solution |
Use glucose tests based on enzymatic glucose oxidase reactions (e.g., Clinistix, Tes-Tape) |
|
Tests for ketones |
Possible false-positive reaction for ketones in urine if nitroprusside tests used; not reported with tests using nitroferricyanide |
Cefixime Pharmacokinetics
Absorption
Bioavailability
30–50% of a single oral dose absorbed; peak serum concentrations attained within 2–6 hours.
Capsules containing 400 mg of cefixime are bioequivalent to conventional tablets containing 400 mg of the drug when administered under fasting conditions.
Chewable tablets are bioequivalent to the oral suspension.
Conventional tablets and oral suspension are not bioequivalent; studies in adults indicate oral suspension results in peak serum concentrations and AUC 25–50% and 10–25% higher, respectively, than those attained with tablets.
Food
Conventional tablets and oral suspension: Food decreases rate but not extent of absorption.
Capsules: Food decreases absorption by about 15% (based on AUC) or 25% (based on peak serum concentrations).
Distribution
Extent
Distributed into bile, sputum, tonsils, maxillary sinus mucosa, middle ear discharge, blister fluid, and prostatic fluid.
Distribution into CSF unknown.
Crosses the placenta. Not detected in human milk following a single 100-mg oral dose.
Plasma Protein Binding
65–70%.
Elimination
Metabolism
Does not appear to be metabolized; no biologically active metabolites detected in serum or urine.
Elimination Route
Eliminated by renal and nonrenal mechanisms.
7–50% of a dose excreted unchanged in urine within 24 hours. In animal studies, >10% of a dose may be excreted unchanged in bile.
Not substantially removed by hemodialysis or peritoneal dialysis.
Half-life
Adults with normal renal function: 2.4–4 hours.
Special Populations
Adults with moderate renal impairment (Clcr 20–40 mL/minute): Serum half-life averages 6.4 hours.
Adults with severe renal impairment (Clcr 5–20 mL/minute): Serum half-life averages 11.5 hours.
Geriatric patients: AUC at steady state approximately 40% higher than in younger adults; not considered clinically important.
Stability
Storage
Oral
Capsules, Conventional Tablets, Chewable Tablets
20–25°C.
For Suspension
20–25°C. After reconstitution, store suspension in tight container at room temperature or in the refrigerator; discard after 14 days.
Actions and Spectrum
-
Based on spectrum of activity, classified as a third generation cephalosporin. Expanded spectrum of activity against gram-negative bacteria compared with first and second generation cephalosporins; less active against Enterobacteriaceae than some other third-generation cephalosporins.
-
Usually bactericidal.
-
Like other β-lactam antibiotics, antibacterial activity results from inhibition of bacterial cell wall synthesis.
-
Spectrum of activity includes many gram-positive and gram-negative aerobic bacteria; inactive against most anaerobic bacteria.
-
Gram-positive aerobes: Active in vitro against Streptococcus pneumoniae and Streptococcus pyogenes (group A β-hemolytic streptococci). Also active in vitro against S. agalactiae (group B streptococci) and groups C, F, and G streptococci. Most staphylococci, enterococci, and Listeria monocytogenes are resistant.
-
Strains of staphylococci resistant to penicillinase-resistant penicillins (methicillin-resistant [oxacillin-resistant] staphylococci) should be considered resistant to cefixime, although results of in vitro susceptibility tests may indicate susceptibility.
-
Gram-negative aerobes: Active in vitro against Neisseria gonorrhoeae, Haemophilus influenzae (including β-lactamase-producing strains), Moraxella catarrhalis (including β-lactamase-producing strains), Escherichia coli, and Proteus mirabilis. Also active in vitro against Citrobacter amalonaticus, C. diversus, H. parainfluenzae, Klebsiella, Pasteurella multocida, P. vulgaris, Providencia, Salmonella, Shigella, and Serratia. Most Enterobacter and Pseudomonas are resistant.
Advice to Patients
-
Advise patients that antibacterials (including cefixime) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Importance of completing full course of therapy, even if feeling better after a few days.
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with cefixime or other antibacterials in the future.
-
Advise patients that diarrhea is a common problem caused by anti-infectives and usually ends when the drug is discontinued. Importance of contacting a clinician if watery and bloody stools (with or without stomach cramps and fever) occur during or as late as 2 months or longer after the last dose.
-
Importance of discontinuing cefixime and informing clinician if an allergic reaction occurs.
-
Advise patients with phenylketonuria that cefixime chewable tablets containing 100, 150, and 200 mg of the drug contain aspartame, which is metabolized in the GI tract to provide 3.3, 5, and 6.7 mg of phenylalanine, respectively.
-
Importance of women informing clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
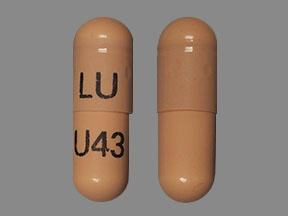
Oral |
Capsules |
400 mg (of cefixime) |
Suprax |
Lupin |
|
For suspension |
100 mg (of cefixime) per 5 mL |
Suprax |
Lupin |
|
|
200 mg (of cefixime) per 5 mL |
Suprax |
Lupin |
||
|
500 mg (of cefixime) per 5 mL |
Suprax |
Lupin |
||
|
Tablets, chewable |
100 mg (of cefixime) |
Suprax |
Lupin |
|
|
150 mg (of cefixime) |
Suprax |
Lupin |
||
|
200 mg (of cefixime) |
Suprax |
Lupin |
||
|
Tablets, film-coated |
400 mg (of cefixime) |
Suprax (scored) |
Lupin |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about cefixime
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (27)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: third generation cephalosporins
- Breastfeeding
- En español