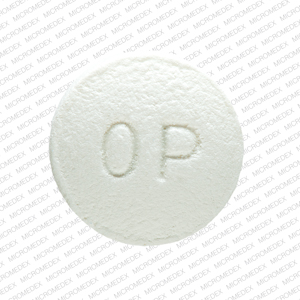
OxyContin Dosage
Generic name: OXYCODONE HYDROCHLORIDE 80mg
Dosage form: tablet, film coated, extended release
Drug class: Opioids (narcotic analgesics)
Medically reviewed by Drugs.com. Last updated on Dec 5, 2024.
Important Dosage and Administration Instructions
- OXYCONTIN should be prescribed only by healthcare professionals who are knowledgeable about the use of extended-release/long-acting opioids and how to mitigate the associated risks.
- OXYCONTIN 60 mg and 80 mg tablets, a single dose greater than 40 mg, or a total daily dose greater than 80 mg are only for use in patients in whom tolerance to an opioid of comparable potency has been established. Adult patients who are opioid tolerant are those receiving, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, 60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid.
- Use the lowest effective dosage for the shortest duration of time consistent with individual patient treatment goals. Because the risk of overdose increases as opioid doses increase, reserve titration to higher doses of OXYCONTIN for patients in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks.
- Initiate the dosing regimen for each patient individually, taking into account the patient's underlying cause and severity of pain, prior analgesic treatment and response, and risk factors for addiction, abuse, and misuse.
- Respiratory depression can occur at any time during opioid therapy, especially when initiating and following dosage increases with OXYCONTIN. Consider this risk when selecting an initial dose and when making dose adjustments.
- Instruct patients to swallow OXYCONTIN tablets whole, one tablet at a time, with enough water to ensure complete swallowing immediately after placing in the mouth. Instruct patients not to pre-soak, lick, or otherwise wet the tablet prior to placing in the mouth. Cutting, breaking, crushing, chewing, or dissolving OXYCONTIN tablets will result in uncontrolled delivery of oxycodone and can lead to overdose or death.
- OXYCONTIN is administered orally every 12 hours.
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with OXYCONTIN.
Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program).
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient.
Consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose.
Initial Dosage in Adults who are not Opioid-Tolerant
The starting dosage for patients who are not opioid tolerant is OXYCONTIN 10 mg orally every 12 hours.
Use of higher starting doses in patients who are not opioid tolerant may cause fatal respiratory depression.
Conversion from Opioids to OXYCONTIN in Adults
Conversion from Other Oral Oxycodone Formulations to OXYCONTIN
If switching from other oral oxycodone formulations to OXYCONTIN, administer one half of the patient's total daily oral oxycodone dose as OXYCONTIN every 12 hours.
Conversion from Other Opioids to OXYCONTIN
When OXYCONTIN therapy is initiated, discontinue all other opioid analgesics other than those used on an as needed basis for breakthrough pain when appropriate.
There are no established conversion ratios for conversion from other opioids to OXYCONTIN defined by clinical trials. Initiate dosing using OXYCONTIN 10 mg orally every 12 hours.
It is safer to underestimate a patient's 24-hour oral oxycodone requirements and provide rescue medication (e.g., immediate-release opioid) than to overestimate the 24-hour oral oxycodone dosage and manage an adverse reaction due to an overdose. While useful tables of opioid equivalents are readily available, there is substantial inter-patient variability in the relative potency of different opioids.
Close observation and frequent titration are warranted until pain management is stable on the new opioid. Monitor patients for signs and symptoms of opioid withdrawal and for signs of oversedation/toxicity after converting patients to OXYCONTIN.
Conversion from Methadone to OXYCONTIN
Regular evaluation is of particular importance when converting from methadone to other opioid agonists. The ratio between methadone and other opioid agonists may vary widely as a function of previous dose exposure. Methadone has a long half-life and can accumulate in the plasma.
Conversion from Transdermal Fentanyl to OXYCONTIN
Treatment with OXYCONTIN can be initiated after the transdermal fentanyl patch has been removed for at least 18 hours. Although there has been no systematic assessment of such conversion, start with a conservative conversion: substitute 10 mg of OXYCONTIN every 12 hours for each 25 mcg per hour fentanyl transdermal patch. Follow the patient closely during conversion from transdermal fentanyl to OXYCONTIN, as there is limited documented experience with this conversion.
Initial Dosage in Pediatric Patients 11 Years and Older
The following dosing information is for use only in pediatric patients 11 years and older already receiving and tolerating opioids for at least five consecutive days. For the two days immediately preceding dosing with OXYCONTIN, patients must be taking a minimum of 20 mg per day of oxycodone or its equivalent. OXYCONTIN is not appropriate for use in pediatric patients requiring less than a 20 mg total daily dose. Table 1, based on clinical trial experience, displays the conversion factor when switching pediatric patients 11 years and older (under the conditions described above) from opioids to OXYCONTIN.
When OXYCONTIN therapy is initiated, discontinue all other opioid analgesics other than those used on an as needed basis for breakthrough pain when appropriate.
There is substantial inter-patient variability in the relative potency of different opioid drugs and formulations. Therefore, a conservative approach is advised when determining the total daily dosage of OXYCONTIN. It is safer to underestimate a patient's 24-hour oral oxycodone requirements and provide rescue medication (e.g., immediate-release opioid) than to overestimate the 24-hour oral oxycodone requirements and manage an adverse reaction due to an overdose.
Consider the following when using the information in Table 1.
- This is not a table of equianalgesic doses.
- The conversion factors in this table are only for the conversion from one of the listed oral opioid analgesics to OXYCONTIN.
- The table cannot be used to convert from OXYCONTIN to another opioid. Doing so will result in an over-estimation of the dose of the new opioid and may result in fatal overdose.
- The formula for conversion from prior opioids, including oral oxycodone, to the daily dose of OXYCONTIN is mg per day of prior opioid x factor = mg per day of OXYCONTIN. Divide the calculated total daily dose by 2 to get the every-12-hour OXYCONTIN dose. If rounding is necessary, always round the dose down to the nearest OXYCONTIN tablet strength available.
| *For patients receiving high-dose parenteral opioids, a more conservative conversion is warranted. For example, for high-dose parenteral morphine, use 1.5 instead of 3 as a multiplication factor. | ||
| Prior Opioid | Conversion Factor | |
| Oral | Parenteral* | |
| Oxycodone | 1 | -- |
| Hydrocodone | 0.9 | -- |
| Hydromorphone | 4 | 20 |
| Morphine | 0.5 | 3 |
| Tramadol | 0.17 | 0.2 |
Step #1: To calculate the estimated total OXYCONTIN daily dosage using Table 1:
- For pediatric patients taking a single opioid, sum the current total daily dosage of the opioid and then multiply the total daily dosage by the approximate conversion factor to calculate the approximate OXYCONTIN daily dosage.
- For pediatric patients on a regimen of more than one opioid, calculate the approximate oxycodone dose for each opioid and sum the totals to obtain the approximate OXYCONTIN daily dosage.
- For pediatric patients on a regimen of fixed-ratio opioid/non-opioid analgesic products, use only the opioid component of these products in the conversion.
Step #2: If rounding is necessary, always round the dosage down to the nearest OXYCONTIN tablet strength available and initiate OXYCONTIN therapy with that dose. If the calculated OXYCONTIN total daily dosage is less than 20 mg, there is no safe strength for conversion and do not initiate OXYCONTIN.
Example conversion from a single opioid (e.g., hydrocodone) to OXYCONTIN: Using the conversion factor of 0.9 for oral hydrocodone in Table 1, a total daily hydrocodone dosage of 50 mg is converted to 45 mg of oxycodone per day or 22.5 mg of OXYCONTIN every 12 hours. After rounding down to the nearest strength available, the recommended OXYCONTIN starting dosage is 20 mg every 12 hours.
Step #3: Close observation and titration are warranted until pain management is stable on the new opioid. Monitor patients for signs and symptoms of opioid withdrawal or for signs of over-sedation/toxicity after converting patients to OXYCONTIN. for important instructions on titration and maintenance of therapy.
There is limited experience with conversion from transdermal fentanyl to OXYCONTIN in pediatric patients 11 years and older. If switching from transdermal fentanyl patch to OXYCONTIN, ensure that the patch has been removed for at least 18 hours prior to starting OXYCONTIN. Although there has been no systematic assessment of such conversion, start with a conservative conversion: substitute 10 mg of OXYCONTIN every 12 hours for each 25 mcg per hour fentanyl transdermal patch. Follow the patient closely during conversion from transdermal fentanyl to OXYCONTIN.
If using asymmetric dosing, instruct patients to take the higher dose in the morning and the lower dose in the evening.
Titration and Maintenance of Therapy in Adults and Pediatric Patients 11 Years and Older
Individually titrate OXYCONTIN to a dosage that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving OXYCONTIN to assess the maintenance of pain control, signs and symptoms of opioid withdrawal, and other adverse reactions, as well as to reassess for the development of addiction, abuse and misuse. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During use of opioid therapy for an extended period of time, periodically reassess the continued need for the use of opioid analgesics.
Patients who experience breakthrough pain may require a dosage adjustment of OXYCONTIN or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dose stabilization, attempt to identify the source of increased pain before increasing the OXYCONTIN dosage. Because steady-state plasma concentrations are approximated in 1 day, OXYCONTIN dosage may be adjusted every 1 to 2 days.
If after increasing the dosage, unacceptable opioid-related adverse reactions are observed (including an increase in pain after a dosage increase), consider reducing the dosage. Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
There are no well-controlled clinical studies evaluating the safety and efficacy with dosing more frequently than every 12 hours. As a guideline for pediatric patients 11 years and older, the total daily oxycodone dosage usually can be increased by 25% of the current total daily dosage. As a guideline for adults, the total daily oxycodone dosage usually can be increased by 25% to 50% of the current total daily dosage, each time an increase is clinically indicated.
Dosage Modifications with Concomitant Use of Central Nervous System Depressants
If the patient is currently taking a central nervous system (CNS) depressant and the decision is made to begin OXYCONTIN, start with one-third to one-half the recommended starting dosage of OXYCONTIN, consider using a lower dosage of the concomitant CNS depressant, and regularly evaluate patients for signs of respiratory depression, sedation, and hypotension.
Dosage Modifications in Geriatric Patients who are Debilitated and not Opioid-Tolerant
For geriatric patients who are debilitated and not opioid tolerant, start dosing patients at one-third to one-half the recommended starting dosage and titrate the dosage cautiously. Regularly evaluate for signs of respiratory depression, sedation, and hypotension.
Dosage Modifications in Patients with Hepatic Impairment
For patients with hepatic impairment, start dosing patients at one-third to one-half the recommended starting dosage and titrate the dosage carefully. Regularly evaluate for signs of respiratory depression, sedation, and hypotension.
Safe Reduction or Discontinuation of OXYCONTIN
Do not abruptly discontinue OXYCONTIN in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking OXYCONTIN, there are a variety of factors that should be considered, including the total daily dose of opioid (including OXYCONTIN) the patient has been taking, the duration of treatment, the type of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with comorbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patient-specific plan to taper the dose of the opioid gradually. For patients on OXYCONTIN who are physically opioid-dependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, evaluate patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for an extended period of time and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic.
Frequently asked questions
- Oxycodone vs Hydrocodone vs OTC Pain Relievers
- Which drugs cause opioid-induced constipation?
- Oxycodone vs OxyContin - What's the difference?
- How long does oxycodone take to work?
- What are the withdrawal symptoms of oxycodone?
- What is Hydrochloride or HCL in a drugname?
- How addictive is OxyContin (oxycodone)?
- How long does oxycodone stay in your system?
More about OxyContin (oxycodone)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (295)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: Opioids (narcotic analgesics)
- Breastfeeding
- En español
Patient resources
Other brands
Roxicodone, Xtampza ER, OxyIR, Oxaydo, ... +7 more
Professional resources
Other brands
Roxicodone, Xtampza ER, Oxaydo, RoxyBond
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.