Polythiazide/prazosin Disease Interactions
There are 13 disease interactions with polythiazide / prazosin.
- Anuria
- Electrolyte losses
- Liver disease
- Lupus erythematosus
- Renal function disorders
- Hypotension
- Liver disease
- Asthma
- Diabetes
- Hyperlipidemia
- Hyperparathyroidism
- Hyperuricemia
- Thyroid function tests
Thiazides (applies to polythiazide/prazosin) anuria
Major Potential Hazard, High plausibility.
The use of thiazide diuretics is contraindicated in patients with anuria.
Thiazides (applies to polythiazide/prazosin) electrolyte losses
Major Potential Hazard, High plausibility. Applicable conditions: Diarrhea, Hypokalemia, Hyponatremia, Magnesium Imbalance, Malnourished, Vomiting, Electrolyte Abnormalities, Hyperaldosteronism, Ventricular Arrhythmia, Dehydration
The use of thiazide diuretics is commonly associated with loss of electrolytes, most significantly potassium but also sodium, chloride, bicarbonate, and magnesium. The loss of other electrolytes such as phosphate, bromide and iodide is usually slight. Potassium and magnesium depletion may lead to cardiac arrhythmias and cardiac arrest. Other electrolyte-related complications include metabolic alkalosis and hyponatremia, which are rarely life-threatening. Therapy with thiazide diuretics should be administered cautiously in patients with or predisposed to fluid and electrolyte depletion, including patients with primary or secondary aldosteronism (may have low potassium levels); those with severe or prolonged diarrhea or vomiting; and those with poor nutritional status. Fluid and electrolyte abnormalities should be corrected prior to initiating therapy, and blood pressure as well as serum electrolyte concentrations monitored periodically and maintained at normal ranges during therapy. Patients should be advised to immediately report signs and symptoms of fluid or electrolyte imbalance, including dry mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, arrhythmia, or gastrointestinal disturbances such as nausea and vomiting. Digitalized patients and patients with a history of ventricular arrhythmias should be monitored carefully, since development of hypokalemia may be particularly dangerous in these patients. The risk of hypokalemia may be minimized by slow diuresis, a lower thiazide dosage, potassium supplementation, or combined use with a potassium-sparing diuretic.
Thiazides (applies to polythiazide/prazosin) liver disease
Major Potential Hazard, High plausibility.
Patients with severe liver disease or cirrhosis are very susceptible to thiazide-induced hypokalemic hypochloremic alkalosis. Blood ammonia concentrations may be further increased in patients with previously elevated concentrations. Hepatic encephalopathy and death have occurred secondary to the electrolyte alterations accompanying diuretic use. Therapy with thiazide diuretics should be administered cautiously in patients with impaired hepatic function or progressive liver disease, and discontinued promptly if signs of impending hepatic coma appear (e.g., tremors, confusion, and increased jaundice).
Thiazides (applies to polythiazide/prazosin) lupus erythematosus
Major Potential Hazard, Low plausibility.
The use of thiazide diuretics has been reported to possibly exacerbate or activate systemic lupus erythematosus. Reported cases have generally been associated with chlorothiazide and hydrochlorothiazide. Therapy with thiazide diuretics should be administered cautiously in patients with a history or risk of SLE.
Thiazides (applies to polythiazide/prazosin) renal function disorders
Major Potential Hazard, High plausibility. Applicable conditions: Renal Dysfunction
Thiazide diuretics may be ineffective when the glomerular filtration rate is low (GFR < 25 mL/min) because they are not expected to be filtered into the renal tubule, their site of action. In addition, thiazide diuretics decrease the GFR and may precipitate azotemia in renal disease. Cumulative effects may also develop because most of these drugs are excreted unchanged in the urine by glomerular filtration and active tubular secretion. Therapy with thiazide diuretics should be administered cautiously at reduced dosages in patients with renal impairment. If renal function becomes progressively worse, as indicated by rising BUN or serum creatinine levels, an interruption or discontinuation of thiazide therapy should be considered.
Alpha-1 blockers (applies to polythiazide/prazosin) hypotension
Moderate Potential Hazard, High plausibility. Applicable conditions: Syncope, Autonomic Neuropathy, Dehydration, Diarrhea, Vomiting
Peripheral alpha 1- adrenergic receptor blocking agents (aka alpha 1- blockers) cause vasodilation and can produce marked hypotension, especially orthostatic hypotension with syncope or other postural symptoms such as dizziness, lightheadedness, and palpitations. Orthostatic effects are most common during initiation of therapy and often occur within 90 minutes after the first dose. However, they can also occur following a dosage increase or resumption of therapy after an interruption of more than a few days. Agents with alpha 1a specificity, such as tamsulosin, act primarily on the prostate but are not devoid of hypotensive effects. Therapy with peripheral alpha-1 blockers should be administered cautiously in patients with or predisposed to hypotensive or syncopal episodes. Caution is also advised in patients who are dehydrated (e.g., due to severe or prolonged diarrhea or vomiting), since they may be more sensitive to the hypotensive effect of the drugs. Therapy should be initiated with the lowest dosage possible and titrated gradually based on patient response and tolerance in accordance with the individual product package labeling. During initiation or reinstitution of therapy and following an increase in dosage, patients should be advised not to rise abruptly from a sitting or recumbent position and to avoid situations where injury could result if syncope occur. Concomitant use of alcohol, extensive periods of standing, prolonged or intense exercise, and exposure to heat can also precipitate orthostatic hypotension and should be minimized. If dizziness, lightheadedness or palpitations occur, the patient should sit or lie down, and seek medical attention if symptoms are recurrent or bothersome.
Prazosin (applies to polythiazide/prazosin) liver disease
Moderate Potential Hazard, High plausibility. Applicable conditions: Biliary Obstruction
Little data exist concerning the pharmacokinetic disposition of prazosin in patients with liver disease. Prazosin is known to be metabolized by the liver and subsequently excreted in the bile, primarily as metabolites. Some of the metabolites are pharmacologically active and possess 10% to 25% of the hypotensive activity of prazosin. Therapy with prazosin should be administered cautiously in patients with significantly impaired hepatic or biliary function, since drug and/or metabolite accumulation may occur.
Thiazides (applies to polythiazide/prazosin) asthma
Moderate Potential Hazard, Moderate plausibility.
Thiazide diuretics should be used with caution in patients with history of bronchial asthma as sensitivity reactions may occur.
Thiazides (applies to polythiazide/prazosin) diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus, Abnormal Glucose Tolerance
Thiazide diuretics may cause hyperglycemia and glycosuria in patients with diabetes. They may also precipitate diabetes in prediabetic patients. These effects are usually reversible following discontinuation of the drugs. Therapy with thiazide diuretics should be administered cautiously in patients with diabetes mellitus, glucose intolerance, or a predisposition to hyperglycemia. Patients with diabetes mellitus should be monitored more closely during thiazide therapy, and their antidiabetic regimen adjusted accordingly.
Thiazides (applies to polythiazide/prazosin) hyperlipidemia
Moderate Potential Hazard, Moderate plausibility.
Thiazide diuretics may increase serum triglyceride and cholesterol levels, primarily LDL and VLDL. Whether these effects are dose-related and sustained during chronic therapy are unknown. Patients with preexisting hyperlipidemia may require closer monitoring during thiazide therapy, and adjustments made accordingly in their lipid-lowering regimen
Thiazides (applies to polythiazide/prazosin) hyperparathyroidism
Moderate Potential Hazard, Moderate plausibility.
Urinary calcium excretion is decreased by thiazide diuretics during chronic administration. Pathologic changes in the parathyroid gland with hypercalcemia and hypophosphatemia have been reported during prolonged therapy. However, the common complications of hyperparathyroidism such as renal lithiasis, bone resorption, and peptic ulceration have not been seen. Clinicians should be cognizant of these effects when prescribing or administering thiazide therapy to patients with hyperparathyroidism. These drugs should be discontinued before carrying out tests for parathyroid function.
Thiazides (applies to polythiazide/prazosin) hyperuricemia
Moderate Potential Hazard, High plausibility. Applicable conditions: Gout
Thiazide diuretics decrease the rate of uric acid excretion. Hyperuricemia occurs frequently but is usually asymptomatic and rarely leads to clinical gout except in patients with a history of gout or chronic renal failure. Therapy with thiazide diuretics should be administered cautiously in such patients.
Thiazides (applies to polythiazide/prazosin) thyroid function tests
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Thyroid Disease
Thiazide diuretics may decrease serum PBI (protein-bound iodine) levels without associated thyroid disturbance. Clinicians should be cognizant of this effect when prescribing or administering thiazide therapy to patients with thyroid disorders.
Switch to professional interaction data
Polythiazide/prazosin drug interactions
There are 511 drug interactions with polythiazide / prazosin.
Polythiazide/prazosin alcohol/food interactions
There are 2 alcohol/food interactions with polythiazide / prazosin.
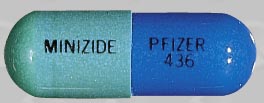
More about polythiazide / prazosin
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiadrenergic agents (peripheral) with thiazides
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.