Milk Allergy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
A milk allergy is a condition that develops because your child's immune system overreacts to milk proteins. Your child's immune system sees the proteins as harmful and attacks them. Milk allergies are most common during the first year of a child's life. Your child may outgrow the allergy by 18 months to 5 years of age. Less commonly, the allergy may continue to adolescence. Rarely, a milk allergy can continue into adulthood.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for signs or symptoms of anaphylaxis,
such as trouble breathing, swelling in your child's mouth or throat, or wheezing. Your child may also have itching, a rash, hives, or feel faint.
Return to the emergency department if:
- Your child has itching or hives that spread all over the body.
- Your child's skin or nails are blue or pale.
- Your child has bloody diarrhea.
Call your child's doctor if:
- Your child has new or worsening rashes, hives, or itching.
- Your child has an upset stomach or is vomiting.
- Your child has stomach cramps or diarrhea.
- You have questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- Epinephrine is used to treat severe allergic reactions such as anaphylaxis.
- Antihistamines decrease mild symptoms such as itching or a rash.
- Steroids may be given to decrease inflammation.
- Short-acting bronchodilators help open your airways quickly. These medicines relieve sudden, severe symptoms and start to work right away. They may be called rescue inhalers or relievers.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Steps to take for signs or symptoms of anaphylaxis:
Your child's healthcare provider will tell you if your child is at risk for anaphylaxis. The provider will prescribe a medicine called epinephrine to use at the first sign of anaphylaxis. Signs include trouble breathing, swelling in your child's mouth or throat, or wheezing.
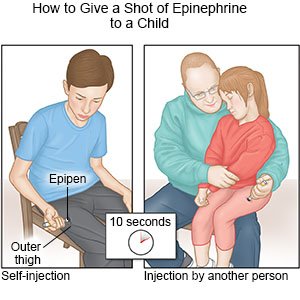
- Immediately give 1 shot of epinephrine only into the outer thigh muscle. Hold the shot in place for up to 10 seconds before you remove it. This helps make sure all of the epinephrine is delivered.
- Call 911 and go to the emergency department, even if the shot improved symptoms. Bring the used epinephrine shot with you.
Foods your child needs to avoid:
Even a small taste of a milk product can cause an allergic reaction. Do not let your child have any of the following:
- Cow's milk, goat's milk, or sheep's milk
- Cheese, cottage cheese, powdered milk, or butter
- Sour cream, yogurt, or buttermilk
- Ice cream, whipped cream, or half-and-half
- Pudding, custard, or milk chocolate
- Microwave or movie popcorn that contains diacetyl for butter flavor
- Soy products, if your child is also allergic to soy
Manage or prevent a milk allergy:
- Read all food labels. Read the label each time you buy the food to make sure the ingredients have not changed. Look for milk protein in the list of ingredients. Milk protein may be listed as casein or whey. Also check for diacetyl, ghee, lactose, lactalbumin, lactoglobulin, lactoferrin, and tagatose. Ask your child's healthcare provider for a complete list of ingredients to check for when you buy packaged foods.
- Talk to servers or managers at restaurants when you eat out. Tell the server or manager about the milk allergy before you order. Ask about ingredients in the dish you want to order for your child. Ask if milk is added to sauces or soups. Ask for food to be prepared without butter or sour cream.
- Prevent cross-contamination. Do not use kitchen items that have touched milk products. For example, do not use a knife to cut a food after it touched a milk product. This is called cross-contamination, and it can still cause an allergic reaction. Keep all utensils, cutting boards, and dishes that touched milk separate from other equipment. Use hot, soapy water to wash all kitchen items that touch food. Wash items after each time they touch food as you cook.
- Breastfeed your baby for the first year. Breast milk is the best food for your baby. Breastfeeding can help prevent allergies, and can help your baby's immune system develop. If possible, give your baby only breast milk for the first 4 to 6 months.
Safety precautions to take if your child is at risk for anaphylaxis:
- Tell others about your child's allergy. Tell family members, friends, and your child's school officials, teachers, and babysitters. Your child's school or daycare center can help make sure your child is not exposed to milk protein. This includes making sure your child does not eat baked foods brought into the classroom to celebrate a holiday or birthday. Ask if your child should carry epinephrine at all times. Some schools keep epinephrine in a medical office. Make sure others know what to do in case of an anaphylactic reaction.
- Keep 2 shots of epinephrine available for your child at all times. Your child may need a second shot if the first dose does not help or if your child's symptoms return. Your child's healthcare provider can show you and family members how to give the shot. Check the expiration date every month and replace it before it expires.
- Create an action plan. Your child's healthcare provider can help you create a written plan that explains the allergy and an emergency plan to treat a reaction. The plan explains when to give a second epinephrine shot if symptoms return or do not improve after the first. Give copies of the action plan and emergency instructions to family members, school and sports staff, and daycare providers. Show them how to give a shot of epinephrine. Update the plan as the allergy changes.
- Tell your child to be careful with exercise. If your child had exercise-induced anaphylaxis, exercise should not happen right after a meal. Your child must stop exercising right away if any signs or symptoms of anaphylaxis develop. Your child may first feel tired, warm, or have itchy skin. Hives, swelling, and severe breathing problems may develop if your child continues to exercise.
- Have your child carry medical alert identification. Have your child wear jewelry or carry a card that describes the milk allergy. Ask your child's provider where to get these items.

- Help your child be safe with food and eating utensils. Do not let your child share utensils or food. Wash your child's hands before and after meals.

Follow up with your child's doctor as directed:
Your child may need to see specialists for ongoing care. Your child's healthcare provider may want to test your child regularly to see if the milk allergy changes. Write down your questions so you remember to ask them during follow-up visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Milk Allergy
- Allergies, Cough/Cold Medications & Alcohol Interactions
- Benadryl Dosage Charts for Infants and Children
- Claritin Dosage Charts for Infants and Children
- EpiPen Costs and Alternatives: What Are Your Best Options?
- Low Salicylate Diet
- Zyrtec Dosage Charts for Infants and Children
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
