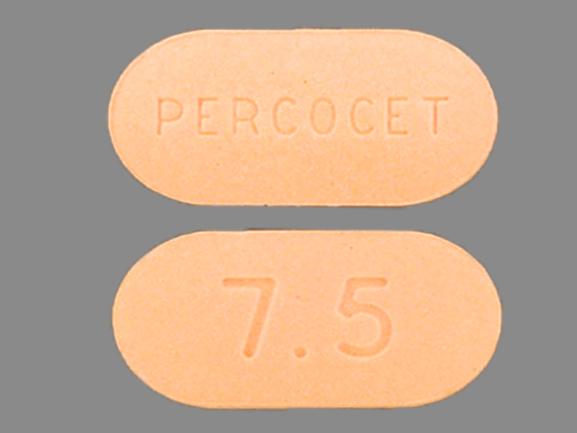
Percocet 7.5/500 Side Effects
Generic name: acetaminophen / oxycodone
Medically reviewed by Drugs.com. Last updated on Sep 1, 2025.
Note: This document provides detailed information about Percocet 7.5/500 Side Effects associated with acetaminophen / oxycodone. Some dosage forms listed on this page may not apply specifically to the brand name Percocet 7.5/500.
Applies to acetaminophen / oxycodone: oral solution, oral tablet.
Important warnings
This medicine can cause some serious health issues
Precautions
It is very important that your doctor check your progress while you are taking this medicine, especially within the first 24 to 72 hours of treatment. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for unwanted effects.
It is against the law and dangerous for anyone else to use your medicine. Keep your unused medicine in a safe and secure place. People who are addicted to drugs might want to steal it.
Check with your doctor before using this medicine with alcohol or other medicines that affect the central nervous system (CNS). This medicine will add to the effects of alcohol and other CNS depressants (medicines that can make you drowsy or less alert). Some examples of CNS depressants are antihistamines or medicine for allergies or colds, sedatives, tranquilizers, or sleeping medicine, other prescription pain medicine or narcotics, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics. Also, there may be a greater risk of liver damage if you drink three or more alcoholic beverages while you are taking acetaminophen. Do not drink alcoholic beverages.
If you think you or someone else may have taken an overdose of this medicine, get emergency help at once. Your doctor may also give naloxone to treat an overdose. Signs of an overdose include: extreme dizziness or weakness, slow heartbeat or breathing, seizures, trouble breathing, and cold, clammy skin. Call your doctor right away if you notice these symptoms.
This medicine may be habit-forming. If you feel that the medicine is not working as well, do not use more than your prescribed dose. Call your doctor for instructions.
Do not use this medicine if you are using or have used an MAO inhibitor (eg, isocarboxazid [Marplan®], linezolid [Zyvox®], phenelzine [Nardil®], selegiline [Eldepryl®], tranylcypromine [Parnate®]) within the past 14 days. Using these medicine together may cause serious unwanted effects.
This medicine may cause sleep-related breathing problems (eg, sleep apnea, sleep-related hypoxemia). Your doctor may decrease your dose if you have sleep apnea (stop breathing for short periods during sleep) while using this medicine.
Dizziness, lightheadedness, or fainting may occur when you get up suddenly from a lying or sitting position. Getting up slowly may help lessen this problem. Also, lying down for a while may relieve the dizziness or lightheadedness.
This medicine may make you dizzy, drowsy, or lightheaded. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
Check with your doctor right away if you have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
Serious skin reactions (eg, acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, and toxic epidermal necrolysis) can occur with this medicine. Check with your doctor right away if you have blistering, peeling, or loosening of the skin, chills, cough, diarrhea, itching, joint or muscle pain red irritated eyes, red skin lesions, often with a purple center, sore throat, sores, ulcers, or white spots in the mouth or on the lips, or unusual tiredness or weakness while you are using this medicine.
This medicine may cause serious allergic reactions, including anaphylaxis, which can be life-threatening and requires immediate medical attention. Call your doctor right away if you have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth while you are using this medicine.
Using narcotics for a long time can cause severe constipation. To prevent this, your doctor may direct you to take laxatives, drink a lot of fluids, or increase the amount of fiber in your diet. Be sure to follow the directions carefully, because continuing constipation can lead to more serious problems.
If you have been using this medicine regularly for several weeks or longer, do not change your dose or suddenly stop using it without checking with your doctor. Your doctor may want you to gradually reduce the amount you are using before stopping it completely. This may help prevent worsening of your condition and reduce the possibility of withdrawal symptoms, including stomach cramps, anxiety, fever, irritability, nausea, restlessness, runny nose, sweating, tremors, or trouble with sleeping.
Using this medicine while you are pregnant may cause serious unwanted effects, including neonatal withdrawal syndrome in your newborn baby. Tell your doctor right away if you think you are pregnant or if you plan to become pregnant while using this medicine.
For nursing mothers:
- Talk to your doctor if you have any questions about taking oxycodone or about how this medicine may affect your baby.
- Call your doctor if you become extremely tired and have difficulty caring for your baby.
- Your baby should generally nurse every 2 to 3 hours and should not sleep for more than 4 hours at a time.
- Check with your doctor or hospital emergency room immediately if your baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, difficulty breathing, or limpness. These may be symptoms of an overdose and need immediate medical attention.
Before you have any medical tests, tell the medical doctor in charge that you are taking this medicine. The results of some tests may be affected by this medicine.
Check with your doctor right away if you have anxiety, restlessness, a fast heartbeat, fever, sweating, muscle spasms, twitching, nausea, vomiting, diarrhea, or see or hear things that are not there. These may be symptoms of a serious condition called serotonin syndrome. Your risk may be higher if you also take certain other medicines that affect serotonin levels in your body.
Using too much of this medicine may cause infertility (unable to have children). Talk with your doctor before using this medicine if you plan to have children.
This medicine may cause adrenal gland problems. Check with your doctor right away if you have darkening of the skin, diarrhea, dizziness, fainting, loss of appetite, mental depression, nausea, skin rash, unusual tiredness or weakness, or vomiting.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of Percocet 7.5/500
Along with its needed effects, acetaminophen / oxycodone may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking acetaminophen / oxycodone:
More common side effects
- black, tarry stools
- chills
- dark urine
- dizziness
- fever
- headache
- itching, skin rash
- light-colored stools
- loss of appetite
- nausea
- stomach pain
- unpleasant breath odor
- unusual tiredness or weakness
- vomiting of blood
- yellow eyes or skin
Rare side effects
- cough
- fever with or without chills
- general feeling of tiredness or weakness
- hoarseness
- lower back or side pain
- painful or difficult urination
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- unusual bleeding or bruising
Incidence not known
- back, leg, or stomach pains
- bleeding gums
- bloating
- blood in the urine or stools
- blue lips and fingernails
- blurred vision
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- chest pain, discomfort, or tightness
- cloudy urine
- clumsiness
- confusion
- constipation
- coughing that sometimes produces a pink frothy sputum
- darkening of the skin
- decreased awareness or responsiveness
- decreased frequency or amount of urine
- diarrhea
- difficult, fast, noisy breathing
- difficulty in passing urine (dribbling)
- difficulty with swallowing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- drowsiness
- dry mouth
- extremely shallow or slow breathing
- fainting
- fast or deep breathing
- fast, slow, irregular, pounding, or racing heartbeat
- feeling of warmth
- general body swelling
- hives or welts
- increased sweating
- increased thirst
- indigestion
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- lightheadedness
- mental depression
- muscle aches, tremors, or weakness
- nervousness
- nosebleeds
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pale skin
- pinpoint red spots on the skin
- pounding in the ears
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid, deep or shallow breathing
- redness of the face, neck, arms, and occasionally, upper chest
- restlessness
- seizures
- severe constipation
- severe sleepiness
- severe vomiting
- skin blisters
- sleepiness
- stomach cramps
- sunken eyes
- sweating
- swelling of the face, fingers, lower legs, or ankles
- thirst
- tiredness
- trouble breathing
- vomiting
- weakness or heaviness of the legs
- weight gain
Get emergency help immediately if any of the following symptoms of overdose occur while taking acetaminophen / oxycodone:
Symptoms of overdose
- bluish lips or skin
- change in consciousness
- cold, clammy skin
- extreme sleepiness
- general feeling of discomfort or illness
- loss of consciousness
- low blood pressure or pulse
- slow breathing
- unconsciousness
Other side effects of Percocet 7.5/500
Some side effects of acetaminophen / oxycodone may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- relaxed and calm feeling
Incidence not known
- agitation
- bad, unusual or unpleasant (after) taste
- belching
- change in taste
- cold sweats
- constricted, pinpoint, or small pupils (black part of the eye)
- continuing ringing or buzzing or other unexplained noise in the ears
- cool, pale skin
- depression
- difficulty with moving
- disturbed color perception
- double vision
- excess air or gas in the stomach or bowels
- false or unusual sense of well-being
- flushed, dry skin
- fruit-like breath odor
- full feeling
- general feeling of discomfort or illness
- halos around lights
- hearing loss
- heartburn
- increased hunger
- increased urination
- indigestion
- joint pain
- lack or loss of strength
- muscle cramps, spasms, pain, or stiffness
- night blindness
- nightmares
- overbright appearance of lights
- seeing, hearing, or feeling things that are not there
- seizures
- shakiness
- slurred speech
- swollen joints
- trouble sleeping
- tunnel vision
- unexplained weight loss
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
See also:
For healthcare professionals
Applies to acetaminophen / oxycodone: oral capsule, oral solution, oral tablet, oral tablet extended release.
General adverse events
The most commonly reported adverse events have included lightheadedness, dizziness, drowsiness, sedation, nausea, and vomiting.[Ref]
Respiratory
- Common (1% to 10%): Cough
- Frequency not reported: Apnea, respiratory arrest, respiratory depression, hiccups
- Postmarketing reports: Bronchospasm, dyspnea, hyperpnea, pulmonary edema, tachypnea, hypoventilation, laryngeal edema[Ref]
Hepatic
Oxycodone-acetaminophen:
- Postmarketing reports: Transient elevations of hepatic enzymes, increased bilirubin, hepatic failure, jaundice, hepatotoxicity, hepatic disorder, hepatitis
Acetaminophen:
- Frequency not reported: Hepatic necrosis[Ref]
At high doses, the most serious acetaminophen related adverse event is a dose-dependent, potentially fatal hepatic necrosis.[Ref]
Hypersensitivity
- Frequency not reported: Skin eruptions, urticaria, erythematous skin reactions
- Postmarketing reports: Anaphylaxis, allergic reaction, angioedema[Ref]
Dermatologic
- Common (1% to 10%): Rash, blister, excoriation, pruritus, erythema
- Frequency not reported: Dermatitis, ecchymosis, hyperhidrosis
- Postmarketing reports: Urticaria, flushing, increased sweating[Ref]
Nervous system
- Very common (10% or more): Dizziness (up to 13%)
- Common (1% to 10%): Headache, somnolence
- Frequency not reported: Lightheadedness, dizziness, drowsiness, sedation, migraine, myoclonus, paresthesia, tremor
- Postmarketing reports: Stupor, cerebral edema, coma, subdural or intracranial hemorrhage, seizures
Opioids:
- Postmarketing reports: Serotonin syndrome[Ref]
Psychiatric
- Frequency not reported: Euphoria, dysphoria, insomnia, altered mood, sleep disorder, withdrawal syndrome
- Postmarketing reports: Agitation, confusion, anxiety, mental impairment, drug dependence, drug abuse, depression, nervousness, hallucination, suicide[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (up to 31%)
- Common (1% to 10%): Vomiting, constipation, dry mouth, dyspepsia, diarrhea
- Frequency not reported: Esophageal spasm, oropharyngeal pain, throat irritation
- Postmarketing reports: Abdominal pain, abdominal distention, flatulence, gastrointestinal disorder, pancreatitis, intestinal obstruction, ileus, thirst[Ref]
Hematologic
Oxycodone-acetaminophen:
- Frequency not reported: Thrombocytopenia, neutropenia, pancytopenia, hemolytic anemia
Acetaminophen:
- Rare (0.01% to 0.1%): Agranulocytosis[Ref]
Renal
- Postmarketing reports: Renal insufficiency and failure[Ref]
Cardiovascular
- Common (1% to 10%): Edema
- Frequency not reported: Hypotension, chest discomfort
- Postmarketing reports: Tachycardia, dysrhythmias, orthostatic hypotension, bradycardia, palpitations, hypertension[Ref]
Metabolic
- Frequency not reported: Decreased appetite
- Postmarketing reports: Hypoglycemia, hyperglycemia, acidosis, alkalosis, hyperkalemia, dehydration
Musculoskeletal
- Postmarketing reports: Rhabdomyolysis, myalgia
Ocular
- Postmarketing reports: Miosis, visual disturbances, red eye
Genitourinary
- Common (1% to 10%): Dysuria
- Frequency not reported: Urinary retention, interstitial nephritis, proteinuria, decreased urine flow
Other
- Postmarketing reports: Malaise, asthenia, fatigue, fever, hypothermia, accidental overdose, non-accidental overdose, hearing loss, tinnitus[Ref]
Endocrine
Opioids:
- Postmarketing reports: Adrenal insufficiency, androgen deficiency
Adrenal insufficiency and androgen deficiency have been reported with opioid use, most often with chronic use.
References
1. Leow KP, Smith MT, Watt JA, Williams BE, Cramond T (1992) "Comparative oxycodone pharmacokinetics in humans after intravenous, oral, and rectal administration." Ther Drug Monit, 14, p. 479-84
2. "Multum Information Services, Inc. Expert Review Panel"
3. (2017) "Product Information. Percocet 5/325 (acetaminophen-oxycodone)." Endo Laboratories LLC
4. (2017) "Product Information. Xartemis XR (acetaminophen-oxycodone)." Mallinckrodt Medical Inc
5. (2017) "Product Information. Acetaminophen-Oxycodone Hydrochloride (acetaminophen-oxycodone)." Mallinckrodt Medical Inc
6. (2001) "Product Information. Percocet (acetaminophen-oxycodone)." DuPont Pharmaceuticals
7. Kondo K, Inoue Y, Hamada H, Yokoyama A, Kohno N, Hiwada K (1993) "Acetaminophen-induced eosinophilic pneumonia." Chest, 104, p. 291-2
8. Kaysen GA, Pond SM, Roper MH, Menke DJ, Marrama MA (1985) "Combined hepatic and renal injury in alcoholics during therapeutic use of acetaminophen." Arch Intern Med, 145, p. 2019-23
9. O'Dell JR, Zetterman RK, Burnett DA (1986) "Centrilobular hepatic fibrosis following acetaminophen-induced hepatic necrosis in an alcoholic." JAMA, 255, p. 2636-7
10. Seeff LB, Cuccherini BA, Zimmerman HJ, Adler E, Benjamin SB (1986) "Acetaminophen hepatotoxicity in alcoholics." Ann Intern Med, 104, p. 399-404
11. Minton NA, Henry JA, Frankel RJ (1988) "Fatal paracetamol poisoning in an epileptic." Hum Toxicol, 7, p. 33-4
12. Keaton MR (1988) "Acute renal failure in an alcoholic during therapeutic acetaminophen ingestion." South Med J, 81, p. 1163-6
13. Shriner K, Goetz MB (1992) "Severe hepatotoxicity in a patient receiving both acetaminophen and zidovudine." Am J Med, 93, p. 94-6
14. Keays R, Harrison PM, Wendon JA, et al. (1991) "Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial." BMJ, 303, p. 1026-9
15. Rumore MM, Blaiklock RG (1992) "Influence of age-dependent pharmacokinetics and metabolism on acetaminophen hepatotoxicity." J Pharm Sci, 81, p. 203-7
16. Mofenson HC, Caraccio TR, Nawaz H, Steckler G (1991) "Acetaminophen induced pancreatitis." Clin Toxicol, 29, p. 223-30
17. Kumar S, Rex DK (1991) "Failure of physicians to recognize acetaminophen hepatotoxicity in chronic alcoholics." Arch Intern Med, 151, p. 1189-91
18. Block R, Jankowski JA, Lacoux P, Pennington CR (1992) "Does hypothermia protect against the development of hepatitis in paracetamol overdose?" Anaesthesia, 47, p. 789-91
19. Brotodihardjo AE, Batey RG, Farrell GC, Byth K (1992) "Hepatotoxicity from paracetamol self-poisoning in Western Sydney: a continuing challenge." Med J Aust, 157, p. 382-5
20. Johnson GK, Tolman KG (1977) "Chronic liver disease and acetaminophen." Ann Intern Med, 87, p. 302-4
21. McJunkin B, Barwick KW, Little WC, Winfield JB (1976) "Fatal massive hepatic necrosis following acetaminophen overdose." JAMA, 236, p. 1874-5
22. Block R (1993) "Liver failure induced by paracetamol." BMJ, 306, p. 457
23. Wong V, Daly M, Boon A, Heatley V (1993) "Paracetamol and acute biliary pain with cholestasis." Lancet, 342, p. 869
24. Bray GP (1993) "Liver failure induced by paracetamol." BMJ, 306, p. 157-8
25. Lee WM (1994) "Acute liver failure." Am J Med, 96, p. 3-9
26. Bonkovsky HL, Kane RE, Jones DP, Galinsky RE, Banner B (1994) "Acute hepatic and renal toxicity from low doses of acetaminophen in the absence of alcohol abuse or malnutrition - evidence for increased susceptibility to drug toxicity due to cardiopulmonary and renal insufficiency." Hepatology, 19, p. 1141-8
27. Cheung L, Potts RG, Meyer KC (1994) "Acetaminophen treatment nomogram." N Engl J Med, 330, p. 1907-8
28. Hartleb M (1994) "Do thyroid hormones promote hepatotoxicity to acetaminophen?" Am J Gastroenterol, 89, p. 1269-70
29. Smilkstein MJ, Douglas Dr, Daya MR (1994) "Acetaminophen poisoning and liver function." N Engl J Med, 331, p. 1310-1
30. Whitcomb DC (1994) "Acetaminophen poisoning and liver function." N Engl J Med, 331, p. 1311
31. Cheung L, Meyer KC (1994) "Acetaminophen poisoning and liver function." N Engl J Med, 331, p. 1311-2
32. Whitcomb DC, Block GD (1994) "Association of acetaminopphen hepatotoxicity with fasting and ethanol use." JAMA, 272, p. 1845-50
33. Bonkovsky HL (1995) "Acetaminophen hepatotoxicity, fasting, and ethanol." JAMA, 274, p. 301
34. Nelson EB, Temple AR (1995) "Acetaminophen hepatotoxicity, fasting, and ethanol." JAMA, 274, p. 301
35. Singer AJ, Carracio TR, Mofenson HC (1995) "The temporal profile of increased transaminase levels in patients with acetaminophen-induced liver dysfunction." Ann Emerg Med, 26, p. 49-53
36. Zimmerman HJ, Maddrey WC (1995) "Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: analysis of instances of therapeutic misadventure." Hepatology, 22, p. 767-73
37. Lee WM (1995) "Medical progress: drug-induced hepatotoxicity." N Engl J Med, 333, p. 1118-27
38. Bolesta S, Haber SL (2002) "Hepatotoxicity associated with chronic acetaminophen administration in patients without risk factors." Ann Pharmacother, 36, p. 331-3
39. Settipane RA, Stevenson DD (1989) "Cross sensitivity with acetaminophen in aspirin-sensitive subjects with asthma." J Allergy Clin Immunol, 84, p. 26-33
40. Van Diem L, Grilliat JP (1990) "Anaphylactic shock induced by paracetamol." Eur J Clin Pharmacol, 38, p. 389-90
41. Leung R, Plomley R, Czarny D (1992) "Paracetamol anaphylaxis." Clin Exp Allergy, 22, p. 831-3
42. Doan T, Greenberger PA (1993) "Nearly fatal episodes of hypotension, flushing, and dyspnea in a 47- year-old woman." Ann Allergy, 70, p. 439-44
43. Kalyoncu AF (1994) "Acetaminophen hypersensitivity and other analgesics." Ann Allergy, 72, p. 285
44. Doan T (1994) "Acetaminophen hypersensitivity and other analgesics - response." Ann Allergy, 72, p. 285
45. Thomas RH, Munro DD (1986) "Fixed drug eruption due to paracetamol." Br J Dermatol, 115, p. 357-9
46. Guccione JL, Zemtsov A, Cobos E, Neldner KH (1993) "Acquired purpura fulminans induced by alcohol and acetaminophen - successful treatment with heparin and vitamin-k." Arch Dermatol, 129, p. 1267-9
47. Filipe PL, Freitas JP, Decastro JC, Silva R (1995) "Drug eruption induced by acetaminophen in infectious mononucleosis." Int J Dermatol, 34, p. 220-1
48. Leow KP, Smith MT, Williams B, Cramond T (1992) "Single-dose and steady-state pharmacokinetics and pharmacodynamics of oxycodone in patients with cancer." Clin Pharmacol Ther, 52, p. 487-95
49. Glare P, Walsh D (1991) "Dose-ranging study of oxycodone for advanced cancer pain (meeting abstract)." Proc Annu Meet Am Soc Clin Oncol, 10, a1201
50. Glare PA, Walsh TD (1993) "Dose-ranging study of oxycodone for chronic pain in advanced cancer." J Clin Oncol, 11, p. 973-8
51. Sunshine A, Olson NZ, Zighelboim I, Decastro A (1993) "Ketoprofen, acetaminophen plus oxycodone, and acetaminophen in the relief of postoperative pain." Clin Pharmacol Ther, 54, p. 546-55
52. Fishbain DA, Goldberg M, Rosomoff RS, Rosomoff H (1988) "Atypical withdrawal syndrome (organic delusional syndrome) secondary to oxycodone detoxification ." J Clin Psychopharmacol, 8, p. 441-2
53. Shoenfeld Y, Shaklai M, Livni E, Pinkhas J (1980) "Thrombocytopenia from acetaminophen." N Engl J Med, 303, p. 47
54. Bougie DW, Benito AI, Sanchez-Abarca LI, Torres R, Birenbaum J, Aster RH (2007) "Acute thrombocytopenia caused by sensitivity to the glucuronide conjugate of acetaminophen." Blood, 109, p. 3608-9
55. Kleinman JG, Breitenfield RV, Roth DA (1980) "Transient cholestatic hepatitis in a neonate associated with carbamazepine exposure during pregnancy and breast-feeding." Clin Nephrol, 14, p. 201-5
56. Segasothy M, Suleiman AB, Puvaneswary M, Rohana A (1988) "Paracetamol: a cause for analgesic nephropathy and end-stage renal disease." Nephron, 50, p. 50-4
57. Duchene A, Chadenas D, Marneffe-Lebrequier H (1991) "Insuffisance renale aigue isolee apres intoxication volontaire par le paracetamol." Presse Med, 20, p. 1684-5
58. Curry RW, Robinson JD, Sughrue MJ (1982) "Acute renal failure after acetaminophen ingestion." JAMA, 247, p. 1012-4
59. Goldberg M (1982) "Analgesic nephropathy in 1981: which drug is responsible?" JAMA, 247, p. 64-5
60. Boyer TD, Rouff SL (1971) "Acetaminophen-induced hepatic necrosis and renal failure." JAMA, 218, p. 440-1
61. Vanchieri C (1993) "Australian study links certain analgesics to renal cancers." J Natl Cancer Inst, 85, p. 262-3
62. McCredie M, Stewart JH, Day NE (1993) "Different roles for phenacetin and paracetamol in cancer of the kidney and renal pelvis." Int J Cancer, 53, p. 245-9
63. Drenth JP, Frenken LA, Wuis EW, Van der Meer JW (1994) "Acute renal failure associated with paracetamol ingestion in an alcoholic patient." Nephron, 67, p. 483-5
64. Perneger TV, Whelton PK, Klag MJ (1994) "Risk of kidney failure associated with the use of acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs." N Engl J Med, 331, p. 1675-79
65. Brown G (1996) "Acetaminophen-induced hypotension." Heart Lung, 25, p. 137-40
66. Gardos G (1977) "Dyskinesia after discountinuation of compound analgesic containing oxycodone ." Lancet, 1, p. 759-60
More about Percocet 7.5 / 500 (acetaminophen / oxycodone)
- Check interactions
- Compare alternatives
- Reviews (5)
- Drug images
- Dosage information
- During pregnancy
- Drug class: narcotic analgesic combinations
Patient resources
Other brands
Endocet, Roxicet, Tylox, Primlev, ... +8 more
Professional resources
Other brands
Endocet, Roxicet, Tylox, Primlev, ... +3 more
Other formulations
Related treatment guides
Further information
Percocet 7.5/500 side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.