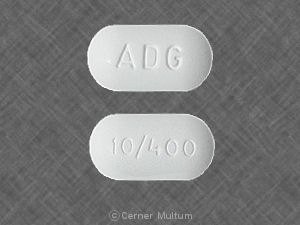
Magnacet (Oral)
Generic name: oxycodone and acetaminophen [ a-seet-a-MIN-oh-fen, ox-i-KOE-done-hye-droe-KLOR-ide ]
Other brand names of oxycodone and acetaminophen include: Endocet, Magnacet, Narvox, Percocet, Perloxx,
... show all 11 brands
Drug class: Narcotic analgesic combinations
Medically reviewed by Drugs.com. Last updated on Jun 15, 2025.
The Magnacet brand name has been discontinued in the U.S. If generic versions of this product have been approved by the FDA, there may be generic equivalents available.
Addiction, Abuse, and Misuse
Oxycodone/acetaminophen exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing oxycodone/acetaminophen, and monitor all patients regularly for the development of these behaviors or conditions .Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse and misuse, the Food and Drug Administration (FDA) has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to: complete a REMS-compliant education program, counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products, emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacists, and consider other tools to improve patient, household, and community safety .Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression may occur with use of oxycodone/acetaminophen. Monitor for respiratory depression, especially during initiation of oxycodone/acetaminophen or following a dose increase .Instruct patients to swallow oxycodone/acetaminophen ER tablets whole; crushing, chewing, or dissolving oxycodone/acetaminophen ER can cause rapid release and absorption of a potentially fatal dose of oxycodone Accidental Ingestion
Accidental ingestion of even one dose of oxycodone/acetaminophen, especially by children, can result in a fatal overdose of oxycodone .Neonatal Opioid Withdrawal Syndrome
Prolonged use of oxycodone/acetaminophen during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available .Cytochrome P450 3A4 Interaction
The concomitant use of Oxycodone/acetaminophen with all cytochrome P450 3A4 inhibitors may result in an increase in oxycodone plasma concentrations, which could increase or prolong adverse reactions and may cause potentially fatal respiratory depression. In addition, discontinuation of a concomitantly used cytochrome P450 3A4 inducer may result in an increase in oxycodone plasma concentration. Monitor patients receiving Oxycodone/acetaminophen and any CYP3A4 inhibitor or inducer .Hepatotoxicity
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at doses that exceed 4000 milligrams per day, and often involve more than one acetaminophen-containing product Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Reserve concomitant prescribing of oxycodone/acetaminophen and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation .
Uses for Magnacet
Oxycodone and acetaminophen combination is used to relieve pain severe enough to require opioid treatment and when other pain medicines did not work well enough or cannot be tolerated.
Acetaminophen is used to relieve pain and reduce fever in patients. It does not become habit-forming when taken for a long time. But acetaminophen may cause other unwanted effects when taken in large doses, including liver damage.
Oxycodone belongs to the group of medicines called narcotic analgesics (pain medicines). It acts on the central nervous system (CNS) to relieve pain.
When oxycodone is used for a long time, it may become habit-forming, causing mental or physical dependence. However, people who have continuing pain should not let the fear of dependence keep them from using narcotics to relieve their pain. Mental dependence (addiction) is not likely to occur when narcotics are used for this purpose. Physical dependence may lead to withdrawal side effects if treatment is stopped suddenly. However, severe withdrawal side effects can usually be prevented by gradually reducing the dose over a period of time before treatment is stopped completely.
This medicine is available only with your doctor's prescription. Percocet® and Xartemis™ are available only under a restricted distribution program called the Opioid Analgesic REMS (Risk Evaluation and Mitigation Strategy) program.
Before using Magnacet
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of oxycodone and acetaminophen combination in the pediatric population. Use of Xartemis™ is not recommended in children. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of oxycodone and acetaminophen combination extended-release tablet, solution, or tablet in the elderly. However, elderly patients are more likely to have age-related kidney, heart, lung, or liver problems, which may require caution and an adjustment in the dose for patients receiving this medicine.
Appropriate studies have not been performed on the relationship of age to the effects of oxycodone and acetaminophen combination capsules in the pediatric population. Safety and efficacy have not been established.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Levoketoconazole
- Nalmefene
- Naltrexone
- Safinamide
- Samidorphan
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abiraterone Acetate
- Acepromazine
- Aclidinium
- Adagrasib
- Alfentanil
- Almotriptan
- Alosetron
- Alprazolam
- Alvimopan
- Amantadine
- Amifampridine
- Amineptine
- Amiodarone
- Amitriptyline
- Amitriptylinoxide
- Amobarbital
- Amoxapine
- Amphetamine
- Amprenavir
- Anileridine
- Apalutamide
- Aprepitant
- Aripiprazole
- Aripiprazole Lauroxil
- Armodafinil
- Asciminib
- Asenapine
- Atazanavir
- Atropine
- Avacopan
- Baclofen
- Belladonna
- Belzutifan
- Benperidol
- Bentazepam
- Benzhydrocodone
- Benzphetamine
- Benztropine
- Berotralstat
- Biperiden
- Boceprevir
- Bosentan
- Bromazepam
- Bromopride
- Brompheniramine
- Buprenorphine
- Bupropion
- Buspirone
- Butabarbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Cannabis
- Carbamazepine
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Cenobamate
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpheniramine
- Chlorpromazine
- Chlorzoxazone
- Cimetidine
- Cinacalcet
- Ciprofloxacin
- Citalopram
- Clarithromycin
- Clemastine
- Clidinium
- Clobazam
- Clomipramine
- Clonazepam
- Clopidogrel
- Clorazepate
- Cloxazolam
- Clozapine
- Cobicistat
- Cocaine
- Codeine
- Conivaptan
- Crizotinib
- Cyclobenzaprine
- Cyclopentolate
- Cyclosporine
- Cyproheptadine
- Dabrafenib
- Dantrolene
- Daridorexant
- Darifenacin
- Darunavir
- Delavirdine
- Delorazepam
- Desipramine
- Desmopressin
- Desvenlafaxine
- Dexamethasone
- Dexmedetomidine
- Dextroamphetamine
- Dextromethorphan
- Dezocine
- Diacetylmorphine
- Diazepam
- Dibenzepin
- Dichloralphenazone
- Dicyclomine
- Difenoxin
- Dihydrocodeine
- Diltiazem
- Dimenhydrinate
- Diphenhydramine
- Diphenoxylate
- Dolasetron
- Donepezil
- Doxepin
- Doxylamine
- Dronedarone
- Droperidol
- Duloxetine
- Efavirenz
- Elagolix
- Eletriptan
- Enflurane
- Enzalutamide
- Erdafitinib
- Erythromycin
- Escitalopram
- Esketamine
- Eslicarbazepine Acetate
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Etravirine
- Fedratinib
- Fenfluramine
- Fentanyl
- Fesoterodine
- Fexinidazole
- Flavoxate
- Flibanserin
- Fluconazole
- Flunitrazepam
- Fluoxetine
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fluvoxamine
- Fosamprenavir
- Fosaprepitant
- Fosnetupitant
- Fosphenytoin
- Fospropofol
- Frovatriptan
- Furazolidone
- Gabapentin
- Gabapentin Enacarbil
- Gepirone
- Glycopyrrolate
- Glycopyrronium Tosylate
- Granisetron
- Halazepam
- Haloperidol
- Halothane
- Hexobarbital
- Homatropine
- Hydrocodone
- Hydromorphone
- Hydroxyamphetamine
- Hydroxytryptophan
- Hydroxyzine
- Hyoscyamine
- Idelalisib
- Imatinib
- Imipramine
- Indinavir
- Ipratropium
- Iproniazid
- Isocarboxazid
- Isoflurane
- Isoniazid
- Itraconazole
- Ivacaftor
- Ketamine
- Ketazolam
- Ketobemidone
- Ketoconazole
- Lacosamide
- Lanreotide
- Larotrectinib
- Lasmiditan
- Lefamulin
- Lemborexant
- Lenacapavir
- Letermovir
- Levocetirizine
- Levomilnacipran
- Levorphanol
- Linezolid
- Lisdexamfetamine
- Lithium
- Lofepramine
- Lofexidine
- Lomitapide
- Lopinavir
- Loprazolam
- Lorazepam
- Lorcaserin
- Lorlatinib
- Lormetazepam
- Loxapine
- Lumacaftor
- Magnesium Oxybate
- Mavacamten
- Meclizine
- Medazepam
- Melitracen
- Melperone
- Mepenzolate
- Meperidine
- Mephobarbital
- Meprobamate
- Meptazinol
- Mesoridazine
- Metaclazepam
- Metaxalone
- Methadone
- Methamphetamine
- Methdilazine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Methylene Blue
- Methylnaltrexone
- Metoclopramide
- Mibefradil
- Midazolam
- Mifepristone
- Milnacipran
- Mirabegron
- Mirtazapine
- Mitotane
- Mobocertinib
- Moclobemide
- Modafinil
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nafcillin
- Nalbuphine
- Nalorphine
- Naloxone
- Naratriptan
- Nefazodone
- Nelfinavir
- Netupitant
- Nevirapine
- Nialamide
- Nicomorphine
- Nilotinib
- Nitrazepam
- Nitrous Oxide
- Nordazepam
- Nortriptyline
- Octreotide
- Olanzapine
- Omaveloxolone
- Ondansetron
- Opipramol
- Opium
- Opium Alkaloids
- Orphenadrine
- Oxazepam
- Oxcarbazepine
- Oxitropium Bromide
- Oxybutynin
- Oxymorphone
- Ozanimod
- Palbociclib
- Palonosetron
- Papaveretum
- Paregoric
- Paroxetine
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenelzine
- Phenobarbital
- Phenytoin
- Pimozide
- Pinazepam
- Pipenzolate Bromide
- Piperacetazine
- Pipotiazine
- Pirenzepine
- Piritramide
- Pirtobrutinib
- Pixantrone
- Pneumococcal 13-Valent Vaccine, Diphtheria Conjugate
- Posaconazole
- Potassium Oxybate
- Prazepam
- Prednisone
- Pregabalin
- Primidone
- Procarbazine
- Prochlorperazine
- Procyclidine
- Promazine
- Promethazine
- Propantheline
- Propiverine
- Propofol
- Protriptyline
- Quazepam
- Quetiapine
- Quinidine
- Quinine
- Ramelteon
- Ranitidine
- Ranolazine
- Rasagiline
- Remifentanil
- Remimazolam
- Remoxipride
- Ribociclib
- Rifabutin
- Rifampin
- Rifapentine
- Ritlecitinib
- Ritonavir
- Rizatriptan
- Rolapitant
- Ropeginterferon Alfa-2b-njft
- Saquinavir
- Scopolamine
- Secobarbital
- Selegiline
- Selpercatinib
- Sertindole
- Sertraline
- Sibutramine
- Sodium Oxybate
- Solifenacin
- Sotorasib
- Stramonium
- Sufentanil
- Sulpiride
- Sumatriptan
- Suvorexant
- Tapentadol
- Taurursodiol
- Telaprevir
- Telithromycin
- Temazepam
- Terbinafine
- Terodiline
- Tetrazepam
- Thiethylperazine
- Thiopental
- Thiopropazate
- Thioridazine
- Thiothixene
- Tianeptine
- Tilidine
- Tiotropium
- Tizanidine
- Tocilizumab
- Tolonium Chloride
- Tolterodine
- Topiramate
- Tramadol
- Tranylcypromine
- Trazodone
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trihexyphenidyl
- Trimeprazine
- Trimipramine
- Trofinetide
- Tropicamide
- Trospium
- Tryptophan
- Tucatinib
- Umeclidinium
- Venlafaxine
- Verapamil
- Vilazodone
- Voriconazole
- Vortioxetine
- Voxelotor
- Zaleplon
- Ziprasidone
- Zolmitriptan
- Zolpidem
- Zopiclone
- Zotepine
- Zuranolone
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acenocoumarol
- Carbamazepine
- Fosphenytoin
- Lixisenatide
- Phenytoin
- St John's Wort
- Warfarin
- Zidovudine
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
- Grapefruit Juice
- Tobacco
Using this medicine with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Cabbage
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Addison disease (adrenal gland problem) or
- Alcohol abuse, history of or
- Brain tumor, history of or
- Breathing or lung problems (eg, low oxygen levels, sleep apnea) or
- Chronic obstructive pulmonary disease (COPD) or
- Cor pulmonale (serious heart problem) or
- Drug dependence, especially with narcotic abuse or dependence, or history of or
- Gallbladder disease or
- Head injury, history of or
- Hypothyroidism (an underactive thyroid) or
- Hypovolemia (low blood volume) or
- Kyphoscoliosis (curvature of the spine with breathing problems) or
- Mental health problems or
- Problems with passing urine or
- Prostatic hypertrophy (enlarged prostate, BPH) or
- Trouble swallowing or
- Weakened physical condition—Use with caution. May increase risk for more serious side effects.
- Asthma, acute or severe or
- Lung disease or breathing problems (eg, asthma, respiratory depression), severe or
- Stomach or bowel blockage (eg, paralytic ileus), known or suspected—Should not be used in patients with these conditions.
- Hypotension (low blood pressure) or
- Pancreatitis (swelling of the pancreas) or
- Seizures, history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Proper use of Magnacet
Take this medicine only as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. This is especially important for elderly patients, who may be more sensitive to the effects of pain medicines. If too much of this medicine is taken for a long time, it may become habit-forming and cause mental or physical dependence. Also, large amounts of acetaminophen may cause liver damage if taken for a long time.
It is very important that you understand the rules of the Opioid Analgesic REMS program to prevent addiction, abuse, and misuse of oxycodone and acetaminophen combination. This medicine should also come with a Medication Guide. Read and follow these instructions carefully. Read it again each time you refill your prescription in case there is new information. Ask your doctor if you have any questions.
You may take this medicine with or without food.
Measure the oral liquid using the patient cup that comes with the package.
Swallow the extended-release tablet whole with water. Do not crush, break, chew, dissolve, snort, or inject it. Do not pre-soak, lick, or wet the tablet before placing it in your mouth. Do not give this medicine by feeding tubes.
Check with your doctor first before changing dosage forms (eg, capsules, extended-release tablets, tablets). These forms are very different from each other.
This combination medicine contains acetaminophen (Tylenol®). Carefully check the labels of all other medicines you are using, because they may also contain acetaminophen. It is not safe to use more than 4 grams (4,000 milligrams) of acetaminophen in one day (24 hours).
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For moderate to moderately severe pain:
- For oral dosage form (capsules):
- Adults—1 capsule every 6 hours as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (extended-release tablets):
- Adults—2 tablets every 12 hours as needed.
- Children—Use is not recommended.
- For oral dosage form (solution):
- Adults—5 milliliters (mL) or 1 teaspoon every 6 hours as needed. Your doctor may adjust the dose as needed. However, the dose is usually not more than 60 mL (12 teaspoons) per day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—1 or 2 tablets every 6 hours as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (capsules):
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
If you miss a dose of Percocet®, skip the missed dose and go back to your regular dosing schedule.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Oxycodone and acetaminophen combination can cause serious unwanted effects or fatal overdose if taken by children, pets, or adults who are not used to strong narcotic pain medicines. Make sure you store the medicine in a safe and secure place to prevent others from getting it.
Drop off any unused narcotic medicine at a drug take-back location right away. If you do not have a drug take-back location near you, flush any unused narcotic medicine down the toilet. Check your local drug store and clinics for take-back locations. You can also check the DEA web site for locations. Here is the link to the FDA safe disposal of medicines website:www.fda.gov/drugs/resourcesforyou/consumers/buyingusingmedicinesafely/ensuringsafeuseofmedicine/safedisposalofmedicines/ucm186187.htm .
Precautions while using Magnacet
It is very important that your doctor check your progress while you are taking this medicine, especially within the first 24 to 72 hours of treatment. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for unwanted effects.
It is against the law and dangerous for anyone else to use your medicine. Keep your unused medicine in a safe and secure place. People who are addicted to drugs might want to steal it.
Check with your doctor before using this medicine with alcohol or other medicines that affect the central nervous system (CNS). This medicine will add to the effects of alcohol and other CNS depressants (medicines that can make you drowsy or less alert). Some examples of CNS depressants are antihistamines or medicine for allergies or colds, sedatives, tranquilizers, or sleeping medicine, other prescription pain medicine or narcotics, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics. Also, there may be a greater risk of liver damage if you drink three or more alcoholic beverages while you are taking acetaminophen. Do not drink alcoholic beverages.
If you think you or someone else may have taken an overdose of this medicine, get emergency help at once. Your doctor may also give naloxone to treat an overdose. Signs of an overdose include: extreme dizziness or weakness, slow heartbeat or breathing, seizures, trouble breathing, and cold, clammy skin. Call your doctor right away if you notice these symptoms.
This medicine may be habit-forming. If you feel that the medicine is not working as well, do not use more than your prescribed dose. Call your doctor for instructions.
Do not use this medicine if you are using or have used an MAO inhibitor (eg, isocarboxazid [Marplan®], linezolid [Zyvox®], phenelzine [Nardil®], selegiline [Eldepryl®], tranylcypromine [Parnate®]) within the past 14 days. Using these medicine together may cause serious unwanted effects.
This medicine may cause sleep-related breathing problems (eg, sleep apnea, sleep-related hypoxemia). Your doctor may decrease your dose if you have sleep apnea (stop breathing for short periods during sleep) while using this medicine.
Dizziness, lightheadedness, or fainting may occur when you get up suddenly from a lying or sitting position. Getting up slowly may help lessen this problem. Also, lying down for a while may relieve the dizziness or lightheadedness.
This medicine may make you dizzy, drowsy, or lightheaded. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
Check with your doctor right away if you have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
Serious skin reactions (eg, acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, and toxic epidermal necrolysis) can occur with this medicine. Check with your doctor right away if you have blistering, peeling, or loosening of the skin, chills, cough, diarrhea, itching, joint or muscle pain red irritated eyes, red skin lesions, often with a purple center, sore throat, sores, ulcers, or white spots in the mouth or on the lips, or unusual tiredness or weakness while you are using this medicine.
This medicine may cause serious allergic reactions, including anaphylaxis, which can be life-threatening and requires immediate medical attention. Call your doctor right away if you have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth while you are using this medicine.
Using narcotics for a long time can cause severe constipation. To prevent this, your doctor may direct you to take laxatives, drink a lot of fluids, or increase the amount of fiber in your diet. Be sure to follow the directions carefully, because continuing constipation can lead to more serious problems.
If you have been using this medicine regularly for several weeks or longer, do not change your dose or suddenly stop using it without checking with your doctor. Your doctor may want you to gradually reduce the amount you are using before stopping it completely. This may help prevent worsening of your condition and reduce the possibility of withdrawal symptoms, including stomach cramps, anxiety, fever, irritability, nausea, restlessness, runny nose, sweating, tremors, or trouble with sleeping.
Using this medicine while you are pregnant may cause serious unwanted effects, including neonatal withdrawal syndrome in your newborn baby. Tell your doctor right away if you think you are pregnant or if you plan to become pregnant while using this medicine.
For nursing mothers:
- Talk to your doctor if you have any questions about taking oxycodone or about how this medicine may affect your baby.
- Call your doctor if you become extremely tired and have difficulty caring for your baby.
- Your baby should generally nurse every 2 to 3 hours and should not sleep for more than 4 hours at a time.
- Check with your doctor or hospital emergency room immediately if your baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, difficulty breathing, or limpness. These may be symptoms of an overdose and need immediate medical attention.
Before you have any medical tests, tell the medical doctor in charge that you are taking this medicine. The results of some tests may be affected by this medicine.
Check with your doctor right away if you have anxiety, restlessness, a fast heartbeat, fever, sweating, muscle spasms, twitching, nausea, vomiting, diarrhea, or see or hear things that are not there. These may be symptoms of a serious condition called serotonin syndrome. Your risk may be higher if you also take certain other medicines that affect serotonin levels in your body.
Using too much of this medicine may cause infertility (unable to have children). Talk with your doctor before using this medicine if you plan to have children.
This medicine may cause adrenal gland problems. Check with your doctor right away if you have darkening of the skin, diarrhea, dizziness, fainting, loss of appetite, mental depression, nausea, skin rash, unusual tiredness or weakness, or vomiting.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Side Effects of Magnacet
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Black, tarry stools
- chills
- dark urine
- dizziness
- fever
- headache
- itching, skin rash
- light-colored stools
- loss of appetite
- nausea
- stomach pain
- unpleasant breath odor
- unusual tiredness or weakness
- vomiting of blood
- yellow eyes or skin
Rare
- Cough
- fever with or without chills
- general feeling of tiredness or weakness
- hoarseness
- lower back or side pain
- painful or difficult urination
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- unusual bleeding or bruising
Incidence not known
- Back, leg, or stomach pains
- bleeding gums
- bloating
- blood in the urine or stools
- blue lips and fingernails
- blurred vision
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- chest pain, discomfort, or tightness
- cloudy urine
- clumsiness
- confusion
- constipation
- coughing that sometimes produces a pink frothy sputum
- darkening of the skin
- decreased awareness or responsiveness
- decreased frequency or amount of urine
- diarrhea
- difficult, fast, noisy breathing
- difficulty in passing urine (dribbling)
- difficulty with swallowing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- drowsiness
- dry mouth
- extremely shallow or slow breathing
- fainting
- fast or deep breathing
- fast, slow, irregular, pounding, or racing heartbeat
- feeling of warmth
- general body swelling
- hives or welts
- increased sweating
- increased thirst
- indigestion
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- lightheadedness
- mental depression
- muscle aches, tremors, or weakness
- nervousness
- nosebleeds
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pale skin
- pinpoint red spots on the skin
- pounding in the ears
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid, deep or shallow breathing
- redness of the face, neck, arms, and occasionally, upper chest
- restlessness
- seizures
- severe constipation
- severe sleepiness
- severe vomiting
- skin blisters
- sleepiness
- stomach cramps
- sunken eyes
- sweating
- swelling of the face, fingers, lower legs, or ankles
- thirst
- tiredness
- trouble breathing
- vomiting
- weakness or heaviness of the legs
- weight gain
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of overdose
- Bluish lips or skin
- change in consciousness
- cold, clammy skin
- extreme sleepiness
- general feeling of discomfort or illness
- loss of consciousness
- low blood pressure or pulse
- slow breathing
- unconsciousness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Relaxed and calm feeling
Incidence not known
- Agitation
- bad, unusual or unpleasant (after) taste
- belching
- change in taste
- cold sweats
- constricted, pinpoint, or small pupils (black part of the eye)
- continuing ringing or buzzing or other unexplained noise in the ears
- cool, pale skin
- depression
- difficulty with moving
- disturbed color perception
- double vision
- excess air or gas in the stomach or bowels
- false or unusual sense of well-being
- flushed, dry skin
- fruit-like breath odor
- full feeling
- general feeling of discomfort or illness
- halos around lights
- hearing loss
- heartburn
- increased hunger
- increased urination
- indigestion
- joint pain
- lack or loss of strength
- muscle cramps, spasms, pain, or stiffness
- night blindness
- nightmares
- overbright appearance of lights
- seeing, hearing, or feeling things that are not there
- seizures
- shakiness
- slurred speech
- swollen joints
- trouble sleeping
- tunnel vision
- unexplained weight loss
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Endocet
- Magnacet
- Narvox
- Percocet
- Perloxx
- Primalev
- Roxicet
- Roxilox
- Tylox
- Xartemix XR
- Xolox
In Canada
- oxyCODONE/ACET
- Rivacocet
- Teva-Oxycocet
Available Dosage Forms:
- Tablet
- Solution
Therapeutic Class: Opioid/Acetaminophen Combination
Chemical Class: Oxycodone
More about Magnacet (acetaminophen / oxycodone)
- Check interactions
- Compare alternatives
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: narcotic analgesic combinations
Patient resources
Other brands
Percocet, Endocet, Roxicet, Tylox, ... +8 more
Professional resources
Other brands
Percocet, Endocet, Roxicet, Tylox, ... +4 more
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.