Glecaprevir / Pibrentasvir Side Effects
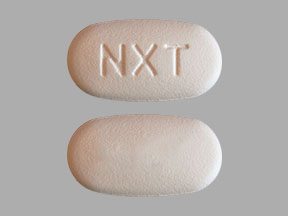
Applies to glecaprevir / pibrentasvir: oral packet, oral tablet.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Test all patients for evidence of current or prior hepatitis B virus (HBV) infection before initiating treatment with glecaprevir / pibrentasvir.
HBV reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct-acting antivirals and were not receiving HBV antiviral therapy.
Some cases have resulted in fulminant hepatitis, hepatic failure, and death.
Monitor HCV/HBV coinfected patients for hepatitis flare or HBV reactivation during HCV treatment and post-treatment follow-up.
Initiate appropriate patient management for HBV infection as clinically indicated.
Precautions
It is very important that your doctor check your or your child's progress at regular visits to make sure that this medicine is working properly. Blood tests may be needed to check for unwanted effects.
Do not use this medicine together with atazanavir (eg, Evotaz®, Reyataz®) or rifampin (eg, Rifadin®, Rifamate®, Rifater®, Rimactane®).
If you have ever had a hepatitis B infection, the virus could become active again during treatment with glecaprevir and pibrentasvir combination. You should be tested for hepatitis B infection before starting treatment with this medicine. Talk with your doctor if you have concerns.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
Other side effects
Some side effects of glecaprevir / pibrentasvir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- diarrhea
- itching skin
- lack or loss of strength
- nausea
- unusual tiredness or weakness
Serious side effects
Along with its needed effects, glecaprevir / pibrentasvir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking glecaprevir / pibrentasvir:
Incidence not known
- dark-colored urine
- headache
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- light-colored stools
- stomach pain, continuing
- yellow eyes or skin
See also:
For healthcare professionals
Applies to glecaprevir / pibrentasvir: oral pellet, oral tablet.
General adverse events
The most common side effects reported with this drug in hepatitis C virus (HCV)-infected patients without cirrhosis were headache, fatigue, and nausea. The most common side effects reported in HCV-infected patients with compensated cirrhosis (Child-Pugh A) were fatigue, headache, nausea, diarrhea, and pruritus. The most common side effects reported in HCV-infected patients with severe renal dysfunction were pruritus, fatigue, nausea, asthenia, and headache. The most common side effects reported in HCV/HIV-1-coinfected patients were fatigue, nausea, and headache. The most common side effects reported in HCV-infected patients with liver or kidney transplant were headache, fatigue, nausea, and pruritus. The most common side effects reported in HCV-infected patients who inject drugs (currently/recently [within the last 12 months prior to therapy]) were fatigue, headache, diarrhea, and nausea. The most common side effects reported in HCV-infected patients with concomitant use of medication-assisted treatment for opioid use disorder were headache, fatigue, nausea, and diarrhea.[Ref]
Nervous system
- Very common (10% or more): Headache (up to 17%)
- Rare (less than 0.1%): Transient ischemic attack[Ref]
Dermatologic
- Very common (10% or more): Pruritus (up to 17.3%)
- Frequency not reported: Rash, erythematous rash
- Postmarketing reports: Angioedema[Ref]
Hepatic
- Very common (10% or more): Elevated bilirubin (up to 17%)
- Common (1% to 10%): Elevated total bilirubin
- Uncommon (0.1% to 1%): Direct hyperbilirubinemia
- Frequency not reported: Jaundice
- Postmarketing reports: Hepatic decompensation, hepatic failure[Ref]
Elevated total bilirubin (at least 2 times the upper limit of normal [2 x ULN]) was reported in 3.5% of patients; such elevations were seen in 1.2% of patients across phase 2 and 3 trials and were related to glecaprevir-mediated inhibition of bilirubin transporters and metabolism. Bilirubin elevations were asymptomatic, transient, and generally occurred early during therapy; these elevations were mainly indirect and not associated with ALT elevations.
In patients with compensated cirrhosis (Child-Pugh A), 17% reported early, transient postbaseline bilirubin elevations above the ULN; these elevations were normally less than 2 x ULN, usually occurred with the first 2 weeks of therapy, and resolved with continued therapy. Patient with compensated cirrhosis and elevated bilirubin did not have concomitant increases in ALT/AST or signs of liver decompensation/failure; these laboratory events did not result in discontinuation of therapy. Few patients reported jaundice or ocular icterus and total bilirubin levels decreased after completion of therapy.[Ref]
Other
- Very common (10% or more): Fatigue (up to 16%)
- Common (1% to 10%): Asthenia[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (up to 12%)
- Common (1% to 10%): Diarrhea
- Frequency not reported: Vomiting, upper abdominal pain[Ref]
Ocular
- Frequency not reported: Ocular icterus
References
1. Cerner Multum, Inc. "UK Summary of Product Characteristics."
2. Cerner Multum, Inc. "Australian Product Information."
3. (2017) "Product Information. Mavyret (glecaprevir-pibrentasvir)." Abbott Pharmaceutical
Frequently asked questions
- What are the new drugs for the treatment of hepatitis C?
- Does Mavyret cure hep C (HCV)? What is the success rate?
- Can you take antibiotics with Mavyret?
- Does Mavyret cause itching?
- What types of Hepatitis C does Mavyret treat?
More about glecaprevir / pibrentasvir
- Check interactions
- Compare alternatives
- Reviews (431)
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Glecaprevir/pibrentasvir side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.