Glecaprevir And Pibrentasvir (Monograph)
Brand name: Mavyret
Drug class: HCV Protease Inhibitors
Warning
- Risk of HBV Reactivation in Patients Coinfected with HCV and HBV
-
HBV reactivation, including cases resulting in fulminant hepatitis, hepatic failure, and death, reported in patients coinfected with HCV and HBV who were receiving or had completed treatment with HCV direct-acting antivirals (DAAs) and were not receiving HBV antiviral therapy.
-
Test all patients for evidence of current or prior HBV infection before initiating fixed combination of glecaprevir and pibrentasvir (glecaprevir/pibrentasvir).
-
Monitor patients coinfected with HCV and HBV for hepatitis flare or HBV reactivation during and after HCV treatment. Initiate appropriate management for HBV infection as clinically indicated.
Introduction
HCV antiviral; fixed combination containing glecaprevir (HCV nonstructural 3/4A [NS3/4A] protease inhibitor) and pibrentasvir (HCV NS5A replication complex inhibitor [NS5A inhibitor]).
Uses for Glecaprevir And Pibrentasvir
Chronic HCV Infection
Treatment of chronic HCV genotype 1, 2, 3, 4, 5, or 6 infection in adults and pediatric patients ≥3 years of age without cirrhosis or with compensated cirrhosis (Child-Pugh class A), including liver or kidney transplant recipients and those with HIV coinfection.
In patients with HCV genotype 1 infection, glecaprevir/pibrentasvir is indicated in those who previously have been treated with a regimen containing an HCV NS5A inhibitor or an NS3/4A protease inhibitor (PI), but not both.
Treatment of chronic HCV infection is complex and rapidly evolving; consult a specialist to obtain the most up-to-date information. Information from the American Association for the Study of Liver Diseases (AASLD) and Infectious Diseases Society of America (IDSA) regarding diagnosis and management of HCV infection, including recommendations for initial treatment, is available at [Web].
Glecaprevir And Pibrentasvir Dosage and Administration
General
Pretreatment Screening
-
Prior to initiating glecaprevir/pibrentasvir, test all patients for evidence of current or prior HBV infection by measuring hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc).
Patient Monitoring
-
In patients with serologic evidence of HBV infection, monitor for clinical and laboratory signs of hepatitis flare or HBV reaction both during and after treatment with glecaprevir/pibrentasvir.
-
Monitor patients with compensated cirrhosis (Child-Pugh A) or evidence of advanced liver disease (e.g., portal hypertension) for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage) during treatment with glecaprevir/pibrentasvir.
Administration
Oral Administration
Administer orally once daily with food.
Available as fixed-combination film-coated tablets and oral pellets.
Preparation and Administration of Glecaprevir/Pibrentasvir Oral Pellets
Administer with a small amount of soft food that has low water content and will stick to a spoon (e.g., peanut butter, chocolate hazelnut spread, cream cheese, thick jam, Greek yogurt). Do not mix with liquids or foods that can drip or slide off a spoon as the drug may dissolve more readily and become less effective when mixed with foods with higher water content.
Sprinkle entire contents of the appropriate number of packets containing glecaprevir/pibrentasvir pellets onto the food. Do not crush or chew the pellets. Swallow entire mixture within 15 minutes after preparation.
No pellets should remain in the packet(s). Discard any unused portion of the mixture.
Dosage
Available as fixed-combination tablets containing 100 mg of glecaprevir and 40 mg of pibrentasvir in each tablet, and as fixed-combination oral pellets containing 50 mg of glecaprevir and 20 mg of pibrentasvir in each packet.
Pediatric Patients
Treatment of Chronic HCV Infection
HCV Genotype 1, 2, 3, 4, 5, or 6 Infection
OralPediatric patients ≥3 years of age: Recommended dosage based on weight. Treatment duration depends on HCV genotype, previous HCV treatment experience, and presence of compensated cirrhosis. (See Tables 1, 2, and 3.)
Dosing with oral pellets has not been studied in pediatric patients weighing >45 kg.
|
Weight (kg) or Age (years of age) |
Dosage of Glecaprevir/Pibrentasvir Tablets or Pellets |
Total Daily Glecaprevir/Pibrentasvir Dosage |
|---|---|---|
|
<20 kg |
Pellets: Three packets containing glecaprevir 50 mg/pibrentasvir 20 mg pellets once daily |
Glecaprevir 150 mg/pibrentasvir 60 mg daily |
|
20 to <30 kg |
Pellets: Four packets containing glecaprevir 50 mg/pibrentasvir 20 mg pellets once daily |
Glecaprevir 200 mg/pibrentasvir 80 mg daily |
|
30 to <45 kg |
Pellets: Five packets containing glecaprevir 50 mg/pibrentasvir 20 mg pellets once daily |
Glecaprevir 250 mg/pibrentasvir 100 mg daily |
|
≥45 kg or ≥12 years of age |
Tablets: Three tablets containing glecaprevir 100 mg/pibrentasvir 40 mg once daily |
Glecaprevir 300 mg/pibrentasvir 120 mg daily |
|
or |
||
|
Pellets: Six packets containing glecaprevir 50 mg/pibrentasvir 20 mg pellets once daily |
Glecaprevir 300 mg/pibrentasvir 120 mg daily |
|
HCV Genotype |
Hepatic Impairment |
Duration of Glecaprevir/Pibrentasvir |
|---|---|---|
|
HCV genotype 1, 2, 3, 4, 5, or 6 infection |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis (Child-Pugh class A) |
8 weeks |
Previously received HCV regimen containing interferon, peginterferon, ribavirin, and/or sofosbuvir; no previous treatment with HCV NS3/4A protease inhibitors or HCV NS5A inhibitors.
In clinical trials, patients previously received HCV regimens containing the fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir) or daclatasvir (no longer commercially available) in conjunction with peginterferon and ribavirin.
In clinical trials, patients previously received HCV regimens containing simeprevir (no longer commercially available) in conjunction with sofosbuvir or simeprevir, boceprevir, or telaprevir (drugs no longer commercially available) in conjunction with peginterferon and ribavirin.
|
HCV Genotype |
Treatment Experience |
Hepatic Impairment |
Duration of Glecaprevir/Pibrentasvir |
|---|---|---|---|
|
HCV genotype 1 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis (Child-Pugh class A) |
12 weeks |
||
|
Previously treated with an HCV NS5A inhibitor; no prior treatment with HCV NS3/4A protease inhibitors |
Noncirrhotic |
16 weeks |
|
|
Compensated cirrhosis |
16 weeks |
||
|
Previously treated with an HCV NS3/4A protease inhibitor; no prior treatment with HCV NS5A inhibitors |
Noncirrhotic |
12 weeks |
|
|
Compensated cirrhosis |
12 weeks |
||
|
HCV genotype 2, 4, 5, or 6 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis |
12 weeks |
||
|
HCV genotype 3 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
16 weeks |
|
Compensated cirrhosis |
16 weeks |
HCV-infected Individuals with HIV Coinfection
OralPediatric patients ≥12 years of age weighing ≥45 kg without cirrhosis or with compensated cirrhosis (Child-Pugh class A): Dosage and duration of therapy generally same as those recommended for patients without HIV coinfection.
HCV Genotype 1, 2, 3, 4, 5, or 6 Infection in Liver or Kidney Transplant Patients
OralPediatric patients ≥12 years of age weighing ≥45 kg without cirrhosis or with compensated cirrhosis (Child-Pugh class A): 3 tablets (total of 300 mg of glecaprevir and 120 mg of pibrentasvir) once daily for 12 weeks.
A treatment duration of 16 weeks in those with HCV genotype 1 infection previously treated with an HCV NS5A inhibitor, but not an HCV NS3/4A protease inhibitor, and in those with HCV genotype 3 infection previously treated with interferon, peginterferon, ribavirin, and/or sofosbuvir, but not an HCV NS3/4A protease inhibitor or HCV NS5A inhibitor.
Adults
Treatment of Chronic HCV Infection
HCV Genotype 1, 2, 3, 4, 5, or 6 Infection
OralWithout cirrhosis or with compensated cirrhosis (Child-Pugh class A): 3 tablets (total of 300 mg of glecaprevir and 120 mg of pibrentasvir) once daily. Treatment duration depends on HCV genotype, previous HCV treatment experience, and presence of compensated cirrhosis. (See Tables 4 and 5.)
|
HCV Genotype |
Hepatic Impairment |
Duration of Glecaprevir/Pibrentasvir |
|---|---|---|
|
HCV genotype 1, 2, 3, 4, 5, or 6 infection |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis (Child-Pugh class A) |
8 weeks |
Previously received HCV regimen containing interferon, peginterferon, ribavirin, and/or sofosbuvir; no previous treatment with HCV NS3/4A protease inhibitors or HCV NS5A inhibitors.
In clinical trials, patients previously received HCV regimens containing the fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir) or daclatasvir (no longer commercially available) in conjunction with peginterferon and ribavirin.
In clinical trials, patients previously received HCV regimens containing simeprevir (no longer commercially available) in conjunction with sofosbuvir or simeprevir, boceprevir, or telaprevir (drugs no longer commercially available) in conjunction with peginterferon and ribavirin.
|
HCV Genotype |
Treatment Experience |
Hepatic Impairment |
Duration of Glecaprevir/Pibrentasvir |
|---|---|---|---|
|
HCV genotype 1 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis (Child-Pugh class A) |
12 weeks |
||
|
Previously treated with an HCV NS5A inhibitor; no prior treatment with HCV NS3/4A protease inhibitors |
Noncirrhotic |
16 weeks |
|
|
Compensated cirrhosis |
16 weeks |
||
|
Previously treated with an HCV NS3/4A protease inhibitor; no prior treatment with HCV NS5A inhibitors |
Noncirrhotic |
12 weeks |
|
|
Compensated cirrhosis |
12 weeks |
||
|
HCV genotype 2, 4, 5, or 6 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
8 weeks |
|
Compensated cirrhosis |
12 weeks |
||
|
HCV genotype 3 infection |
Previously treated without HCV NS3/4A protease inhibitors or HCV NS5A inhibitors |
Noncirrhotic |
16 weeks |
|
Compensated cirrhosis |
16 weeks |
HCV-infected Individuals with HIV Coinfection
OralWithout cirrhosis or with compensated cirrhosis (Child-Pugh class A): Dosage and duration of therapy generally same as those recommended for adults without HIV coinfection.
HCV Genotype 1, 2, 3, 4, 5, or 6 Infection in Liver or Kidney Transplant Recipients
OralWithout cirrhosis or with compensated cirrhosis (Child-Pugh class A): 3 tablets (total of 300 mg of glecaprevir and 120 mg of pibrentasvir) once daily for 12 weeks.
A treatment duration of 16 weeks in those with HCV genotype 1 infection previously treated with an HCV NS5A inhibitor, but not an HCV NS3/4A protease inhibitor, and in those with HCV genotype 3 infection previously treated with interferon, peginterferon, ribavirin, and/or sofosbuvir, but not an HCV NS3/4A protease inhibitor or HCV NS5A inhibitor.
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustments not needed. Monitor for signs and symptoms of hepatic decompensation.
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation: Contraindicated.
Renal Impairment
Mild, moderate, or severe renal impairment (including hemodialysis patients): Dosage adjustments not needed. Not removed by hemodialysis to any clinically important extent.
Geriatric Patients
Dosage adjustments not needed.
Persons Who Inject Drugs (PWID) or Receive Medication-Assisted Treatment (MAT) for Opioid Use Disorder
Dosage adjustment not necessary in PWID or who are receiving MAT for opioid use disorder.
Cautions for Glecaprevir And Pibrentasvir
Contraindications
-
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation.
-
Concomitant use with atazanavir or rifampin.
Warnings/Precautions
Warnings
Risk of HBV Reactivation in Patients Coinfected with HCV and HBV
Postmarketing reports of reactivation of HBV infection when HCV DAAs were used for treatment of HCV infection in patients with HBV coinfection; fulminant hepatitis, hepatic failure, and death reported in some cases.
HBV reactivation (abrupt increase in HBV replication manifested as rapid increase in serum HBV DNA levels or detection of HBsAg in an individual who was previously HBsAg negative and anti-HBc positive) reported in patients with HCV and HBV coinfection receiving HCV treatment with a regimen that included HCV DAAs without HBV antiviral therapy. HBV reactivation usually occurred within 4–8 weeks after initiation of HCV treatment.
Patients with HBV reactivation heterogeneous in terms of HCV genotype and baseline HBV disease. Some patients were HBsAg positive; others had serologic evidence of resolved HBV infection (i.e., HBsAg negative and anti-HBc positive).
HBV reactivation also reported in patients receiving certain immunosuppressant or chemotherapeutic drugs; risk of reactivation associated with HCV DAAs may be increased in such patients.
Mechanism for HBV reactivation in coinfected patients receiving HCV DAAs unknown. Although HCV DAAs not known to cause immunosuppression, HBV reactivation in coinfected patients may result from a complex interplay of host immunologic responses in the setting of infection with 2 hepatitis viruses.
Prior to initiating treatment with glecaprevir/pibrentasvir, screen all patients for evidence of current or prior HBV infection by measuring HBsAg and anti-HBc. If there is serologic evidence of HBV infection, measure baseline HBV DNA level.
In all patients with evidence of current or prior HBV infection, monitor for clinical and laboratory signs (i.e., HBsAg, HBV DNA levels, serum aminotransferase and bilirubin concentrations) of hepatitis flare or HBV reactivation during and after treatment with HCV DAAs. Initiate appropriate management for HBV infection as clinically indicated
Advise coinfected patients to immediately contact a clinician if they develop any signs or symptoms of serious liver injury.
When making decisions regarding HBV monitoring or HBV treatment in coinfected patients, consult a clinician with expertise in managing HBV infection.
Other Warnings and Precautions
Risk of Hepatic Decompensation or Failure in Patients with Evidence of Advanced Liver Disease
Postmarketing reports of hepatic decompensation or failure, including some fatalities, in patients receiving HCV treatment regimens containing an HCV NS3/4A protease inhibitor, including glecaprevir/pibrentasvir. Data insufficient to estimate frequency of such events; causal relationship not established. Hepatic decompensation or failure usually occurred within first 4 weeks of HCV treatment.
Majority of reported cases of hepatic decompensation or failure with severe outcomes in patients receiving glecaprevir/pibrentasvir occurred in those with evidence of advanced liver disease with moderate or severe hepatic impairment (Child-Pugh class B or C) prior to initiation of the drug. Some cases occurred in patients who had compensated cirrhosis with mild liver impairment (Child-Pugh class A) at baseline, but had a history of a decompensation event (i.e., history of ascites, variceal bleeding, encephalopathy). Rare cases of hepatic decompensation or failure reported in patients without cirrhosis or with compensated cirrhosis (Child-Pugh A); many of these patients had evidence of portal hypertension. Some cases also reported in patients receiving concomitant therapy with drugs not recommended for concomitant use with the HCV treatment regimen and in those with confounding factors (e.g., serious liver-related medical or surgical comorbidities).
If glecaprevir/pibrentasvir used in patients who have compensated cirrhosis (Child-Pugh class A) or evidence of advanced liver disease (e.g., portal hypertension), perform hepatic function tests as clinically indicated and monitor for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage).
Discontinue glecaprevir/pibrentasvir in patients who develop evidence of hepatic decompensation or failure.
Advise patients to contact a clinician if they develop any signs or symptoms of worsening liver disease.
Interactions
Concomitant use with certain drugs (i.e., carbamazepine, efavirenz, St. John's wort) may result in clinically important decreases in glecaprevir and pibrentasvir plasma concentrations leading to reduced therapeutic effect of glecaprevir/pibrentasvir. Concomitant use with such drugs not recommended.
Precautions Related to Fixed Combinations
Consider cautions, precautions, contraindications, and drug interactions associated with both drugs in the fixed combination. Consider cautionary information applicable to specific populations (e.g., pregnant or nursing women, individuals with hepatic or renal impairment, geriatric patients) for both glecaprevir and pibrentasvir.
Specific Populations
Pregnancy
Adequate data not available regarding use in pregnant women. In animal studies, no adverse effects on fetal development at glecaprevir or pibrentasvir exposures 53 or 51 times greater, respectively, than human exposures at recommended human dosage.
Lactation
Not known whether glecaprevir or pibrentasvir distribute into human milk, affect human milk production, or affect the breast-fed infant.
Glecaprevir and pibrentasvir distributed into milk in rodents; no apparent effects on growth and development observed in nursing pups.
Consider benefits of breast-feeding and importance of glecaprevir/pibrentasvir to the woman; also consider potential adverse effects on breast-fed child from the drug or underlying maternal condition.
Pediatric Use
Safety, efficacy, and pharmacokinetics not established in pediatric patients <3 years of age.
Safety and efficacy established in pediatric patients ≥3 years of age. Safety and efficacy generally consistent with those observed in HCV-infected adults, except for vomiting, rash, and abdominal pain, which occurred more frequently in patients <12 years of age compared to adults.
Use in pediatric patients with HCV genotype 5 or 6 infection and cirrhosis or those who received a kidney and/or liver transplant supported by data indicating that glecaprevir and pibrentasvir systemic exposures in pediatric patients are comparable to those reported in adults.
Geriatric Use
No overall differences in safety and efficacy observed between patients ≥65 years of age and younger adults.
In patients with severe renal impairment, higher incidence of adverse effects observed in patients ≥65 years of age compared with younger adults.
Hepatic Impairment
Mild hepatic impairment or compensated cirrhosis (Child-Pugh class A): Monitor for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage).
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation: Contraindicated. Postmarketing reports of hepatic decompensation or failure in such patients.
Increased glecaprevir and pibrentasvir exposures reported in patients with moderate or severe hepatic impairment.
Renal Impairment
Mild, moderate, and severe renal impairment: Glecaprevir and pibrentasvir AUCs up to 56% higher compared with normal renal function; AUCs not affected by dialysis.
HCV-infected with end-stage renal disease (ESRD): Glecaprevir and pibrentasvir AUCs 86 and 54% higher, respectively, compared with normal renal function.
Persons Who Inject Drugs (PWID) or Receive Medication-Assisted Treatment (MAT) for Opioid Use Disorder
No overall differences in safety and efficacy of glecaprevir/pibrentasvir between patients who self-identify as recent or current injection drug users and people who self-identify as former or noninjection drug users. Safety and efficacy also similar between patients who report and those who do not report concomitant use of MAT for opioid use disorder.
Common Adverse Effects
Adverse effects (≥10%): Headache, fatigue.
Drug Interactions
Glecaprevir and pibrentasvir are weak inhibitors of CYP3A and 1A2. Glecaprevir is a substrate of CYP3A.
Glecaprevir and pibrentasvir inhibit P-glycoprotein (P-gp) transport system and are substrates of P-gp.
Glecaprevir and pibrentasvir inhibit breast cancer resistance protein (BCRP) and are substrates of BCRP.
Glecaprevir and pibrentasvir inhibit organic anion transporting polypeptide (OATP) 1B1 and 1B3. Glecaprevir is a substrate of OATP1B1 and 1B3.
Glecaprevir and pibrentasvir are weak inhibitors of UGT1A1.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP3A, 1A2, 2C9, 2C19, or 2D6: Clinically important pharmacokinetic interactions not expected.
CYP3A4 inducers: Possible decreased glecaprevir and pibrentasvir plasma concentrations.
Drugs Affecting or Affected by P-glycoprotein Transport System
P-gp substrates: Possible increased plasma concentrations of P-gp substrates.
P-gp inducers: Possible decreased glecaprevir and pibrentasvir plasma concentrations.
P-gp inhibitors: Possible increased glecaprevir and pibrentasvir plasma concentrations.
Drugs Affecting or Affected by Breast Cancer Resistance Protein
BCRP substrates: Possible increased plasma concentrations of BCRP substrates.
BCRP inducers: Possible decreased glecaprevir and pibrentasvir plasma concentrations.
BCRP inhibitors: Possible increased glecaprevir and pibrentasvir plasma concentrations.
Drugs Affecting or Affected by Organic Anion Transporting Polypeptides
OATP1B1 or 1B3 substrates: Possible increased plasma concentrations of these substrates.
OATP1B1 or 1B3 inducers: Possible decreased glecaprevir plasma concentrations.
OATP1B1 or 1B3 inhibitors: Possible increased glecaprevir plasma concentrations.
Drugs Affecting or Affected by Other Membrane Transporters
UGT1A1 or 1A4 substrates: Clinically important pharmacokinetic interactions not expected.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Angiotensin II receptor antagonists |
Losartan, valsartan: No clinically important pharmacokinetic interactions |
Losartan, valsartan: Dosage adjustments not needed |
|
Anticonvulsants |
Carbamazepine: Clinically important decreases in glecaprevir and pibrentasvir concentrations and AUCs; possible reduced therapeutic effect of Lamotrigine: No clinically important pharmacokinetic interactions Phenytoin: May decrease glecaprevir and pibrentasvir concentrations; may result in loss of therapeutic effect |
Carbamazepine, phenytoin: Concomitant use not recommended Lamotrigine: Dosage adjustments not needed |
|
Antiretrovirals, HIV integrase inhibitors (INSTIs) |
Fixed combination of abacavir, dolutegravir, and lamivudine (abacavir/dolutegravir/lamivudine): No clinically important pharmacokinetic interactions Fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide fumarate (EVG/c/FTC/TAF): Increased concentrations and AUCs of glecaprevir and pibrentasvir Raltegravir: Increased raltegravir concentrations and AUC |
Dolutegravir: Dosage adjustments not needed Cobicistat-boosted elvitegravir: Dosage adjustments not needed Raltegravir: Dosage adjustments not needed |
|
Antiretrovirals, HIV nonnucleoside reverse transcriptase inhibitors (NNRTIs) |
Efavirenz: Decreased glecaprevir and pibrentasvir concentrations expected and possible reduced therapeutic effect Rilpivirine: Increased rilpivirine concentrations and AUC; |
Efavirenz: Concomitant use not recommended Rilpivirine: Dosage adjustments not needed |
|
Antiretrovirals, HIV nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs) |
Abacavir/dolutegravir/lamivudine: No clinically important pharmacokinetic interactions Abacavir/dolutegravir/lamivudine: No clinically important pharmacokinetic interactions EVG/c/FTC/TAF: Increased glecaprevir and pibrentasvir concentrations and AUCs; no effect on tenofovir concentrations or AUC Fixed combination of efavirenz, emtricitabine, and tenofovir disoproxil fumarate (TDF): Increased tenofovir concentrations and AUC |
Abacavir: Dosage adjustments not needed Emtricitabine: Dosage adjustments not needed Lamivudine: Dosage adjustments not needed TAF or TDF: Dosage adjustments not needed |
|
Antiretrovirals, HIV protease inhibitors (PIs) |
Ritonavir-boosted atazanavir: Increased glecaprevir and pibrentasvir concentrations and AUC; possible increased ALT concentrations Ritonavir-boosted darunavir: Increased glecaprevir concentrations and AUC and increased pibrentasvir concentrations Fixed combination of lopinavir and ritonavir (lopinavir/ritonavir): Increased glecaprevir and pibrentasvir concentrations and AUCs Ritonavir: Increased glecaprevir and pibrentasvir concentrations expected |
Cobicistat-boosted, ritonavir-boosted, or unboosted atazanavir: Concomitant use contraindicated Cobicistat-boosted or ritonavir-boosted darunavir: Concomitant use not recommended Lopinavir/ritonavir: Concomitant use not recommended Ritonavir: Concomitant use not recommended |
|
Benzodiazepines |
Midazolam: No clinically important pharmacokinetic interactions |
Midazolam: Dosage adjustments not needed |
|
Buprenorphine/naloxone |
Buprenorphine, naloxone, or fixed combination of buprenorphine and naloxone (buprenorphine/naloxone): No clinically important pharmacokinetic interactions |
Buprenorphine, naloxone, or buprenorphine/naloxone: Dosage adjustments not needed |
|
Caffeine |
No clinically important pharmacokinetic interactions |
Dosage adjustments not needed |
|
Calcium-channel blocking agents |
Amlodipine, felodipine: No clinically important pharmacokinetic interactions |
Amlodipine, felodipine: Dosage adjustments not needed |
|
Dabigatran |
Increased dabigatran concentrations and AUC |
If used concomitantly in patients with renal impairment, consult recommendations from manufacturer of dabigatran regarding dosage modifications for concomitant use with P-gp inhibitors |
|
Dextromethorphan |
No clinically important pharmacokinetic interactions |
Dosage adjustments not needed |
|
Digoxin |
Increased digoxin exposures |
Measure digoxin concentrations prior to and during glecaprevir/pibrentasvir therapy; decrease digoxin dosage by 50% or adjust frequency to reduce digoxin concentrations |
|
Estrogens |
Concomitant use of glecaprevir/pibrentasvir and an ethinyl estradiol-containing product (e.g., oral contraceptives) does not affect glecaprevir or pibrentasvir concentrations Coadministration of glecaprevir/pibrentasvir with products containing more than 20 mcg of ethinyl estradiol may increase the risk of ALT elevations and is not recommended |
No dose adjustment is required when glecaprevir/pibrentasvir is coadministered with products containing ≤20 mcg of ethinyl estradiol |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, pravastatin, rosuvastatin, simvastatin: Substantially increased statin concentrations and AUCs; possible increased risk of myopathy and rhabdomyolysis Fluvastatin, pitavastatin: Possible substantially increased statin concentrations and AUCs; possible increased risk of myopathy and rhabdomyolysis |
Atorvastatin, lovastatin, simvastatin: Concomitant use not recommended Fluvastatin, pitavastatin: Use lowest statin dosage; if higher dosages required, use lowest necessary dosage taking into account risks and benefits Pravastatin: Reduce pravastatin dosage by 50% Rosuvastatin: Do not exceed rosuvastatin dosage of 10 mg |
|
Immunosuppressive agents |
Cyclosporine: Increased glecaprevir concentrations and AUC and increased pibrentasvir concentrations and AUC; no substantial effect on cyclosporine exposure Tacrolimus: No clinically important pharmacokinetic interactions |
Cyclosporine: Concomitant use not recommended in patients receiving stable cyclosporine dosage >100 mg daily Tacrolimus: Dosage adjustments not needed |
|
Methadone |
No clinically important pharmacokinetic interactions |
Dosage adjustments not needed |
|
Naltrexone |
Insufficient data regarding concomitant use |
|
|
Proton-pump inhibitors (PPIs) |
No clinically important pharmacokinetic interactions with omeprazole 20 mg once daily; decreased glecaprevir concentrations and AUC with omeprazole 40 mg once daily, but no effect on pibrentasvir concentrations or AUC No evidence to date that PPIs affect efficacy of glecaprevir/pibrentasvir |
Omeprazole: Manufacturer states dosage adjustments not needed; some clinicians state avoid long-term concomitant use with omeprazole 40 mg once daily |
|
Rifampin |
Clinically important decreases in glecaprevir and pibrentasvir concentrations and AUC; may result in loss of therapeutic effect of glecaprevir/pibrentasvir |
Concomitant use contraindicated |
|
Sofosbuvir |
No clinically important pharmacokinetic interactions |
Dosage adjustments not needed |
|
St. John's Wort (Hypericum perforatum) |
Possible substantially decreased glecaprevir and pibrentasvir concentrations; may result in loss of therapeutic effect of glecaprevir/pibrentasvir |
Concomitant use not recommended |
|
Warfarin |
Possible INR fluctuations |
Closely monitor INR; may need to adjust warfarin dosage |
Glecaprevir And Pibrentasvir Pharmacokinetics
Absorption
Bioavailability
Following oral administration of glecaprevir/pibrentasvir tablets in healthy individuals, peak plasma concentrations of glecaprevir and pibrentasvir occur 5 hours after the dose.
Following oral administration of glecaprevir/pibrentasvir oral pellets in healthy individuals, peak plasma concentrations of glecaprevir and pibrentasvir occur 3 and 5 hours, respectively, after the dose.
Food
Administration of glecaprevir/pibrentasvir tablets with a low/moderate- to high-fat meal increases glecaprevir exposures by 83–163% and increases pibrentasvir exposures by 40–53% relative to administration in the fasting state.
Administration of glecaprevir/pibrentasvir oral pellets with a low/moderate- to high-fat meal increased systemic exposure of glecaprevir and pibrentasvir by 131–167% and 56–114%, respectively, compared with the fasting state.
Special Populations
HCV-infected patients with compensated cirrhosis (Child-Pugh class A): Glecaprevir exposures approximately twofold higher than those reported in HCV-infected individuals without cirrhosis; pibrentasvir exposures similar to those in HCV-infected individuals without cirrhosis.
Moderate hepatic impairment (Child-Pugh class B): Glecaprevir exposures twofold higher and pibrentasvir exposures 26% higher than those in individuals with normal hepatic function.
Severe hepatic impairment (Child-Pugh class C): Glecaprevir exposures 11-fold higher and pibrentasvir exposures 114% higher than those in individuals with normal hepatic function.
Mild, moderate, severe, or ESRD without HCV infection: Glecaprevir and pibrentasvir exposures up to 56 and 46% higher, respectively, than those in individuals with normal renal function. In dialysis-dependent individuals, pibrentasvir and glecaprevir exposures similar with or without dialysis (up to 18% difference).
HCV-infected with ESRD (with or without dialysis): Glecaprevir and pibrentasvir exposures 86 and 54% higher, respectively, than reported in individuals with normal renal function.
Pediatric patients ≥3 years of age: Glecaprevir and pibrentasvir AUC and peak plasma concentrations comparable to those observed in adults.
Pediatric patients <3 years of age: Pharmacokinetics not studied.
Distribution
Plasma Protein Binding
Glecaprevir: 97.5%.
Pibrentasvir: >99.9%.
Elimination
Metabolism
Glecaprevir: Metabolized to some extent by CYP3A.
Pibrentasvir: None.
Elimination Route
Glecaprevir: Biliary and fecal excretion. Following a single dose, 92.1% excreted in feces and 0.7% eliminated in urine.
Pibrentasvir: Biliary and fecal excretion. Following a single dose, 96.6% excreted in feces; no drug eliminated in urine.
Half-life
Glecaprevir: 6 hours.
Pibrentasvir: 13 hours.
Stability
Storage
Oral
Pellets
≤30°C.
Tablets
≤30°C.
Actions and Spectrum
-
Glecaprevir/pibrentasvir is a fixed combination containing 2 HCV antivirals. Glecaprevir is an HCV NS3/4A protease inhibitor and pibrentasvir is an HCV NS5A replication complex inhibitor (NS5A inhibitor).
-
Glecaprevir and pibrentasvir are both direct-acting antivirals (DAAs) with activity against HCV. No in vitro evidence of antagonistic anti-HCV effects between the drugs in replicon studies.
-
Glecaprevir binds to the active site of HCV NS3/4A protease, thereby blocking enzyme activity essential for viral replication (i.e., blocking cleavage of the HCV-encoded polyproteins into mature forms of NS3, NS4A, NS4B, NS5A, and NS5B). In vitro studies using biochemical assays indicate that glecaprevir has activity against clinical isolates of HCV genotypes 1a, 1b, 2a, 2b, 3a, 4a, 5a, and 6a.
-
Pibrentasvir inhibits the HCV NS5A protein, which is required for viral replication and virion assembly. In HCV replicon assays, pibrentasvir has shown in vitro activity against laboratory and clinical isolates of HCV genotypes 1a, 1b, 2a, 2b, 3a, 4a, 4b, 4d, 5a, 6a, 6e, and 6p.
-
Certain amino acid substitutions in NS3/4A protease inhibitor resistance-associated positions of HCV genotypes 1a (e.g., D168F/Y), 1b, 2a, 3a (e.g., Q168R), 4a, and 6a (e.g., D168A/G/H/V/Y) have been selected in cell culture and have been associated with reduced susceptibility to glecaprevir in vitro in replicon studies. Emergence of amino acid substitutions occurred most commonly at NS3 positions A156 or D/Q168. The combination of NS3 resistance-associated substitutions Y56H and D/Q168 resulted in greater reductions in glecaprevir susceptibility. Treatment-emergent NS3 resistance-associated substitutions were detected in clinical trials evaluating glecaprevir/pibrentasvir in patients with HCV genotype 1 (e.g., A156V, V36A/M, Y56H, R155K/T, A156G/T/V, D168A/T) or genotype 3 (e.g., Y56H/N, Q80K/R, A156G, Q168L/R) infection who experienced virologic failure.
-
Certain amino acid substitutions in NS5A of HCV genotype 1a (e.g., Q30D/deletion, Y93D/H/N, H58D and Y93H, M28G), genotype 1b (e.g., P32-deletion), genotype 2a (e.g., F28S and M31I, P29S and K30G), and genotype 3a (e.g., K30, M31,Y93H) have been selected in cell culture and have been associated with reduced susceptibility to pibrentasvir in vitro in replicon studies. Combinations of these NS5A substitutions often resulted in greater reductions in susceptibility to pibrentasvir compared with a single NS5A substitution. Treatment-emergent NS5A resistance-associated substitutions were detected in clinical trials evaluating glecaprevir/pibrentasvir in patients with HCV genotype 1 (e.g., Q30R, L31M, M28A/G, L28M, P29Q/R, Q30K/R, H58D, Y93H/N) or genotype 3a (e.g., S24F, M28G/K, A30G/K, L31F, P58T, Y93H) infection who experienced virologic failure. Some of these patients also had baseline NS5A polymorphisms at resistance-associated amino acid positions.
-
Cross-resistance is possible between glecaprevir and other HCV NS3/4A protease inhibitors and between pibrentasvir and other HCV NS5A inhibitors. Cross-resistance not expected between glecaprevir/pibrentasvir and sofosbuvir, peginterferon, or ribavirin.
Advice to Patients
-
Advise patients to read the patient information provided by the manufacturer.
-
Advise patients that glecaprevir/pibrentasvir should be taken once daily with food on a regular dosing schedule.
-
Advise patients or their caregivers to read and follow the manufacturer's instructions to prepare the correct dose of glecaprevir/pibrentasvir oral pellets.
-
Importance of taking the recommended dosage of glecaprevir/pibrentasvir for the recommended duration of treatment; importance of not missing doses.
-
If a dose is missed and remembered <18 hours after scheduled administration time, take glecaprevir/pibrentasvir as soon as possible and then take the next dose at the usual time. If a dose is missed and remembered >18 hours after schedule administration time, skip the missed dose and take the next dose at the usual time.
-
Inform patients that reactivation of HBV infection has occurred in patients being treated for HCV infection who were coinfected with HBV. Importance of informing clinician of any history of HBV infection or other liver problems (e.g., cirrhosis). Importance of immediately contacting a clinician if any signs or symptoms of serious liver injury (e.g., fatigue, weakness, loss of appetite, nausea and vomiting, yellowing of the eyes or skin, light-colored bowel movements) occur.
-
Advise patients to immediately contact a clinician if they have symptoms of worsening liver problems (e.g., nausea, tiredness, yellowing of skin or white part of the eyes, bleeding or bruising more easily than normal, confusion, loss of appetite, diarrhea, dark or brown urine, dark or bloody stool, abdominal swelling, pain in upper right side of stomach area, sleepiness, vomiting of blood).
-
Advise patients that glecaprevir/pibrentasvir may interact with some drugs. Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Pellets |
Glecaprevir 50 mg and Pibrentasvir 20 mg |
Mavyret |
AbbVie |
|
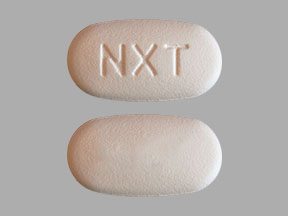
Tablets, film-coated |
Glecaprevir 100 mg and Pibrentasvir 40 mg |
Mavyret |
AbbVie |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What are the new drugs for the treatment of hepatitis C?
- Does Mavyret cure hep C (HCV)? What is the success rate?
- Can you take antibiotics with Mavyret?
- Does Mavyret cause itching?
- What types of Hepatitis C does Mavyret treat?
More about glecaprevir / pibrentasvir
- Check interactions
- Compare alternatives
- Reviews (431)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
- En español