PHENobarbital, PHENobarbital Sodium (Systemic) (Sedative) (Monograph)
Brand name: Luminal
Drug class: Barbiturates
Introduction
Barbiturate; anxiolytic, sedative, hypnotic, and anticonvulsant.
Uses for PHENobarbital, PHENobarbital Sodium (Systemic) (Sedative)
Insomnia and Anxiety
Relief of anxiety, tension, and apprehension. However, barbiturates used infrequently for routine sedation, since there are few clinical situations in which oral barbiturates provide a safety or efficacy advantage over nonbarbiturate sedatives/hypnotics.
Short-term treatment of insomnia. However, generally not used orally as a hypnotic because several hours are required to achieve maximal effects and barbiturates have decreased effectiveness for sleep induction and maintenance after 2 weeks.
Drug Withdrawal
Withdrawal of barbiturate or nonbarbiturate hypnotics in patients who are physically dependent on these drugs.
Surgery
Preoperatively, to produce sedation and relieve anxiety.
Seizure Disorders
Management of tonic-clonic seizures and partial seizures; used alone (particularly in infants and young children) or, more commonly, in combination with phenytoin or other anticonvulsants.
Prevention of febrile seizures in infants and young children.
Second-line agent in the termination of status epilepticus; may be useful to prevent seizure recurrence after seizures are initially terminated with other anticonvulsants (e.g., diazepam, phenytoin) or for termination of status epilepticus that does not respond to initial therapy with other anticonvulsants. Usefulness of parenteral phenobarbital in terminating acute seizure episodes is limited by its slow onset of action.
Prophylactic management of epilepsy.
Hyperbilirubinemia in Neonates
Prevention and treatment of hyperbilirubinemia in neonates† [off-label].
Cholestasis
Has been used to reduce bilirubin concentrations in patients with congenital nonhemolytic unconjugated hyperbilirubinemia† [off-label] or chronic intrahepatic cholestasis† [off-label].
Has been used in the management of hyperlipemia associated with intrahepatic and extrahepatic cholestasis† [off-label].
PHENobarbital, PHENobarbital Sodium (Systemic) (Sedative) Dosage and Administration
General
-
Adjust dosage carefully and slowly according to individual requirements and response.
-
Following chronic administration, withdraw phenobarbital slowly to avoid the possibility of precipitating withdrawal symptoms if the patient is physically dependent on the drug.
-
To prevent rebound in rapid eye movement (REM) sleep, withdrawal of a single therapeutic dose over 5 or 6 days (e.g., reducing dosage from 3 to 2 doses daily for 1 week) has been recommended when barbiturates are discontinued following prolonged use.
Seizures
-
2–3 weeks of therapy may be required to achieve full anticonvulsant effects.
-
When transferring a patient to another anticonvulsant drug, reduce phenobarbital dosage gradually over 1 week while, at the same time, instituting therapy with a low dose of the replacement drug.
-
Withdraw phenobarbital or reduce dosage slowly to avoid precipitating seizures or status epilepticus.
Insomnia
-
Do not administer for periods >2 weeks.
Administration
Administer orally or by IM or slow IV injection. Sub-Q injection not recommended.
Oral Administration
Frequently administered in 2 or 3 divided doses; however, there is no advantage in dividing the daily dosage (because of the long half-life).
IV Administration
Reserve IV administration for emergency treatment of acute seizure states; however, usefulness in these conditions is limited. (See Seizure Disorders under Uses.)
Patient should be hospitalized and under close supervision.
To minimize the risk of irritation and thrombosis, do not use small veins (e.g., those on the dorsum of the hands or wrist).
Avoid intra-arterial injection. (See Intra-arterial Injection under Cautions.)
Rate of Administration
≤60 mg/minute.
IM Administration
Maximum volume of single injections is 5 mL; administer deeply into a large muscle to avoid tissue irritation.
Dosage
Available as phenobarbital sodium; dosage expressed in terms of the salt.
Pediatric Patients
Anxiety
Oral
6 mg/kg daily or 180 mg/m2 daily, in 3 equally divided doses.
Surgery
Oral
1–3 mg/kg preoperatively.
IM
16–100 mg administered 60–90 minutes before surgery; alternatively, 1–3 mg/kg preoperatively.
Drug Withdrawal
Oral
Infants: 3–10 mg/kg daily. After symptoms are relieved, decrease dosage gradually and withdraw drug completely over a 2-week period.
Seizure Disorders
Oral
15–50 mg 2 or 3 times daily. Alternatively, 3–5 mg/kg or 125 mg/m2 daily.
IV or IM
4–6 mg/kg daily for 7–10 days to reach therapeutic blood concentrations; alternatively, 10–15 mg/kg daily.
Prevention of Febrile Seizures
Oral3–4 mg/kg daily.
Status Epilepticus
IV or IM15–20 mg/kg IV over 10–15 minutes. Alternatively 100–400 mg IM or IV; allow up to 30 minutes for maximum anticonvulsant effect before administering additional doses (to prevent overdosage).
Hyperbilirubinemia in Neonates† [off-label]
Oral
7 mg/kg per day from the first to fifth day of life.
IM, then Oral
5 mg/kg IM on the first day of life, followed by 5 mg/kg orally on the second to seventh day.
Cholestasis†
Oral
Children <12 years of age: Dosages of 3–12 mg/kg daily in 2 or 3 divided doses have been used.
Adults
Insomnia and Anxiety
Anxiety
Oral30–120 mg daily.
Insomnia
Oral100–320 mg.
IM100–320 mg.
Drug Withdrawal
Oral
30-mg dose for each 100- to 200-mg dose of the barbiturate or nonbarbiturate hypnotic that the patient has been taking daily, administered in 3 or 4 divided doses. If the patient shows signs of withdrawal on the first day, a loading dose of 100–200 mg of phenobarbital sodium may be administered IM in addition to the oral dose.
After stabilization on phenobarbital sodium, decrease the total daily dose of phenobarbital sodium by 30 mg per day. After withdrawal symptoms are relieved, gradually decrease dosage and withdraw completely over a 2-week period.
Surgery
IM
100–200 mg given 60–90 minutes before surgery.
Seizure Disorders
Oral
100–300 mg daily, usually at bedtime.
Status Epilepticus
IV or IM20–320 mg; repeat in 6 hours, if necessary. Alternatively, 200–600 mg; allow up to 30 minutes for maximum anticonvulsant effect before administering additional doses (to prevent overdosage).
Some clinicians administer phenobarbital sodium IV until seizures stop or a total dose of 20 mg/kg has been given. Discontinue IV injections as soon as the desired effect is obtained.
Cholestasis†
Oral
Dosages of 90–180 mg daily in 2 or 3 divided doses have been used.
Special Populations
Hepatic Impairment
Dosage reduction recommended in patients with hepatic impairment; avoid use in patients with marked hepatic impairment.
Renal Impairment
Dosage reduction recommended.
Geriatric Patients
Dosage reduction recommended.
Cautions for PHENobarbital, PHENobarbital Sodium (Systemic) (Sedative)
Contraindications
-
Known hypersensitivity to any barbiturates.
-
Respiratory disease in which dyspnea or obstruction is evident.
-
Marked impairment of hepatic function.
-
History of manifest or latent porphyria (due to potential for exacerbation of acute intermittent porphyria or porphyria variegata).
-
Previous addiction to sedative and/or hypnotic drugs.
Warnings/Precautions
Warnings
Pain Reaction
Potential for paradoxical excitement and/or euphoria, restlessness, or delirium in patients with severe pain. Barbiturates could mask important symptoms in patients with acute or chronic pain. Use with caution in such patients. Should not be used to relieve pain or to produce sedation or sleep in the presence of uncontrolled pain.
Abuse Potential
Possible tolerance, psychologic dependence, and physical dependence. (See Contraindications under Cautions.)
Withdrawal Effects
Abrupt cessation after prolonged use in dependent individuals may result in withdrawal symptoms (e.g., delirium, convulsions) and potentially be fatal. Drug must be withdrawn gradually in patients receiving excessive dosages over extended periods of time.
CNS Depression
Performance of activities requiring mental alertness and physical coordination may be impaired.
Concurrent use of other CNS depressants may potentiate CNS depression. (See Specific Drugs under Interactions.)
Respiratory and Cardiovascular Effects
Possible respiratory depression, apnea, laryngospasm, hypertension, or vasodilation and hypotension, particularly if phenobarbital is administered IV too rapidly. Administer slowly; personnel and equipment should be readily available for administration of artificial respiration.
Sensitivity Reactions
Dermatologic Effects and Hypersensitivity Reactions
Exfoliative dermatitis (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis), sometimes fatal, reported rarely. Because skin eruptions can precede potentially fatal reactions, discontinue phenobarbital whenever dermatologic reactions occur.
Hypersensitivity reactions (e.g., localized swelling, particularly of the eyelids, cheeks, or lips; erythematous dermatitis) may occur, particularly in patients with a history of asthma, urticaria, or angioedema.
General Precautions
Intra-arterial Injection
Inadvertent intra-arterial administration can cause spasm and severe pain along the affected artery, resulting in local reactions varying in severity from transient pain to gangrene.
Discontinue injection if the patient complains of pain or if signs of inadvertent intra-arterial injection (e.g., patches of discolored skin, a white hand with cyanosed skin, delayed onset of action) occur. Appropriate therapy for such inadvertent injection has not been fully established; consult manufacturers’ labeling for current recommendations.
Suicide
Use with caution, if at all, in depressed patients; potential for suicidal tendencies. Prescribe drug in the smallest feasible quantity.
Concomitant Diseases
Use parenterally with extreme caution in debilitated patients or patients with severe hepatic impairment, pulmonary or cardiac disease, status asthmaticus, uremia, or shock.
Specific Populations
Pregnancy
Tablets: Category B. Injection: Category D.
Barbiturates have caused postpartum hemorrhage and hemorrhagic disease in neonates; readily reversible with vitamin K therapy.
Possible withdrawal symptoms in neonates born to women who received barbiturates throughout the last trimester of pregnancy. Premature neonates are particularly susceptible to the depressant effects of barbiturates.
Lactation
Distributed into milk; use with caution.
Pediatric Use
May produce paradoxical excitement and hyperactivity or exacerbate existing hyperactivity; if severe, substitute another barbiturate or therapeutic agent.
Possible behavioral (e.g., hyperactivity, fussiness, lethargy, disturbed sleep, irritability, disobedience, stubbornness, depressive symptoms) or cognitive effects (e.g., deficits on neuropsychiatric tests, impaired short-term memory and memory concentration tasks) associated with anticonvulsant use. If such changes occur and alternative causes are not readily evident, consider the possibility that anticonvulsant therapy may be responsible and the need for dosage reduction or substitution of alternative anticonvulsant(s).
Phenobarbital sodium injection contains benzyl alcohol. Manufacturer does not recommend use in neonates; AAP states that the presence of small amounts of this preservative in a commercially available injection should not proscribe its use when indicated in neonates.
Geriatric Use
Possible increased sensitivity to barbiturates. Geriatric patients may frequently react to barbiturates with excitement, confusion, or depression.
Hepatic Impairment
Use with caution; should not be used in patients with marked hepatic impairment. (See Contraindications under Cautions.)
Renal Impairment
Use with extreme caution in patients with nephritis. Use parenterally with extreme caution in patients with uremia.
Common Adverse Effects
Residual sedation, drowsiness, lethargy, vertigo, nausea, vomiting, headache.
Drug Interactions
Metabolized by hepatic microsomal enzymes. Induces hepatic microsomal enzymes.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants, oral (e.g., warfarin) |
Possible decreased plasma warfarin concentrations |
Monitor PT; adjust anticoagulant dosage as necessary, especially with initiation or discontinuance of phenobarbital |
|
Antidepressants, tricyclics |
Antidepressant may precipitate seizures, resulting in decreased seizure control Potentiation of respiratory depression following toxic doses of tricyclic antidepressants |
Monitor epileptic patients for decreased seizure control following initiation of antidepressant therapy; adjust phenobarbital dosage, if necessary |
|
CNS depressants (e.g., sedatives, hypnotics, antihistamines, tranquilizers, alcohol) |
Possible additive depressant effects |
|
|
Contraceptives, oral |
Possible enhanced metabolism of estrogenic and progestinic components; potential for decreased oral contraceptive effectiveness and increased risk of pregnancy with phenobarbital pretreatment or concurrent therapy |
Consider alternate methods of contraception |
|
Corticosteroids |
Possible increased corticosteroid metabolism |
Dosage adjustment of corticosteroid may be required; closely monitor asthmatics receiving corticosteroids when phenobarbital is initiated |
|
Doxycycline |
Possible decreased half-life of doxycycline; effect may persist up to 2 weeks after discontinuance of phenobarbital |
If possible, avoid concomitant administration; if administered concomitantly, monitor clinical response to doxycycline |
|
Griseofulvin |
Possible decreased griseofulvin absorption, resulting in decreased blood concentrations |
Avoid concomitant administration; if concomitant therapy is necessary, administration of griseofulvin in 3 divided daily doses may improve absorption. Monitor blood griseofulvin concentrations and increase dosage, if necessary |
|
MAO inhibitors |
Possible prolongation of phenobarbital effects |
Dosage adjustment of phenobarbital may be required |
|
Phenytoin |
Increased, decreased, or no change in plasma phenytoin concentrations reported |
Monitor plasma concentrations of phenytoin and phenobarbital; adjust dosages as necessary |
|
Valproic acid |
Possible increased plasma phenobarbital concentrations |
Monitor plasma phenobarbital concentrations and adjust dosage as needed |
PHENobarbital, PHENobarbital Sodium (Systemic) (Sedative) Pharmacokinetics
Absorption
Bioavailability
Slowly absorbed from GI tract following oral administration, with peak plasma concentrations usually attained within 8–12 hours and peak brain concentrations in 10–15 hours.
Following IV administration, ≥15 minutes may be required to reach peak brain concentrations.
Onset
Following oral administration, onset occurs within 30 minutes.
Following IV administration, onset occurs within 5 minutes, with maximum CNS depression occurring ≥15 minutes after administration. Onset is slower following IM administration.
Duration
About 5–6 hours or 4–6 hours following oral or parenteral administration, respectively.
Plasma Concentrations
Plasma concentrations of 10–25 mcg/mL associated with anticonvulsant activity in most patients. Concentrations >50 mcg/mL may produce coma; concentrations >80 mcg/mL are potentially lethal.
Distribution
Extent
Rapidly distributed to all tissues and fluids, with high concentrations in the brain, liver, and kidneys.
Crosses the placenta and is distributed into milk.
Plasma Protein Binding
20–45%.
Elimination
Metabolism
Metabolized primarily by hepatic microsomal enzymes.
Elimination Route
Excreted principally in urine (25–50% as unchanged drug).
Half-life
Adults: 53–118 hours.
Children and neonates: 60–180 hours.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 15–30°C. Protect from moisture.
Elixir
Tight containers at 20–25°C.
Parenteral
Injection
15–30°C.
Actions
-
CNS effects appear to be related, at least partially, to the drug’s ability to enhance activity of GABA, the principal inhibitory neurotransmitter in the CNS, by altering inhibitory synaptic transmissions that are mediated by GABAA receptors.
-
Capable of producing all levels of CNS depression—from mild sedation to hypnosis to deep coma to death.
-
Anticonvulsant effects of barbiturates are multiple and rather nonselective. Principal mechanism of action appears to be reduction of monosynaptic and polysynaptic transmission resulting in decreased excitability of the entire nerve cell; barbiturates also increase the threshold for electrical stimulation of the motor cortex.
-
Barbiturates lower serum bilirubin concentrations in neonates and patients with congenital nonhemolytic unconjugated hyperbilirubinemia, presumably by induction of glucuronyl transferase, the enzyme that conjugates bilirubin.
Advice to Patients
-
Potential for phenobarbital to impair mental alertness or physical coordination; do not drive or operate machinery until effects on individual are known.
-
Importance of taking exactly as prescribed; do not exceed the recommended dosage.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and alcohol consumption. Importance of avoiding alcohol while taking the drug.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as schedule IV (C-IV) drugs.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
30 mg/mL* |
Phenobarbital Sodium Injection (C-IV) |
Wyeth |
|
60 mg/mL* |
Phenobarbital Sodium Injection (C-IV) |
Wyeth |
||
|
65 mg/mL* |
Phenobarbital Sodium Injection (C-IV) |
Baxter |
||
|
130 mg/mL* |
Luminal Sodium (C-IV) |
Sanofi-Aventis |
||
|
PHENobarbital Sodium Injection (C-IV) |
Wyeth |
|||
|
Phenobarbital Sodium Injection (C-IV) |
Baxter |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about phenobarbital
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (38)
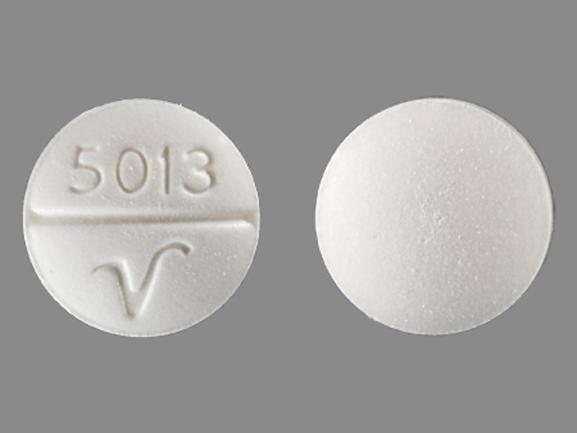
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: barbiturate anticonvulsants
- Breastfeeding
- En español
Patient resources
Professional resources
- PHENobarbital, PHENobarbital Sodium (Anticonvulsant) monograph
- Phenobarbital (FDA)
- Phenobarbital Elixir (FDA)
- Phenobarbital Oral Solution (FDA)
- Phenobarbital Sodium Injection (FDA)
- Phenobarbital Tablets (FDA)