Modafinil (Monograph)
Brand name: Provigil
Drug class: Wakefulness-promoting Agents
VA class: CN809
Chemical name: 2-((Diphenylmethyl)sulfinyl)acetamide
Molecular formula: C15H15NO2S
CAS number: 68693-11-8
Introduction
Wakefulness-promoting agent. 50:50 racemic mixture of the R- and S-enantiomers; the R-enantiomer of modafinil also is commercially available as armodafinil.
Uses for Modafinil
Narcolepsy
Symptomatic treatment of narcolepsy to improve wakefulness in adults with excessive daytime sleepiness.
Careful attention to diagnosis and treatment of the sleep disorder is essential. (See Diagnosis of Sleep Disorders under Cautions.)
Obstructive Sleep Apnea/Hypopnea Syndrome (OSAHS)
Symptomatic treatment (in combination with standard treatment[s] for underlying obstruction) of OSAHS to improve wakefulness in adults with excessive sleepiness.
If continuous positive airway pressure (CPAP) is the treatment of choice for a patient, make every effort to optimize treatment with CPAP for an adequate period prior to initiating modafinil. If modafinil is used adjunctively with CPAP, encourage and periodically assess CPAP compliance.
Careful attention to diagnosis and treatment of the sleep disorder is essential. (See Diagnosis of Sleep Disorders under Cautions.)
Shift Work Sleep Disorder (SWSD)
Symptomatic treatment of SWSD to improve wakefulness in adults with excessive sleepiness.
Careful attention to diagnosis and treatment of the sleep disorder is essential. (See Diagnosis of Sleep Disorders under Cautions.)
Modafinil Dosage and Administration
Administration
Oral Administration
Administer orally once daily without regard to meals. (See Food under Pharmacokinetics.)
In patients with narcolepsy or OSAHS, usually administer as a single dose in the morning. In patients with SWSD, administer dose approximately 1 hour prior to start of work shift.
In patients with narcolepsy, modafinil also has been administered in 2 divided doses daily, in the morning and at noon† [off-label].
Dosage
Adults
Narcolepsy
Oral
200 mg once daily.
Dosages up to 400 mg daily have been well tolerated, but may not provide additional clinical benefit beyond 200-mg daily dosage.
Long-term efficacy (>9 weeks) not systematically established. If clinician elects to prescribe for an extended period, periodically reassess long-term usefulness in the individual patient.
OSAHS
Oral
200 mg once daily.
Dosages up to 400 mg daily have been well tolerated, but may not provide additional clinical benefit beyond 200-mg daily dosage.
Long-term efficacy (>12 weeks) not systematically established. If clinician elects to prescribe for an extended period, periodically reassess long-term usefulness in the individual patient.
SWSD
Oral
200 mg once daily.
Dosages up to 400 mg daily have been well tolerated, but may not provide additional clinical benefit beyond 200-mg daily dosage.
Long-term efficacy (>12 weeks) not systematically established. If clinician elects to prescribe for an extended period, periodically reassess long-term usefulness in the individual patient.
Special Populations
Hepatic Impairment
Reduce dosage to 100 mg daily in patients with severe hepatic impairment (with or without cirrhosis). (See Hepatic Impairment under Cautions.)
Renal Impairment
Current information inadequate to make specific dosage recommendations in patients with severe renal impairment. (See Renal Impairment under Cautions.)
Geriatric Patients
Consider use of lower than usual recommended dosage. (See Geriatric Use under Cautions.)
Cautions for Modafinil
Contraindications
-
Known hypersensitivity to modafinil, armodafinil, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Serious Dermatologic Reactions
Serious skin rash (e.g., Stevens-Johnson syndrome [SJS]) requiring hospitalization and drug discontinuance reported in adult and pediatric patients receiving modafinil.
Severe rash (e.g., possible SJS, multiorgan hypersensitivity reaction), sometimes associated with fever and other abnormalities (e.g., vomiting, leukopenia), reported in pediatric clinical trials. No serious rashes reported in clinical trials in adults. Serious or life-threatening rash (e.g., SJS, toxic epidermal necrolysis [TEN], drug rash with eosinophilia and systemic symptoms [DRESS]) reported rarely during postmarketing experience. Modafinil is not approved for use in pediatric patients for any indication. (See Pediatric Use under Cautions.)
No known risk factors predict the occurrence or severity of rash. Nearly all cases occurred within 1–5 weeks following initiation of therapy, but cases also reported after prolonged (e.g., 3 months) treatment.
Benign rashes also occur with modafinil; not possible to predict which rashes will become serious. Therefore, discontinue drug at first sign of rash unless clearly not drug related. (See Advice to Patients.) Rash may become potentially life-threatening or permanently disabling or disfiguring despite drug discontinuance.
Persistent Sleepiness
In patients with abnormal levels of sleepiness, level of wakefulness may improve with modafinil therapy, but may not return to normal. (See Advice to Patients.)
Frequently reassess degree of sleepiness, and, if appropriate, advise patients to avoid driving or other potentially dangerous activity. Patients may not acknowledge sleepiness or drowsiness until directly questioned about these symptoms during specific activities. (See Advice to Patients.)
Psychiatric Effects
Adverse psychiatric effects (e.g., mania, delusions, hallucinations, suicidal ideation, aggression), sometimes resulting in hospitalization, reported in modafinil-treated patients; many, but not all, patients had a psychiatric history.
In controlled clinical trials, psychiatric symptoms that required treatment discontinuance in ≥0.3% of patients and more often for modafinil than for placebo included anxiety, nervousness, insomnia, confusion, agitation, and depression.
Use with caution in patients with a history of psychosis, depression, or mania.
Some clinicians recommend careful monitoring of patients receiving modafinil or other CNS stimulants for possible psychiatric effects. If psychiatric symptoms develop, consider drug discontinuance. (See Advice to Patients.)
Sensitivity Reactions
Angioedema and Anaphylactoid Reactions
Angioedema and hypersensitivity (with rash, dysphagia, and bronchospasm) reported with armodafinil. Angioedema also reported during postmarketing experience with modafinil.
Immediately discontinue therapy if any signs or symptoms of angioedema or anaphylaxis (e.g., swelling of face, eyes, lips, tongue, or larynx; difficulty swallowing or breathing; hoarseness) develop.
Multiorgan Hypersensitivity Reactions
Multiorgan hypersensitivity reactions, including at least 1 fatality, reported with modafinil.
Reactions detected a median of 13 days (range: 4–33 days) after initiation of modafinil. Clinical presentation was variable but typically included fever and rash associated with other organ system involvement (e.g., myocarditis, hepatitis, liver function test abnormalities, hematologic abnormalities [e.g., eosinophilia, leukopenia, thrombocytopenia], pruritus, asthenia).
No risk factors known to predict occurrence or severity.
If a multi-organ hypersensitivity reaction is suspected, discontinue therapy. Cross-sensitivity with other drugs that produce this syndrome not yet reported but is possible.
General Precautions
Diagnosis of Sleep Disorders
Use only in patients who have had a complete evaluation (e.g., complete history, physical examination, testing in a laboratory setting [polysomnography]) of excessive sleepiness and in whom a diagnosis of narcolepsy, OSAHS, and/or SWSD has been made in accordance with International Classification of Sleep Disorders (ICSD) or DSM diagnostic criteria.
Consider that >1 sleep disorder may contribute to excessive sleepiness in some patients (e.g., OSAHS and SWSD concurrently in the same patient).
Cognitive/Psychomotor Impairment
Although modafinil has not been shown to cause functional impairment, altered judgment, thinking, or motor skills is possible with any drug affecting the CNS. (See Advice to Patients.)
Continuous Positive Airway Pressure (CPAP) in OSAHS
In OSAHS, modafinil is indicated as an adjunct to standard treatment(s) for the underlying obstruction. If CPAP is the treatment of choice, make a maximal effort to treat with CPAP for an adequate period of time prior to initiating modafinil therapy. If modafinil is used adjunctively with CPAP, encourage and periodically assess CPAP compliance. (See Advice to Patients.)
Cardiovascular Effects
Adverse cardiovascular effects (e.g., chest pain, palpitations, dyspnea, transient ischemic T-wave changes on ECG) reported in several modafinil-treated patients in association with mitral valve prolapse or left ventricular hypertrophy.
Not recommended in patients with history of left ventricular hypertrophy or in patients with mitral valve prolapse who have experienced mitral valve prolapse syndrome (e.g., ischemic ECG changes, chest pain, arrhythmia) with previous CNS stimulant use. If new onset of any of these symptoms of mitral valve prolapse syndrome occurs during modafinil therapy, consider cardiac evaluation.
Use with caution in patients with recent history of MI or unstable angina.
A greater proportion of modafinil-treated patients required new or increased use of antihypertensive medication compared with those receiving placebo in a retrospective analysis (2.4 and 0.7%, respectively). Increased monitoring of BP may be appropriate during therapy.
Abuse and Misuse Potential
Modafinil is subject to control as a schedule IV (C-IV) drug.
Produces psychoactive and euphoric effects, and alterations in mood, perception, thinking, and feelings similar to those observed with other CNS stimulants (e.g., amphetamines, methylphenidate), but current evidence indicates risk of abuse or misuse is lower with modafinil than with schedule II CNS stimulants (e.g., amphetamine, methylphenidate). (See Actions.)
Monitor patients closely during treatment for possible signs of misuse or abuse (e.g., incrementation of doses, drug-seeking behavior), particularly in those with history of drug or stimulant abuse (e.g., amphetamine, cocaine, methylphenidate).
Contraceptive Precautions
Possible reduced efficacy of hormonal contraceptives during and for 1 month after discontinuance of therapy. Alternative or concomitant nonhormonal contraceptive methods recommended during these periods. (See Specific Drugs under Interactions and see Advice to Patients.)
Drug Interaction with Cyclosporine
Possible reduced blood cyclosporine concentrations when given concurrently with modafinil. (See Specific Drugs under Interactions.)
Specific Populations
Pregnancy
Category C.
Provigil Pregnancy Registry (for clinicians or patients) at 866-404-4106, or [Web].
Lactation
Not known whether modafinil or its metabolites are distributed into milk. Caution if used in nursing women.
Pediatric Use
Modafinil is not approved for use in pediatric patients for any indication, including attention deficit hyperactivity disorder (ADHD). Safety and efficacy not established in children <17 years of age.
Serious skin rashes (e.g., erythema multiforme, Stevens-Johnson syndrome) associated with use of modafinil in pediatric patients. (See Serious Dermatologic Reactions under Cautions.)
Geriatric Use
Limited experience indicates that the incidence of adverse effects in patients >65 years of age is similar to that in younger patients.
Elimination of modafinil and its metabolites may be reduced; consider reduced dosage. (See Geriatric Patients under Dosage and Administration and see Special Populations under Pharmacokinetics.)
Hepatic Impairment
Reduce dosage in patients with severe hepatic impairment. (See Hepatic Impairment under Dosage and Administration and see Special Populations under Pharmacokinetics.)
Renal Impairment
Use with caution in patients with severe renal impairment. (See Renal Impairment under Dosageand Administration and see Special Populations under Pharmacokinetics.)
Common Adverse Effects
Headache, nausea, nervousness, rhinitis, diarrhea, back pain, anxiety, insomnia, dizziness, dyspepsia.
Drug Interactions
Partially metabolized by CYP3A4 enzymes. Modafinil and modafinil sulfone metabolite reversibly inhibit CYP2C19. Slightly induces CYP1A2, CYP2B6, and CYP3A4 and produces suppression of CYP2C9 activity in a concentration-dependent manner in vitro.
Possible auto-induction of modafinil metabolism after multiple weeks of dosing; magnitude of decreases in modafinil trough concentrations and inconsistency of occurrence suggest clinical importance is minimal.
Drugs Affecting Hepatic Microsomal Enzymes
Potent inducers or inhibitors of CYP3A4: Potential pharmacokinetic interaction (altered elimination of modafinil).
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP1A2, CYP2B6, and CYP3A4: Potential pharmacokinetic interaction (decreased plasma substrate concentrations). Caution if used concomitantly.
Substrates of CYP2C19: Potential pharmacokinetic interaction (possible prolonged elimination of substrate).
Substrates of CYP2C9: Potential metabolic interaction.
Protein-bound Drugs
Potential for interactions with highly protein-bound drugs considered unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Concomitant use not evaluated |
Avoid alcohol during therapy |
|
Antidepressants, SSRIs |
Possible increased SSRI concentration in patients who are CYP2D6 deficient |
Dosage adjustment of SSRI may be necessary |
|
Antidepressants, tricyclics |
Possible increased concentration of certain tricyclic antidepressants (e.g., clomipramine, desipramine) in patients who are CYP2D6 deficient |
Dosage reduction of tricyclic antidepressant may be necessary |
|
Antifungals, azoles (itraconazole, ketoconazole) |
Possible increased plasma modafinil concentrations |
|
|
Carbamazepine |
Possible decreased modafinil plasma concentrations |
|
|
Clomipramine |
Pharmacokinetic interaction unlikely; however, increased concentrations of clomipramine and its active desmethyl metabolite reported in a patient who was a poor CYP2D6 metabolizer |
Dosage reduction of clomipramine may be necessary |
|
Clozapine |
Possible elevation in serum clozapine concentrations and resulting clozapine toxicity |
Use concomitantly with caution; closely monitor serum clozapine concentrations |
|
Cyclosporine |
Possible decreased blood concentrations and effectiveness of cyclosporine |
Consider monitoring cyclosporine concentrations; adjust cyclosporine dosage if necessary |
|
Dextroamphetamine |
Clinically important pharmacokinetic interaction unlikely, although modafinil absorption may be delayed by approximately 1 hour |
|
|
Diazepam |
Possible increased plasma diazepam concentrations |
May need to reduce diazepam dosage and monitor for toxicity |
|
Hormonal contraceptives |
Potential for decreased plasma concentrations of ethinyl estradiol; possible hormonal contraceptive failure |
Alternative or concomitant nonhormonal methods of contraception recommended during and for 1 month after discontinuance of modafinil therapy |
|
MAO inhibitors |
Interaction studies not performed to date Acute chorea, confusion, and hyperthermia (possibly related to serotonin syndrome) reported with concurrent modafinil and tranylcypromine |
Use concomitantly with caution |
|
Methylphenidate |
Clinically important pharmacokinetic interaction unlikely, although modafinil absorption may be delayed by approximately 1 hour |
|
|
Phenobarbital |
Possible decreased plasma modafinil concentrations |
|
|
Phenytoin |
Possible increased plasma phenytoin concentrations |
May need to reduce phenytoin dosage and monitor for toxicity |
|
Propranolol |
Possible increased plasma propranolol concentrations |
May need to reduce propranolol dosage and monitor for toxicity |
|
Rifampin |
Possible decreased plasma modafinil concentrations |
|
|
Triazolam |
Potential for reduced plasma concentrations and effectiveness of triazolam |
Dosage adjustment of triazolam may be necessary |
|
Warfarin |
Single-dose pharmacokinetics of warfarin not substantially affected by chronic administration of modafinil |
Monitor PT and/or INR more frequently |
Modafinil Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract after oral administration, with peak plasma concentrations attained within 2–4 hours. Absolute oral bioavailability not determined due to low aqueous solubility.
Food
Food may delay GI absorption by approximately 1 hour, but does not affect extent of absorption.
Distribution
Extent
Well distributed into body tissues.
Not known whether modafinil or its metabolites are distributed into milk.
Plasma Protein Binding
Approximately 60% (mainly albumin).
Elimination
Metabolism
Metabolized to inactive metabolites via hydrolytic deamidation, S-oxidation, aromatic ring hydroxylation, and glucuronide conjugation.
Elimination Route
Excreted in urine (80%) and in feces (1%), mainly as metabolites.
Half-life
Approximately 10–15 hours after multiple dosing.
Special Populations
In patients with severe hepatic impairment and cirrhosis (Child-Pugh class B, B+, C, or C+), clearance of modafinil is decreased by about 60% and steady-state concentrations are doubled compared with healthy individuals.
In patients with severe chronic renal impairment (Clcr ≤20 mL/minute), pharmacokinetics of modafinil are not substantially altered, but exposure to modafinil acid (an inactive metabolite) is increased ninefold compared with healthy individuals.
In geriatric patients, clearance of modafinil and metabolites may be reduced.
Stability
Storage
Oral
Tablets
20–25°C.
Actions
-
Modafinil, a nonamphetamine wakefulness-promoting agent, is a 50:50 racemic mixture of the R- and S-enantiomers; exhibits pharmacologic properties similar to those of armodafinil.
-
Promotes vigilance and wakefulness. Exact mechanism of action unknown, but may alter metabolic activity and increase neuronal activity in areas of the brain that control sleep/wakefulness and the biologic clock.
-
Inhibits release of GABA and increases release of glutamate from the cerebral cortex, hippocampus, nucleus accumbens, medial preoptic area, and posterior hypothalamus in animals.
-
Does not appear to act as a direct- or indirect-acting dopamine-receptor or α1-adrenergic agonist or as a sympathomimetic agent; may stimulate central α1-adrenergic activity but has no important peripheral adrenergic activity. Blocked dopamine transporters and increased dopamine concentrations in the human brain (including the nucleus accumbens); drugs with such activity generally have abuse potential.
-
At usual pharmacologic concentrations, does not bind to certain receptors that regulate sleep and wakefulness (e.g., norepinephrine, serotonin, dopamine, GABA, adenosine, histamine H3, melatonin, benzodiazepine).
-
Does not inhibit MAO-B or phosphodiesterases 2-5; does not alter plasma melatonin or cortisol hormone profiles.
-
Reinforcing properties in animals; produces psychoactive, euphoric, and subjective effects typical of classic CNS stimulants (e.g., amphetamines, methylphenidate) in humans.
Advice to Patients
-
Importance of providing copy of written patient information (medication guide) each time modafinil is dispensed; importance of reading this information prior to taking modafinil.
-
Importance of advising clinician of existing or contemplated therapy, including prescription and OTC drugs and/or herbal supplements, as well as any concomitant illnesses. Advise patient that it is prudent to avoid alcohol since combined use has not been studied.
-
Potential increased risk of pregnancy in women taking hormonal contraceptives (e.g., oral contraceptives, injectable or implantable contraceptives, transdermal systems, vaginal rings, intrauterine devices) during and for 1 month after discontinuing modafinil therapy; discuss use of alternative or concomitant methods of contraception during these periods. (See Contraceptive Precautions under Cautions.) Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of clinicians informing women about the existence of and encouraging enrollment in the Provigil pregnancy registry (see Pregnancy under Cautions).
-
Risk of serious rash or serious allergic reaction. Advise patient to immediately discontinue modafinil and notify their clinician if they develop a rash or other manifestations of an allergic reaction (e.g., hives; mouth sores; blisters; peeling skin; swelling of face, eyes, lips, tongue, or larynx; difficulty swallowing or breathing; hoarseness; a related allergic phenomenon).
-
Risk of mental (psychiatric) symptoms. Importance of discontinuing modafinil and informing clinician if depression, anxiety, hallucinations, mania, suicidal thoughts, aggression, or other psychiatric symptoms occur.
-
Risk of heart problems. Importance of discontinuing modafinil and informing clinician if symptoms of a heart problem, including chest pain, abnormal heart beats, and trouble breathing, occur.
-
Advise that modafinil may affect judgment, thinking, or motor skills. Use caution when operating machinery or driving a motor vehicle until effects of the drug are known.
-
Advise patient that modafinil may improve, but not eliminate, the abnormal tendency to fall asleep. Therefore, stress importance of not altering previous behavior with regard to activities that require appropriate levels of wakefulness (e.g., driving, operating machinery) until and unless modafinil produces sufficient wakefulness to permit such activities. Advise that modafinil is not a replacement for sleep.
-
Importance of continuing previously prescribed therapy (e.g., patients with OSAHS should continue using their CPAP machine while sleeping).
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule IV (C-IV) drug.
|
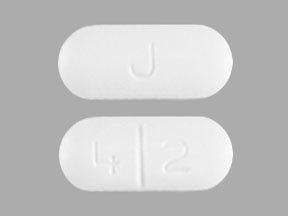
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
100 mg |
Provigil (C-IV) |
Cephalon |
|
200 mg |
Provigil (C-IV; scored) |
Cephalon |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 3, 2014. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Adderall
Adderall (amphetamine and dextroamphetamine) is used to treat narcolepsy and ADHD. Includes side ...
Concerta
Concerta is used to treat attention deficit disorder (ADD) and attention deficit hyperactivity ...
Xywav
Xywav is used for the treatment of cataplexy and excessive daytime sleepiness (EDS) in patients ...
Ritalin
Ritalin (methylphenidate) is used to treat attention deficit disorder (ADD) and narcolepsy ...
Provigil
Provigil promotes wakefulness and is used to treat excessive daytime sleepiness caused by ...
Armodafinil
Armodafinil may be used to improve wakefulness in adults who are very sleepy due to narcolepsy ...
Amphetamine
Amphetamine is a stimulant and is used to trat narcolepsy and attention deficit disorder. Includes ...
Amphetamine/dextroamphetamine
Amphetamine/dextroamphetamine is used for ADHD, fatigue, narcolepsy
Frequently asked questions
- Modafinil (Provigil) vs Adderall: What's the difference?
- How do I know if I have sleep apnea? The warning signs
- Modafinil: Smart Drug For Decision Fatigue Or Workaholic Crutch?
- How long does it take for Provigil (modafinil) to work?
- Is Provigil (modafinil) a controlled substance?
- Is sleep apnea the hidden cause of your high blood pressure?
- Can sleep apnea kill you? Understanding the real risks?
- Does Provigil (modafinil) cause weight loss?
More about modafinil
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (536)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: CNS stimulants
- Breastfeeding
- En español