Ephedrine (Monograph)
Brand name: Akovaz
Drug class: alpha- and beta-Adrenergic Agonists
VA class: AU100
Chemical name: [R-(R*, S*)]-α-[1-(Methylamino)ethyl]-benzenemethanol hydrochloride
Molecular formula: C10H15NO • HCl(C10H15NO)2 • H2SO4
CAS number: 299-42-3
Introduction
Sympathomimetic agent.
Uses for Ephedrine
Hypotension During Anesthesia
Used parenterally for treatment of clinically important hypotension in the setting of anesthesia.
Increases systolic and mean arterial BP when administered as a direct IV (“bolus”) injection following development of hypotension in patients receiving neuraxial and/or general anesthesia. Such effects observed across a variety of surgical settings, including obstetric surgery in pregnant women undergoing cesarean delivery with neuraxial anesthesia.
Although ephedrine historically considered the vasopressor of choice in obstetric anesthesia, some evidence suggests that phenylephrine may provide more favorable fetal acid-base balance. Experts currently recommend either IV ephedrine or phenylephrine for treatment of hypotension during neuraxial anesthesia; however, consideration should be given to selection of phenylephrine in the absence of maternal bradycardia because of improved fetal acid-base status in uncomplicated pregnancies.
IM use of ephedrine also evaluated in this setting; however, results have been equivocal.
Bronchospasm
Used orally as a bronchodilator for symptomatic treatment of asthma.
Used in fixed-combination with guaifenesin as self-medication for the temporary relief of mild symptoms of intermittent asthma (e.g., wheezing, chest tightness, shortness of breath).
Use of an OTC bronchodilator may be appropriate in patients with mild symptoms of intermittent asthma; however, those with more severe asthma (i.e., persistent asthma) or worsening asthma (symptoms not relieved within 60 minutes or with maximum recommended dosages, increasing frequency of asthma attacks) should consult a clinician for other treatment options.
While oral ephedrine was once widely used in the treatment of asthma, the drug generally has been replaced by more selective and rapid-acting agents (e.g., inhaled β2-adrenergic agonists).
CNS Conditions
Has been used in the treatment of narcolepsy† [off-label] or depressive states† [off-label]; however, cardiovascular effects of the drug limit usefulness in these conditions.
Obesity
Previously used for self-medication in the management of obesity† [off-label].
Dietary supplements containing ephedrine alkaloids are no longer commercially available in the US. (See Risks Associated with Dietary Supplements under Cautions.)
Nasal Congestion
Has been used as a nasal decongestant, but of doubtful value when used for this condition.
Myasthenia Gravis
Has been used in patients with myasthenia gravis† [off-label]; however, randomized controlled studies are needed to evaluate potential benefit.
Misuse and Abuse
Has been misused and abused by athletes, bodybuilders, weight lifters, and others, including high school- and college-aged individuals engaged in sports† [off-label].
Dietary supplements containing ephedrine alkaloids are no longer commercially available in the US. (See Risks Associated with Dietary Supplements under Cautions.)
Ephedrine has been used in clandestine synthesis of methamphetamine and methcathinone. Federal restrictions to reduce the potential for misuse (diversion) and abuse of ephedrine include limiting the amount that can be purchased to 3.6 g per day or 9 g per month, requiring storage behind the counter or in a locked cabinet, requiring purchasers to provide approved photographic identification, and requiring retail distributors to maintain a written or electronic logbook of purchases for at least 2 years. (For additional information on these and other federal restrictions, visit [[Web]]). Additional requirements have been enacted in some states; follow state requirements if such requirements are more stringent than federal restrictions.
Ephedrine Dosage and Administration
Administration
Oral Administration
Administer orally as a fixed-combination preparation.
Parenteral Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by IV injection. Also has been administered by sub-Q† or IM† injection.
Administer ephedrine sulfate (Akovaz) by direct IV (“bolus”) injection. Must dilute commercially available injection prior to IV administration. May prepare a 5-mg/mL solution by diluting 1 mL of the 50-mg/mL injection concentrate with 9 mL of 0.9% sodium chloride injection or 5% dextrose injection.
Vials are for single-use only; discard unused portions.
Dosage
Available as ephedrine hydrochloride or ephedrine sulfate; dosage expressed in terms of the salt.
Pediatric Patients
Hypotension During Anesthesia
IM† or Sub-Q†
Ephedrine sulfate: Usual dose of 0.5 mg/kg or 16.7 mg/m2 every 4–6 hours has been administered. However, ephedrine sulfate injection not FDA-labeled for use in pediatric patients.
Bronchospasm
Oral
Ephedrine hydrochloride or sulfate self-medication in children ≥12 years of age: 12.5–25 mg every 4 hours as needed for treatment of mild symptoms of intermittent asthma; administer in fixed combination with guaifenesin.
IM† or Sub-Q†
Ephedrine sulfate: Usual dose of 0.5 mg/kg or 16.7 mg/m2 every 4–6 hours has been administered. However, ephedrine sulfate injection not FDA-labeled for use in pediatric patients.
Adults
Hypotension During Anesthesia
IV
Ephedrine sulfate: Initially, 5–10 mg by IV bolus injection; administer additional bolus doses as needed (up to a total dose of 50 mg) to achieve desired BP response.
Other IV dosage regimens have been recommended.
IM † or Sub-Q†
Ephedrine sulfate: Usual dose of 25–50 mg has been administered.
Bronchospasm
Oral
Ephedrine hydrochloride or sulfate self-medication: 12.5–25 mg every 4 hours as needed for treatment of mild symptoms of intermittent asthma; administer in fixed combination with guaifenesin.
Parenteral
Ephedrine sulfate: Parenteral doses of 12.5–25 mg have been given.
Prescribing Limits
Pediatric Patients
Bronchospasm
Oral
Ephedrine hydrochloride or sulfate self-medication in children ≥12 years of age: Maximum 150 mg in any 24-hour period.
Adults
Bronchospasm
Oral
Ephedrine hydrochloride or sulfate self-medication: Maximum 150 mg in any 24-hour period.
Cautions for Ephedrine
Contraindications
-
For self-medication in asthma: Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor, pediatric patients <12 years of age, known hypersensitivity to the specific product or any of its ingredients.
-
Known hypersensitivity to ephedrine or sympathomimetic drugs.
Warnings/Precautions
Warnings
Cardiovascular Effects
May cause hypertension and tachycardia; risk of serious adverse effects (e.g., MI, stroke, intracranial hemorrhage, exacerbation of CHF, death). (See Risks Associated with Dietary Supplements under Cautions.)
Serious postpartum hypertension, in some cases resulting in stroke, reported in patients receiving a vasopressor (e.g., ephedrine) and an oxytocic agent (e.g., ergonovine, methylergonovine) concomitantly. (See Specific Drugs under Interactions.)
Increased risk of hypertension in patients receiving ephedrine sulfate injection for prevention of hypotension.
Risk of anginal pain in patients with coronary insufficiency or ischemic heart disease. Risk of potentially fatal arrhythmias in patients with organic heart disease or in those receiving drugs that sensitize the myocardium (e.g., cyclopropane, halothane).
Caution in patients with cardiovascular disease (e.g., angina) and in those receiving digoxin.
Tolerance and Tachyphylaxis
Tolerance and tachyphylaxis may develop with repeated parenteral administration; in some cases; effectiveness may return after the drug is withheld temporarily.
If used for treatment of hypotension during anesthesia, consider possibility of tachyphylaxis and be prepared to use an alternative vasopressor.
Concomitant Diseases
Use with caution in patients with cardiovascular disease, hypertension, angina, hyperthyroidism, diabetes mellitus, or prostatic hyperplasia. Patients with cardiovascular disease, hypertension, diabetes mellitus, thyroid disease, seizures, angle-closure (narrow-angle) glaucoma, psychiatric or emotional conditions should consult a clinician before initiating self-medication with ephedrine.
Use for self-medication for bronchospasm only if previously diagnosed with asthma; do not use if previously hospitalized for asthma unless directed by a clinician.
Risks Associated with Dietary Supplements
Dietary supplements containing ephedrine alkaloids have been associated with serious adverse cardiac effects (e.g., hypertension, possibly resulting in MI, stroke, or death), CNS effects, and death.
In February 2004, FDA declared dietary supplements containing ephedrine alkaloids adulterated by virtue of their unreasonable health risks to consumers. Manufacturing, sale, and distribution of all dietary supplements containing ephedrine alkaloids (e.g., Ephedra spp. [“ma huang”], Sida cordifolia, Pinellia spp.) were prohibited after April 12, 2004. This regulation does not apply to traditional Chinese herbal remedies or products regulated as conventional foods (e.g., herbal teas). Ephedra is not generally recognized as safe for foods and not approved for use as a food additive. After litigation, FDA’s rule was upheld, and FDA reiterated its position that no dosage of dietary supplements containing ephedrine alkaloids is safe, and the sale of these products in the US is illegal and subject to FDA enforcement action.
General Precautions
When used in fixed combination with guaifenesin, observe the usual cautions, precautions, and contraindications associated with guaifenesin.
Duration of Therapy
Self-medication in asthma: Consult a clinician if symptoms are not improved within 1 hour or worsen, more than the recommended dosage of ephedrine is required, or asthma attacks become more frequent (i.e., >2 asthma attacks in a week).
Misuse and Abuse
Potential for misuse and abuse.
Specific Populations
Pregnancy
Animal reproduction studies not performed to date; not known whether the drug can cause fetal harm or miscarriage when administered during pregnancy.
Has been used in pregnant women for treatment of hypotension during spinal anesthesia; available data support efficacy and safety of ephedrine sulfate injection for such use.
Some evidence indicates that fetal acidosis is more likely to occur with ephedrine than phenylephrine. Low umbilical artery pH (≤7.2) reported at the time of delivery in neonates whose mothers were exposed to ephedrine. Assess acid-base status in newborn infants and monitor for signs and symptoms of metabolic acidosis.
Lactation
Distributed into milk; however, no information regarding effects on breast-fed infant or milk production. Consider known benefits of breast-feeding along with mother's clinical need for ephedrine and any potential adverse effects of the drug or underlying maternal condition on the infant.
Pediatric Use
Ephedrine sulfate injection is not FDA-labeled for use in pediatric patients. Although the drug has been used in children, safety and efficacy not established in this patient population.
Should not be used for self-medication in children <12 years of age unless otherwise directed by a clinician.
Risk of overdosage and toxicity (including death) in children <2 years of age receiving OTC preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection. Limited evidence of efficacy for these preparations in this age group; appropriate dosages not established. Therefore, FDA recommends not to use such preparations in children <2 years of age; safety and efficacy in older children under evaluation. Because children 2–3 years of age also are at increased risk of overdosage and toxicity, some manufacturers of oral nonprescription cough and cold preparations agreed to voluntarily revise the product labeling to state that such preparations should not be used in children <4 years of age. FDA recommends that parents and caregivers adhere to dosage instructions and warnings on the product labeling that accompanies the preparation and consult a clinician about any concerns. Clinicians should ask caregivers about use of OTC cough/cold preparations to avoid overdosage.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults. Other clinical experience has not identified differences in responses between geriatric and younger patients. Select dosage with caution, usually starting at low end of dosage range.
Because geriatric patients may have decreased renal function, risk of adverse effects may be increased; consider monitoring renal function.
Renal Impairment
Substantially excreted by kidneys; risk of ephedrine-induced adverse effects may be increased in patients with impaired renal function.
Carefully monitor patients with renal impairment after administration of initial IV dose.
Common Adverse Effects
Parenteral ephedrine: Nervousness, insomnia, vertigo, headache, tachycardia, palpitation, sweating, nausea, vomiting, anorexia, vesical sphincter spasm (resulting in difficult and painful urination), urinary retention (particularly in males with prostatism).
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comment |
|---|---|---|
|
α-Adrenergic blocking agents |
Vasopressor response to ephedrine decreased |
Carefully monitor BP |
|
β-Adrenergic blocking agents |
Antagonism of cardiac and bronchodilating effects of ephedrine |
Carefully monitor BP |
|
Anesthetics, epidural |
May decrease efficacy of epidural blockade by facilitating regression of sensory analgesia |
Monitor patients for this effect and treat accordingly |
|
Anesthetics, general (e.g., halogenated hydrocarbons [e.g., halothane], cyclopropane) |
Increased cardiosensitivity to ephedrine and possible increased risk of arrhythmias |
|
|
Atropine |
May increase pressor effect |
Carefully monitor BP |
|
Cardiac glycosides |
Increased cardiosensitivity to ephedrine and possible increased risk of arrhythmias |
Carefully monitor patients |
|
Clonidine |
May increase pressor effect |
Carefully monitor BP |
|
Diuretics |
Decreased arterial responsiveness to pressor drugs |
|
|
MAO inhibitors |
Pressor effects of ephedrine increased; may result in hypertensive crisis or subarachnoid hemorrhage rarely |
Carefully monitor BP Some manufacturers recommend avoidance with or for 2 weeks after discontinuance of MAO inhibitors |
|
Oxytocics (e.g., ergonovine, methylergonovine) |
May increase pressor effect and cause severe postpartum hypertension and possible stroke |
Carefully monitor BP |
|
Propofol |
May increase pressor effect |
Carefully monitor BP |
|
Quinidine |
May antagonize pressor effect |
Carefully monitor BP |
|
Reserpine |
May antagonize pressor effect |
Carefully monitor BP |
|
Rocuronium |
Ephedrine may reduce onset time of rocuronium-induced neuromuscular blockade for intubation when administered simultaneously with anesthetic induction |
|
|
Theophylline |
May increase incidence of nausea, nervousness, and insomnia |
Monitor patients for these symptoms and treat accordingly |
Ephedrine Pharmacokinetics
Absorption
Bioavailability
Peak serum concentrations attained within 2.6–3 hours following oral administration.
Onset
Oral administration: Bronchodilation occurs within 15–60 minutes.
Duration
Oral administration: Bronchodilation persists for 2–4 hours; pressor and cardiac responses persist for up to 4 hours following oral administration of 15–50 mg.
Parenteral administration: Pressor and cardiac responses persist for 1 hour after IV administration of 10–25 mg or IM or sub-Q administration of 25–50 mg.
Distribution
Extent
Distributed into milk.
Elimination
Metabolism
Metabolic pathway not completely elucidated. Some data suggest drug is slowly metabolized in the liver.
Elimination Route
Ephedrine and its metabolites are excreted in urine; most of the drug is excreted as unchanged ephedrine. The rate of urinary excretion of ephedrine and its metabolites is dependent upon urinary pH.
Half-life
About 3 hours when the urine is acidified to pH 5; about 6 hours when urinary pH is about 6.3.
Stability
Storage
Oral
Fixed-dose Combination with Guaifenesin
Primatene tablets: 20–25°C.
Bronkaid caplets: Room temperature; avoid exposure to >40°C.
Parenteral
Injection
20–25°C. Store in carton until time of use. Protect from light.
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|---|
|
Dextrose–Ringer’s injection combinations |
|
Dextrose–Ringer’s injection, lactated, combinations |
|
Dextrose–saline combinations |
|
Dextrose 2½, 5, or 10% in water |
|
Ionosol products |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.45 or 0.9% |
|
Sodium lactate (1/6) M |
Drug Compatibility
|
Compatible |
|---|
|
Chloramphenicol sodium succinate |
|
Lidocaine HCl |
|
Nafcillin sodium |
|
Penicillin G potassium |
|
Incompatible |
|
Pentobarbital sodium |
|
Phenobarbital sodium |
|
Compatible |
|---|
|
Bivalirudin |
|
Dexmedetomidine HCl |
|
Etomidate |
|
Fenoldopam mesylate |
|
Hetastarch in lactated electrolyte injection (Hextend) |
|
Propofol |
Actions
-
Sympathomimetic agent; occurs naturally in plants of the genus Ephedra.
-
Stimulates both α- and β-adrenergic receptors.
-
Relaxes bronchial smooth muscle, stimulates cardiac muscle (producing positive inotropic effects), constricts arterioles, increases BP, and stimulates the cerebral cortex and subcortical centers.
-
Relaxes GI smooth muscle. Contracts urinary bladder trigone and sphincter and relaxes the detrusor muscle.
Advice to Patients
-
For self-medication in asthma, importance of not exceeding recommended dosages or frequency of administration unless otherwise instructed by a clinician.
-
For self-medication in asthma, importance of discontinuing therapy and contacting a clinician if symptoms are not improved within 1 hour or they become worse.
-
For asthma, advise that ephedrine should be used for self-medication only if asthma was previously diagnosed by a clinician. Before considering self-medication, inform clinician of any history of hospitalization for asthma.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses (e.g., cardiovascular disease). Importance of avoiding MAO inhibitors and allowing 2 weeks to elapse after discontinuing these antidepressants.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder* |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
50 mg/mL* |
Akovaz |
Eclat |
|
ePHEDrine Sulfate Injection |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
12.5 mg with Guaifenesin 200 mg |
Ephed Plus |
DMD |
|
Primatene |
Pfizer |
|||
|
25 mg with Guaifenesin 200 mg |
Ephed Plus |
DMD |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg with Guaifenesin 400 mg |
Bronkaid Caplets |
Bayer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 15, 2017. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about ephedrine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (9)
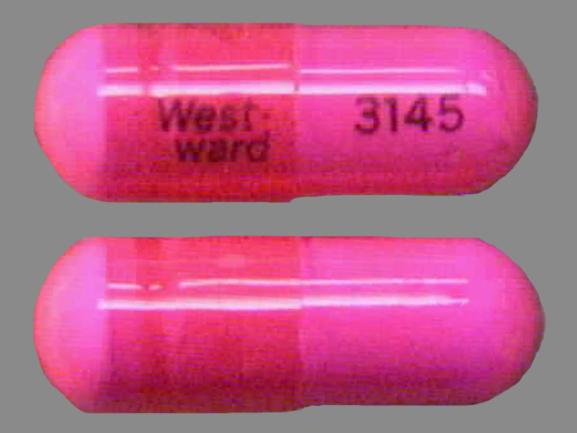
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: decongestants
Patient resources
Professional resources
Other brands
Akovaz, Corphedra, Emerphed, Rezipres