Captopril, Captopril and Hydrochlorothiazide (Monograph)
Drug class: Angiotensin-Converting Enzyme Inhibitors
Captopril, Captopril and Hydrochlorothiazide (Systemic) is also contained as an ingredient in the following combinations:
Captopril and Hydrochlorothiazide
Warning
-
May cause fetal and neonatal morbidity and mortality if used during pregnancy. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
If pregnancy is detected, discontinue captopril as soon as possible.
Introduction
Sulfhydryl ACE inhibitor.
Uses for Captopril, Captopril and Hydrochlorothiazide
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents).
ACE inhibitors are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include angiotensin II receptor antagonists, calcium-channel blockers, and thiazide diuretics. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Other hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the current ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient’s BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the current ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to ACE inhibitors. However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
ACE inhibitors may be preferred in hypertensive patients with heart failure, ischemic heart disease, diabetes mellitus, CKD, or cerebrovascular disease or post-MI.
Has been used in the management of hypertensive urgencies† [off-label].
Diabetic Nephropathy
Management of diabetic nephropathy manifested by proteinuria (urinary protein excretion >500 mg/24 hours) in patients with type 1 diabetes mellitus and diabetic retinopathy.
A recommended agent in the management of patients with diabetes mellitus and persistent albuminuria who have modestly elevated (30–300 mg/24 hours) or higher (>300 mg/24 hours) levels of urinary albumin excretion; slows rate of progression of renal disease in such patients.
Heart Failure
Management of heart failure, usually in conjunction with other agents such as cardiac glycosides, diuretics, and β-adrenergic blocking agents (β-blockers).
Some evidence indicates that therapy with an ACE inhibitor may be less effective than angiotensin receptor-neprilysin inhibitor (ARNI) therapy (e.g., sacubitril/valsartan) in reducing cardiovascular death and heart failure-related hospitalization.
ACCF, AHA, and the Heart Failure Society of America (HFSA) recommend that patients with chronic symptomatic heart failure and reduced left ventricular ejection fraction (LVEF) (NYHA class II or III) who are able to tolerate an ACE inhibitor or angiotensin II receptor antagonist be switched to therapy containing an ARNI to further reduce morbidity and mortality.
Left Ventricular Dysfunction After Acute MI
Treatment of clinically stable patients with left ventricular dysfunction (ejection fraction ≤40%) to improve survival following MI and to reduce the incidence of overt heart failure and subsequent hospitalizations for heart failure.
Expert guidelines recommend initiation of an oral ACE inhibitor within the first 24 hours of acute MI in patients with an anterior infarct, heart failure, or ejection fraction ≤40% who do not have any contraindications (e.g., hypotension, shock, renal dysfunction). Use with caution (and with gradual upward titration) during initial postinfarction period because of the possibility of hypotension or renal dysfunction.
Continue therapy indefinitely in patients with left ventricular dysfunction or other compelling indications (e.g., hypertension, diabetes mellitus, CKD).
Captopril, Captopril and Hydrochlorothiazide Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., calcium-channel blocker, thiazide diuretic). Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Oral Administration
Administer orally 1 hour before meals to maximize absorption.
Extemporaneously Compounded Oral Liquid
An extemporaneously compounded oral liquid formulation of captopril has been prepared.
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral liquid formulation of captopril have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web] .
|
Concentration Standards |
|---|
|
1 mg/mL |
Dosage
Pediatric Patients
Hypertension
Oral
Dosage has been reduced in proportion to body weight; titrate carefully. Initiate drug at the low end of the dosage range per some experts; may increase dosage every 2–4 weeks until BP controlled, maximum dosage (6 mg/kg per day) reached, or adverse effects occur.
Infants: Some experts recommend initial dosage of 0.05 mg/kg 1–4 times daily.
Children: Some experts recommend initial dosage of 0.5 mg/kg 3 times daily.
Adults
Hypertension
Captopril Therapy
OralManufacturer recommends initial dosage of 25 mg 2 or 3 times daily; if response is inadequate after 1–2 weeks, dosage may be increased to 50 mg 2 or 3 times daily.
Lower initial dosages (e.g., 6.25 mg twice daily to 12.5 mg 3 times daily) may be effective in some patients, particularly those already receiving a diuretic. (See Hypotension under Cautions.)
Usual maintenance dosage: Manufacturers recommend 25–150 mg 2 or 3 times daily (usually not necessary to exceed 150 mg daily).
Captopril/Hydrochlorothiazide Fixed-combination Therapy
OralIf combination therapy is initiated with captopril/hydrochlorothiazide fixed-combination preparation, initial dosage of captopril 25 mg and hydrochlorothiazide 15 mg once daily; adjust dosage (generally at 6-week intervals) by administering each drug separately or by advancing the fixed-combination preparation.
Hypertensive Crises
OralSevere (e.g., accelerated, malignant) hypertension: 25 mg 2 or 3 times daily, initiated promptly under close supervision with frequent monitoring of BP. May continue previous diuretic therapy, but discontinue other hypotensive agents. May increase dosage at intervals of ≤24 hours under continuous supervision until optimum BP response is attained or 450 mg daily is given. Adjunctive therapy with other hypotensive agents may be necessary.
Hypertensive urgency† [off-label]: Acute therapy (e.g., 12.5–25 mg, repeated once or twice if necessary at intervals of 30–60 minutes or longer) has been used.
Diabetic Nephropathy
Oral
25 mg 3 times daily.
Heart Failure
Oral
Manufacturers recommend initial dosage of 25 mg 3 times daily; in patients with normal or low BP who may be volume- and/or salt-depleted, initial dosage of 6.25 or 12.5 mg 3 times daily. Increase dosage gradually to 50 mg 3 times daily; delay further dosage increases for ≥2 weeks to assess response.
ACCF and AHA recommend initial dosage of 6.25 mg 3 times daily, with gradual titration to 50 mg 3 times daily. Generally titrate dosage to prespecified target (i.e., ≥150 mg daily) or highest tolerated dosage rather than according to response.
Left Ventricular Dysfunction After Acute MI
Oral
Manufacturers recommend initiation of therapy ≥3 days post-MI with single dose of 6.25 mg, followed by 12.5 mg 3 times daily. Increase dosage over next several days to 25 mg 3 times daily and then over next several weeks (as tolerated) to 50 mg 3 times daily.
Some clinicians recommend initiation of therapy within the first 24 hours following MI.
Recommended maintenance dosage: 50 mg 3 times daily.
Prescribing Limits
Pediatric Patients
Hypertension
Oral
Maximum 6 mg/kg daily.
Adults
Hypertension
Oral
Maximum 450 mg daily.
Dosage of captopril/hydrochlorothiazide fixed-combination generally should not exceed captopril 150 mg and hydrochlorothiazide 50 mg daily.
Heart Failure
Oral
Maximum dosage recommended by manufacturer is 450 mg daily. Experts suggest maximum dosage of 50 mg 3 times daily.
Special Populations
Renal Impairment
Manufacturers recommend initial dosage of <75 mg daily; increase dosage in small increments at 1- to 2-week intervals. After desired therapeutic effect has been attained, slowly reduce dosage to minimum effective level.
Patients with Clcr 10–50 mL/minute: 75% of usual captopril dosage or administration of usual dose every 12–18 hours suggested by some clinicians.
Clcr <10 mL/minute: 50% of usual dosage or administration of usual dose every 24 hours suggested by some clinicians.
Patients undergoing hemodialysis may require supplemental dose after dialysis.
Fixed-combination captopril/hydrochlorothiazide tablets usually are not recommended for patients with severe renal impairment.
Geriatric Patients
Hypertension
Usual adult dosages generally have been used; dosages of 6.25–12.5 mg 1–4 times daily used occasionally.
Volume-and/or Salt-Depleted Patients
Correct volume and/or salt depletion prior to initiation of therapy or initiate therapy under close medical supervision using lower initial dosage. (See Dosage: Heart Failure, under Dosage and Administration.)
Cautions for Captopril, Captopril and Hydrochlorothiazide
Contraindications
-
Known hypersensitivity (e.g. history of angioedema) to captopril or another ACE inhibitor.
Warnings/Precautions
Warnings
Hematologic Effects
Possible neutropenia or agranulocytosis; risk of neutropenia appears to depend principally on degree of renal impairment and presence of collagen vascular disease (e.g., systemic lupus erythematosus, scleroderma).
Use with caution and only after careful risk/benefit assessment in patients with collagen vascular disease or those taking drugs known to affect leukocytes or immune response.
If used in patients with renal impairment, determine complete and differential leukocyte counts prior to initiation of therapy, at about 2-week intervals for the first 3 months of therapy, and periodically thereafter. Discontinue therapy if confirmed neutrophil count is <1000/mm3.
Proteinuria
Proteinuria possible, particularly in patients with prior renal disease and/or those receiving relatively high dosages (>150 mg daily). Usually occurs by the 8th month of treatment and subsides or clears within 6 months whether or not therapy is continued; however, may persist in some patients.
Hypotension
Possible excessive hypotension, particularly in volume- and/or salt-depleted patients (e.g., those treated with diuretics or undergoing dialysis, patients with severe heart failure).
Hypotension may occur in patients undergoing surgery or during anesthesia with agents that produce hypotension; recommended treatment is fluid volume expansion.
Transient hypotension is not a contraindication to additional doses; may reinstate therapy cautiously after BP is stabilized (e.g., with volume expansion).
To minimize potential for hypotension, consider recent antihypertensive therapy, extent of BP elevation, sodium intake, fluid status, and other clinical conditions. (See Special Populations under Dosage and Administration.) Discontinue other antihypertensive therapy, if possible, 1 week before initiating captopril, except in patients with severe hypertension. Withholding diuretic therapy and/or increasing sodium intake approximately 3–7 days prior to initiation of captopril may minimize potential for severe hypotension.
Initiate therapy in patients with heart failure under close medical supervision; monitor closely for first 2 weeks following initiation of captopril or any increase in captopril or diuretic dosage.
Fetal/Neonatal Morbidity and Mortality
Possible fetal and neonatal morbidity and mortality when used during pregnancy. (See Boxed Warning.) Such potential risks occur throughout pregnancy, especially during the second and third trimesters.
Also may increase the risk of major congenital malformations when administered during the first trimester of pregnancy.
Discontinue as soon as possible when pregnancy is detected, unless continued use is considered lifesaving. Nearly all women can be transferred successfully to alternative therapy for the remainder of their pregnancy.
Hepatic Effects
Clinical syndrome that usually is manifested initially by cholestatic jaundice and may progress to fulminant hepatic necrosis (occasionally fatal) reported rarely with ACE inhibitors.
If jaundice or marked elevation of liver enzymes occurs, discontinue drug and monitor patient.
Sensitivity Reactions
Anaphylactoid reactions and/or angioedema possible; if associated with laryngeal edema, may be fatal. Immediate medical intervention (e.g., epinephrine) for involvement of tongue, glottis, or larynx. Intestinal angioedema possible; consider in differential diagnosis of patients who develop abdominal pain.
Anaphylactoid reactions reported in patients receiving ACE inhibitors while undergoing LDL apheresis with dextran sulfate absorption or following initiation of hemodialysis that utilized high-flux membrane.
Life-threatening anaphylactoid reactions reported in at least 2 patients receiving ACE inhibitors while undergoing desensitization treatment with hymenoptera venom.
Not recommended in patients with a history of angioedema associated with or unrelated to ACE inhibitors.
General Precautions
Renal Effects
Transient increases in BUN and Scr possible, especially in patients with preexisting renal impairment, sodium depletion, or hypovolemia; patients with renovascular hypertension, particularly those with bilateral renal-artery stenosis or those with renal-artery stenosis in a solitary kidney; or patients with chronic or severe hypertension in whom the glomerular filtration rate may decrease transiently.
Possible increases in BUN and Scr in patients with heart failure; rapidity of onset and magnitude may depend in part on degree of sodium depletion.
Closely monitor renal function following initiation of therapy in such patients. Some patients may require dosage reduction or discontinuance of ACE inhibitor or diuretic and/or adequate sodium repletion.
Hyperkalemia
Possible hyperkalemia, especially in patients with impaired renal function, heart failure, or diabetes mellitus and those receiving drugs that can increase serum potassium concentration (e.g., potassium-sparing diuretics, potassium supplements, potassium-containing salt substitutes). (See Interactions.)
Monitor serum potassium concentration carefully in these patients.
Cough
Persistent and nonproductive cough; resolves after drug discontinuance.
Valvular Stenosis
Possible risk of decreased coronary perfusion in patients with aortic stenosis when treated with captopril.
Use of Fixed Combinations
When used in fixed combination with hydrochlorothiazide, consider the cautions, precautions, and contraindications associated with hydrochlorothiazide.
Specific Populations
Pregnancy
Category C (1st trimester); Category D (2nd and 3rd trimesters). (See Fetal/Neonatal Morbidity and Mortality under Cautions and see Boxed Warning.)
Lactation
Distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established; however, captopril has been used in children. Manufacturer states that captopril should be used only when other measures for controlling BP have not been effective.
Possible excessive, prolonged, and unpredictable decreases in BP and associated complications (e.g., oliguria, seizures) in infants.
Renal Impairment
Systemic exposure to captopril may be increased. (See Special Populations under Pharmacokinetics.) Initial dosage adjustment recommended in patients with severe renal impairment. (See Renal Impairment under Dosage and Administration.)
Deterioration of renal function may occur. Possible increased risk of neutropenia/agranulocytosis, proteinuria, and hyperkalemia. (See Warnings and General Precautions under Cautions.)
Use of captopril/hydrochlorothiazide fixed combination usually is not recommended in patients with severe renal impairment.
Black Patients
BP reduction may be smaller in black patients compared with nonblack patients. (See Hypertension under Uses.)
Higher incidence of angioedema reported with ACE inhibitors in black patients compared with other races.
Common Adverse Effects
Rash, pruritus, cough, dysgeusia, proteinuria, tachycardia, chest pain, palpitations.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Adrenergic neuron blocking agents (guanethidine) |
Possible increased hypotensive effect |
Use with caution |
|
Antacids |
Decreased rate and extent of captopril absorption |
Clinical importance is uncertain |
|
Antidiabetic agents, oral |
Possible hypoglycemia in diabetic patients |
Consider risk of hypoglycemia if used concomitantly |
|
Allopurinol |
Pharmacokinetic interaction unlikely |
|
|
β-Adrenergic blocking agents |
Increased (but less than additive) hypotensive effect |
|
|
Cimetidine |
Neuropathy reported |
Further documentation of interaction necessary |
|
Digoxin |
Possible increased serum digoxin concentrations in patients with heart failure |
Monitor serum digoxin concentration; reduction of digoxin dosage not required upon initiation of captopril |
|
Diuretics |
Possible additive hypotensive effects Pharmacokinetic interaction with furosemide unlikely |
Adjust dosage carefully (see Dosage under Dosage and Administration) |
|
Diuretics, potassium-sparing (amiloride, spironolactone, triamterene) |
Possible hyperkalemia, especially in patients with renal impairment |
Use cautiously and only if hypokalemia is documented; monitor serum potassium carefully; discontinue or reduce dosage of potassium-sparing diuretic as necessary |
|
Insulin |
Possible hypoglycemia in diabetic patients |
Consider risk of hypoglycemia |
|
Lithium |
Possible increased serum lithium concentrations, particularly in patients receiving concomitant diuretic therapy |
Use with caution; monitor serum lithium concentrations frequently |
|
NSAIAs |
Possible decreased antihypertensive response to captopril; potential for acute reduction of renal function; possible attenuation of hemodynamic actions of ACE inhibitors in patients with heart failure |
Monitor BP carefully and be alert for evidence of impaired renal function; if interaction is suspected, discontinue NSAIA or modify captopril dosage or use another hypotensive agent |
|
Potassium supplements or potassium-containing salt substitutes |
Possible hyperkalemia, especially in patients with renal impairment |
Use cautiously and only if hypokalemia is documented; monitor serum potassium carefully; discontinue or reduce dosage of potassium supplement as necessary |
|
Probenecid |
Possible increased blood concentrations of captopril and its metabolites |
|
|
Test for urine acetone |
Possible false-positive results with sodium nitroprusside reagent |
|
|
Vasodilating agents (e.g., hydralazine, nitrates, prazosin) |
Possible increased hypotensive effect |
If possible, discontinue vasodilating agent before starting captopril; if vasodilating agent is resumed during captopril therapy, administer with caution and possibly at a lower dosage |
Captopril, Captopril and Hydrochlorothiazide Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration in fasting individuals, with peak blood concentration attained in 1 hour. Approximately 60–75% of an oral dose is absorbed.
Onset
Hypotensive effect may be apparent within 15 minutes and usually is maximal in 1–2 hours after a single oral dose. Several weeks of therapy may be required before full effect on BP is achieved.
Duration
Duration of action generally is 2–6 hours but appears to increase with increasing doses.
Food
Food may decrease absorption of captopril by up to 25–40%; effect may not be clinically important.
Distribution
Extent
Appears to be rapidly distributed into most body tissues, except CNS.
Crosses the placenta and is distributed into milk.
Plasma Protein Binding
25–30% (mainly albumin).
Elimination
Metabolism
About half the absorbed dose is rapidly metabolized. Captopril and its metabolites may undergo reversible interconversions.
Elimination Route
Excreted in urine (95%) as unchanged drug (40–50%) and metabolites.
Half-life
<2 hours.
Special Populations
Elimination half-life is about 20–40 hours in patients with Clcr <20 mL/minute and up to 6.5 days in anuric patients.
Stability
Storage
Oral
Tablets
Tight containers at ≤30°C.
Tablets (Captopril and Hydrochlorothiazide)
Tight containers at ≤30°C.
Actions
-
Suppresses the renin-angiotensin-aldosterone system.
Advice to Patients
-
Risk of angioedema, anaphylactoid reactions, or other sensitivity reactions. Importance of reporting sensitivity reactions (e.g., edema of face, eyes, lips, tongue, or extremities; hoarseness; swallowing or breathing with difficulty) immediately to clinician and of discontinuing the drug.
-
Importance of reporting signs of infection (e.g., sore throat, fever).
-
Risk of hypotension. Importance of informing clinicians promptly if lightheadedness or fainting occurs.
-
Importance of adequate fluid intake; risk of volume depletion with excessive perspiration, dehydration, vomiting, or diarrhea.
-
Importance of not discontinuing or interrupting therapy unless instructed by a clinician.
-
Risks of use during pregnancy. (See Boxed Warning.)
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs (including salt substitutes containing potassium) as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of taking 1 hour before meals.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
12.5 mg* |
Captopril Tablets |
|
|
25 mg* |
Captopril Tablets |
|||
|
50 mg* |
Captopril Tablets |
|||
|
100 mg* |
Captopril Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg Captopril and Hydrochlorothiazide 15 mg* |
Captopril and Hydrochlorothiazide Tablets |
|
|
25 mg Captopril and Hydrochlorothiazide 25 mg* |
Captopril and Hydrochlorothiazide Tablets |
Sandoz |
||
|
50 mg Captopril and Hydrochlorothiazide 15 mg* |
Captopril and Hydrochlorothiazide Tablets |
|||
|
50 mg Captopril and Hydrochlorothiazide 25 mg* |
Captopril and Hydrochlorothiazide Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about captopril
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
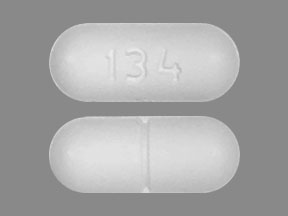
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: Angiotensin Converting Enzyme Inhibitors
- Breastfeeding
- En español