Tapentadol (Monograph)
Brand names: Nucynta, Nucynta ER
Drug class: Opioid Agonists
ATC class: N02AX06
VA class: CN101
Chemical name: 3-[(1R, 2R)-3-(dimethylamino)-1-ethyl-2-methylpropyl]phenol monohydrochloride
Molecular formula: C14H23NO HCL
CAS number: 175591-23-8
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for tapentadol to ensure that the benefits outweigh the risk. The REMS may apply to one or more preparations of tapentadol and consists of the following: medication guide and elements to assure safe use. See https://www.accessdata.fda.gov/scripts/cder/rems/.
-
FDA drug safety communication (4/13/2023): As part of its ongoing efforts to address the nation’s opioid crisis, FDA is requiring several updates to the prescribing information of opioid pain medicines. The changes are being made to provide additional guidance for safe use of these drugs while also recognizing the important benefits when used appropriately. The changes apply to both immediate-release (IR) and extended-release/long-acting preparations (ER/LA).
-
Updates to the IR opioids state that these drugs should not be used for an extended period unless the pain remains severe enough to require an opioid pain medicine and alternative treatment options are insufficient, and that many acute pain conditions treated in the outpatient setting require no more than a few days of an opioid pain medicine.
-
Updates to the ER/LA opioids recommend that these drugs be reserved for severe and persistent pain requiring an extended period of treatment with a daily opioid pain medicine and for which alternative treatment options are inadequate.
-
A new warning is being added about opioid-induced hyperalgesia (OIH) for both IR and ER/LA opioid pain medicines. This includes information describing the symptoms that differentiate OIH from opioid tolerance and withdrawal.
-
Information in the boxed warning for all IR and ER/LA opioid pain medicines will be updated and reordered to elevate the importance of warnings concerning life-threatening respiratory depression, and risks associated with using opioid pain medicines in conjunction with benzodiazepines or other medicines that depress the central nervous system (CNS).
-
Other changes will also be required in various other sections of the prescribing information to educate clinicians, patients, and caregivers about the risks of these drugs.
Warning
- Addiction, Abuse, and Misuse
-
Risk of addiction, abuse, and misuse, which can lead to overdosage and death. Assess each patient’s risk for addiction, abuse, and misuse before prescribing tapentadol; monitor all patients regularly for development of these behaviors or conditions. (See Addiction, Abuse, and Misuse under Cautions.)
- Respiratory Depression
-
Serious, life-threatening, or fatal respiratory depression may occur. Monitor for respiratory depression, especially during initiation of therapy and following dosage increases. (See Respiratory Depression under Cautions.)
-
Patients must swallow extended-release tablets whole to avoid exposure to a potentially fatal dose.
- Accidental Exposure
-
Accidental ingestion of even 1 dose, especially by a child, can result in a fatal overdose.
- Neonatal Opiate Withdrawal
-
Prolonged maternal use of opiates during pregnancy can result in neonatal withdrawal syndrome, which may be life-threatening if not recognized and treated. Advise women who require such therapy during pregnancy of this risk and ensure appropriate treatment will be available. (See Pregnancy under Cautions.)
- Concomitant Use with Benzodiazepines or Other CNS Depressants
-
Concomitant use of opiate agonists with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death.
-
Reserve concomitant use of opiate analgesics and benzodiazepines or other CNS depressants for patients in whom alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy and monitor closely for respiratory depression and sedation. (See Specific Drugs under Interactions.)
- Medication Errors with Oral Solutions
-
Potential for medication errors due to confusion between mg and mL; can result in inadvertent overdosage and death. Ensure accuracy in prescribing, dispensing, and administration. (See Oral Solution under Dosage and Administration.)
- Interaction with Alcohol
-
Consuming alcohol while receiving tapentadol extended-release tablets could result in increased plasma concentrations of the drug and a potentially fatal overdose; patients must not consume alcoholic beverages or take alcohol-containing prescription or nonprescription preparations during therapy with extended-release tablets.
Introduction
Synthetic, centrally active analgesic; structurally and pharmacologically related to tramadol.
Uses for Tapentadol
Pain
Conventional tablets or oral solution: Relief of acute pain that is severe enough to require an opiate analgesic and for which alternative treatment options (e.g., nonopiate analgesics, opiate-containing fixed combinations) have not been, or are not expected to be, adequate or tolerated.
Extended-release tablets: Management of pain (including neuropathic pain associated with diabetic peripheral neuropathy) that is severe enough to require long-term, daily, around-the-clock use of an opiate analgesic and for which alternative treatment options (e.g., nonopiate analgesics, immediate-release opiates) are inadequate or not tolerated. Not indicated for as-needed (“prn”) use.
In symptomatic treatment of acute pain, reserve opiate analgesics for pain resulting from severe injuries, severe medical conditions, or surgical procedures, or when nonopiate alternatives for relieving pain and restoring function are expected to be ineffective or are contraindicated. Use smallest effective dosage for shortest possible duration since long-term opiate use often begins with treatment of acute pain. Optimize concomitant use of other appropriate therapies. (See Managing Opiate Therapy for Acute Pain under Dosage and Administration.)
Generally use opiates for management of chronic pain (i.e., pain lasting >3 months or past the time of normal tissue healing ) that is not associated with active cancer treatment, palliative care, or end-of-life care only if other appropriate nonpharmacologic and nonopiate pharmacologic strategies have been ineffective and expected benefits for both pain relief and functional improvement are anticipated to outweigh risks.
If used for chronic pain, opiate analgesics should be part of an integrated approach that also includes appropriate nonpharmacologic modalities (e.g., cognitive-behavioral therapy, relaxation techniques, biofeedback, functional restoration, exercise therapy, certain interventional procedures) and other appropriate pharmacologic therapies (e.g., nonopiate analgesics, analgesic adjuncts such as selected anticonvulsants and antidepressants for certain neuropathic pain conditions).
Available evidence insufficient to determine whether long-term opiate therapy for chronic pain results in sustained pain relief or improvements in function and quality of life or is superior to other pharmacologic or nonpharmacologic treatments. Use is associated with serious risks (e.g., opiate use disorder [OUD], overdose). (See Managing Opiate Therapy for Chronic Noncancer Pain under Dosage and Administration.)
Tapentadol Dosage and Administration
General
Managing Opiate Therapy for Acute Pain
-
Optimize concomitant use of other appropriate therapies.
-
When opiate analgesia required, use conventional (immediate-release) opiates in smallest effective dosage and for shortest possible duration, since long-term opiate use often begins with treatment of acute pain.
-
Consider prescribing naloxone concomitantly for patients who are at increased risk of opiate overdosage or who have household members, including children, or other close contacts who are at risk for accidental ingestion or overdosage. (See Respiratory Depression under Cautions.)
-
When sufficient for pain management, use lower-potency opiate analgesics given in conjunction with acetaminophen or an NSAIA on as-needed (“prn”) basis.
-
For acute pain not related to trauma or surgery, limit prescribed quantity to amount needed for expected duration of pain severe enough to require opiate analgesia (generally ≤3 days and rarely >7 days). Do not prescribe larger quantities for use in case pain continues longer than expected; instead, reevaluate patient if severe acute pain does not remit.
-
For moderate to severe postoperative pain, provide opiate analgesic as part of a multimodal regimen that also includes acetaminophen and/or NSAIAs and other pharmacologic (e.g., certain anticonvulsants, regional local anesthetic techniques) and nonpharmacologic therapy as appropriate.
-
Oral administration of conventional opiate analgesics generally preferred over IV administration in postoperative patients who can tolerate oral therapy.
-
Scheduled (around-the-clock) dosing frequently is required during immediate postoperative period or following major surgery. When repeated parenteral administration is required, IV patient-controlled analgesia (PCA) generally is recommended.
Managing Opiate Therapy for Chronic Noncancer Pain
-
Although specific recommendations may vary, common elements in clinical guideline recommendations include risk mitigation strategies, upper dosage thresholds, careful dosage titration, and consideration of risks associated with particular opiates and formulations, coexisting diseases, and concomitant drug therapy.
-
Prior to initiating therapy, thoroughly evaluate patient; assess risk factors for misuse, abuse, and addiction; establish treatment goals (including realistic goals for pain and function); and consider how therapy will be discontinued if benefits do not outweigh risks.
-
Regard initial opiate therapy for chronic noncancer pain as a therapeutic trial that will be continued only if there are clinically meaningful improvements in pain and function that outweigh treatment risks.
-
Prior to and periodically during therapy, discuss with patients known risks and realistic benefits and patient and clinician responsibilities for managing therapy.
-
Some experts recommend initiating opiate therapy for chronic noncancer pain with conventional (immediate-release) opiate analgesics prescribed at lowest effective dosage. Individualize opiate selection, initial dosage, and dosage titration based on patient’s health status, prior opiate use, attainment of therapeutic goals, and predicted or observed harms.
-
Evaluate benefits and harms within 1–4 weeks following initiation of therapy or dosage increase and reevaluate on ongoing basis (e.g., at least every 3 months ) throughout therapy. Document pain intensity and level of functioning and assess progress toward therapeutic goals, presence of adverse effects, and adherence to prescribed therapies. Anticipate and manage common adverse effects (e.g., constipation, nausea and vomiting, cognitive and psychomotor impairment). If benefits do not outweigh harms, optimize other therapies and taper opiate to lower dosage or taper and discontinue opiate.
-
When repeated dosage increases required, evaluate potential causes and reassess relative benefits and risks. Although evidence is limited, some experts state that opiate rotation may be considered in patients with intolerable adverse effects or inadequate benefit despite dosage increases.
-
Higher dosages require particular caution, including more frequent and intensive monitoring or referral to specialist. Greater benefits of high-dose opiates for chronic pain not established in controlled clinical studies; higher dosages associated with increased risks (motor vehicle accidents, overdosage, OUD).
-
CDC states that primary care clinicians should carefully reassess individual benefits and risks before prescribing dosages equivalent to ≥50 mg of morphine sulfate daily for chronic pain and should avoid dosages equivalent to ≥90 mg of morphine sulfate daily or carefully justify decision to prescribe such dosages. Other experts recommend consulting a pain management specialist before exceeding a dosage equivalent to 80–120 mg of morphine sulfate daily. Some states have established opiate dosage thresholds (e.g., maximum daily dosages that can be prescribed, dosage thresholds at which consultation with specialist is mandated or recommended) or have mandated risk-management strategies (e.g., review of state prescription drug monitoring program [PDMP] data prior to prescribing).
-
Recommended strategies for managing risks include written treatment agreements or plans (e.g., “contracts”), urine drug testing, review of state PDMP data, and risk assessment and monitoring tools.
-
Taper and discontinue opiate therapy if patient engages in serious or repeated aberrant drug-related behaviors or drug abuse or diversion. Offer or arrange treatment for patients with OUD.
-
Consider prescribing naloxone concomitantly for patients who are at increased risk of opiate overdosage or who have household members, including children, or other close contacts who are at risk for accidental ingestion or overdosage. (See Respiratory Depression under Cautions.)
Administration
Oral Administration
Administer orally without regard to food.
Extended-release Tablets
Administer twice daily (approximately every 12 hours).
Administer tablets one at a time with enough water to ensure that each tablet is completely swallowed immediately after it is placed in the mouth.
Swallow tablets whole; do not crush, chew, or dissolve. Do not consume alcohol concomitantly. (See Boxed Warning.)
Oral Solution
Take care to ensure that the appropriate dose is communicated, dispensed, and administered. Prescriptions should specify the intended total dose of the drug (in mg) along with the corresponding total volume (in mL).
Always use the calibrated measuring device provided by the manufacturer to ensure that the dose is measured and administered accurately; use of a household spoon could result in overdosage.
Dosage
Available as tapentadol hydrochloride; dosage expressed in terms of tapentadol.
Use lowest effective dosage and shortest duration of therapy consistent with treatment goals of the patient.
Individualize dosage according to severity of pain, response, prior analgesic use, and risk factors for addiction, abuse, and misuse.
When used concomitantly with other CNS depressants, use lowest effective dosages and shortest possible duration of concomitant therapy. (See Specific Drugs under Interactions.)
Appropriate dosage selection and titration are essential to reduce the risk of respiratory depression. Monitor closely for respiratory depression, especially during the first 24–72 hours of therapy and following any increase in dosage.
Frequent communication among the prescriber, other members of the healthcare team, the patient, and the patient's caregiver or family is important during periods of changing analgesic requirements, including the initial dosage titration period.
Continually assess adequacy of pain control and reevaluate for adverse effects, as well as for development of addiction, abuse, or misuse. During long-term therapy, periodically reevaluate need for continued opiate therapy.
If level of pain increases after dosage stabilization, attempt to identify source of increased pain before increasing dosage.
When discontinuing tapentadol in a patient who may be physically dependent on opiates, generally reduce dosage by 25–50% every 2–4 days. If manifestations of withdrawal occur, increase dosage to the prior level and taper more slowly (increase interval between dosage reductions and/or reduce amount of each incremental change in dose).
Adults
Pain
Oral Solution or Conventional Tablets
OralInitially, 50–100 mg every 4–6 hours as needed. On day 1, patients not experiencing adequate pain relief may receive a second dose as early as 1 hour following first dose. Administer subsequent doses every 4–6 hours; adjust dosage to maintain adequate analgesia and minimize adverse effects.
Extended-release Tablets
OralOpiate naive or nontolerant patients: Initially, 50 mg every 12 hours. Higher initial dosages may result in fatal respiratory depression.
Patients switching from conventional tapentadol preparations to extended-release tapentadol tablets: Administer the total daily dosage of tapentadol in 2 divided doses at 12-hour intervals.
Patients switching from other opiates to tapentadol extended-release tablets: Initially, 50 mg every 12 hours. Dosage conversion factors not established in clinical trials. Monitor closely, particularly when switching from methadone since conversion ratios between methadone and other opiates vary widely depending on extent of prior methadone exposure and because methadone has a long half-life and tends to accumulate in plasma.
Discontinue all other tapentadol or tramadol preparations when therapy with tapentadol extended-release tablets is initiated.
Because of substantial interpatient variability in relative potency of opiate analgesics and analgesic formulations, it is preferable to underestimate the patient's 24-hour opiate requirements and provide “rescue” therapy with an immediate-release opiate analgesic than to overestimate the requirements and manage an adverse reaction.
Adjust dosage in increments of 50 mg no more than twice daily at intervals of every 3 days to provide adequate analgesia and acceptable adverse effects. Dosage range in clinical studies was 100–250 mg twice daily.
Patients with chronic pain who experience episodes of breakthrough pain may require dosage adjustment or supplemental analgesia (i.e., “rescue” therapy with an immediate-release analgesic).
Prescribing Limits
Adults
Pain
Oral
For acute pain not related to trauma or surgery, limit prescribed quantity to amount needed for the expected duration of pain severe enough to require opiate analgesia (generally ≤3 days and rarely >7 days).
CDC recommends that primary care clinicians carefully reassess individual benefits and risks before prescribing dosages equivalent to ≥50 mg of morphine sulfate daily for chronic pain and avoid dosages equivalent to ≥90 mg of morphine sulfate daily or carefully justify their decision to prescribe such dosages. Other experts recommend consulting a pain management specialist before exceeding a dosage equivalent to 80–120 mg of morphine sulfate daily.
Some states have set prescribing limits (e.g., maximum daily dosages that can be prescribed, dosage thresholds at which consultation with a specialist is mandated or recommended).
Oral Solution or Conventional Tablets
OralDosages >700 mg on day 1 and dosages >600 mg on subsequent days are not recommended.
Extended-release Tablets
Oral
Maximum 500 mg daily.
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh score 5–6): No dosage adjustment necessary.
Moderate hepatic impairment (Child-Pugh score 7–9): Initiate conventional tablets or oral solution at dosage of 50 mg administered no more frequently than once every 8 hours (maximum 3 doses in 24 hours); adjust subsequent dosage by shortening or lengthening the dosing interval. Initiate extended-release tablets at dosage of 50 mg administered no more frequently than once every 24 hours; maximum dosage of extended-release tablets is 100 mg daily.
Severe hepatic impairment (Child-Pugh score 10–15): Not recommended. (See Special Populations under Pharmacokinetics: Absorption and also under Pharmacokinetics: Elimination.)
Renal Impairment
Mild or moderate renal impairment (Clcr 30–90 mL/minute): No dosage adjustment necessary.
Severe renal impairment (Clcr <30 mL/minute): Not recommended. (See Special Populations under Pharmacokinetics: Elimination.)
Geriatric Patients
Cautious dosage selection; consider initiating tapentadol therapy at the lower end of the usual dosage range. Titrate dosage slowly with close monitoring for CNS and respiratory depression. (See Geriatric Use under Cautions.)
Cautions for Tapentadol
Contraindications
-
Substantial respiratory depression.
-
Acute or severe bronchial asthma or hypercarbia in unmonitored settings or in the absence of resuscitative equipment.
-
Known or suspected GI obstruction, including paralytic ileus.
-
Hypersensitivity (e.g., anaphylaxis, angioedema) to tapentadol or any ingredient in the formulation.
-
Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor.
Warnings/Precautions
Warnings
Addiction, Abuse, and Misuse
Risk of addiction, abuse, and misuse; addiction can occur at recommended dosages or with misuse or abuse. Abuse of tapentadol can result in overdosage and death; concurrent abuse of alcohol or other CNS depressants increases risk of toxicity. Abuse potential similar to that of other opiates. (See Actions.)
Assess each patient’s risk for addiction, abuse, and misuse prior to prescribing; monitor all patients for development of these behaviors or conditions. Personal or family history of substance abuse (drug or alcohol addiction or abuse) or mental illness (e.g., major depression) increases risk. The potential for addiction, abuse, and misuse should not prevent opiate prescribing for appropriate pain management, but does necessitate intensive counseling about risks and proper use and intensive monitoring for signs of addiction, abuse, and misuse.
Extended-release opiates are associated with a greater risk of overdosage and death because of the larger amount of drug contained in each dosage unit.
Abuse or misuse of tapentadol extended-release tablets by crushing or chewing the tablets, snorting the powder, or injecting the dissolved contents will result in uncontrolled delivery of the drug and can result in a fatal overdose. IV injection of tablet excipients can result in local tissue necrosis, infection, pulmonary granulomas, embolism, and death and increase the risk of endocarditis and valvular heart injury.
Prescribe in smallest appropriate quantity and instruct patients on secure storage and proper disposal to prevent theft.
Respiratory Depression
Serious, life-threatening, or fatal respiratory depression can occur with use of opiates, even when used as recommended; can occur at any time during therapy, but risk is greatest during initiation of therapy and following dosage increases. Monitor for respiratory depression, especially during first 24–72 hours of therapy and following any dosage increase.
Carbon dioxide retention from opiate-induced respiratory depression can exacerbate the drug's sedative effects and, in certain patients, can lead to elevated intracranial pressure. (See Increased Intracranial Pressure or Head Injury under Cautions.)
Geriatric, cachectic, or debilitated patients are at increased risk for life-threatening respiratory depression. Closely monitor such patients, particularly following initiation of therapy, during dosage titration, and during concomitant therapy with other respiratory depressants. Consider use of nonopiate analgesics.
Even recommended doses of tapentadol may decrease respiratory drive to the point of apnea in patients with COPD or cor pulmonale, substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression. Closely monitor such patients, particularly following initiation of therapy, during dosage titration, and during concomitant therapy with other respiratory depressants. Consider use of nonopiate analgesics.
Appropriate dosage selection and titration are essential to reduce the risk of respiratory depression. Overestimation of the dosage when transferring patients from another opiate analgesic can result in fatal overdosage with the first dose; large initial doses in nontolerant patients also can result in fatal overdosage.
Accidental ingestion of even 1 dose, especially by a child, can result in respiratory depression and fatal overdosage.
If respiratory depression occurs, follow usual guidelines for management of opiate agonist-induced respiratory depression.
Routinely discuss availability of the opiate antagonist naloxone with all patients receiving new or reauthorized prescriptions for opiate analgesics, including tapentadol.
Consider prescribing naloxone for patients receiving opiate analgesics who are at increased risk of opiate overdosage (e.g., those receiving concomitant therapy with benzodiazepines or other CNS depressants, those with history of opiate or substance use disorder, those with medical conditions that could increase sensitivity to opiate effects, those who have experienced a prior opiate overdose) or who have household members, including children, or other close contacts who are at risk for accidental ingestion or overdosage. Even if patients are not receiving an opiate analgesic, consider prescribing naloxone if the patient is at increased risk of opiate overdosage (e.g., those with current or past diagnosis of OUD, those who have experienced a prior opiate overdose).
Concomitant Use with Benzodiazepines or Other CNS Depressants
Concomitant use of opiates, including tapentadol, and benzodiazepines or other CNS depressants (e.g., anxiolytics, sedatives, hypnotics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opiate agonists, alcohol) may result in profound sedation, respiratory depression, coma, and death. Substantial proportion of fatal opiate overdoses involve concurrent benzodiazepine use.
Reserve concomitant use of tapentadol and other CNS depressants for patients in whom alternative treatment options are inadequate. (See Specific Drugs under Interactions.)
Dispensing and Administration Precautions with Oral Solution
Use caution when prescribing, dispensing, and administering tapentadol oral solution; dosing errors due to confusion between mg and mL can result in overdosage and death. Specify the intended total dose of the drug (in mg) along with the corresponding total volume (in mL). (See Oral Solution under Dosage and Administration.)
Interaction of Extended-release Tablets with Alcohol
Use of alcohol with tapentadol extended-release tablets may result in increased plasma concentrations of tapentadol and a potentially fatal overdose; patients must not consume alcoholic beverages or take prescription or nonprescription preparations containing alcohol concomitantly.
Other Warnings and Precautions
Only clinicians who are knowledgeable in the use of potent opiates for the management of chronic pain should prescribe tapentadol extended-release tablets.
Opiate Agonist Precautions
May cause effects similar to those produced by other opiate agonists; observe the usual precautions of opiate agonist therapy.
Serotonin Syndrome
Potentially life-threatening serotonin syndrome with SNRIs, including tapentadol, particularly with concurrent use of other serotonergic drugs or drugs that impair serotonin metabolism (e.g., MAO inhibitors). (See Actions and see Interactions.)
Manifestations may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile BP, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination, rigidity), and/or GI symptoms (e.g., nausea, vomiting, diarrhea).
Adrenal Insufficiency
Adrenal insufficiency reported in patients receiving opiate agonists or opiate partial agonists. Manifestations are nonspecific and may include nausea, vomiting, anorexia, fatigue, weakness, dizziness, and hypotension.
If adrenal insufficiency is suspected, perform appropriate laboratory testing promptly and provide physiologic (replacement) dosages of corticosteroids; taper and discontinue the opiate agonist or partial agonist to allow recovery of adrenal function. If the opiate agonist or partial agonist can be discontinued, perform follow-up assessment of adrenal function to determine if corticosteroid replacement therapy can be discontinued. In some patients, switching to a different opiate improved symptoms.
Hypotension
May cause severe hypotension, including orthostatic hypotension and syncope, in ambulatory patients, especially in individuals whose ability to maintain their BP is compromised by depleted blood volume or concomitant use of certain CNS depressants (e.g., phenothiazines, general anesthetics). Monitor BP following initiation of therapy and dosage increases in such patients. (See Specific Drugs under Interactions.)
Vasodilation produced by the drug may further reduce cardiac output and BP in patients with circulatory shock. Avoid use in such patients.
Increased Intracranial Pressure or Head Injury
Potential for increased carbon dioxide retention and secondary elevation of intracranial pressure; in patients particularly susceptible to these effects (e.g., those with evidence of elevated intracranial pressure or brain tumors), monitor closely for sedation and respiratory depression, particularly during initiation of therapy.
Opiates may obscure the clinical course in patients with head injuries.
Avoid use in patients with impaired consciousness or coma.
GI Conditions
May cause spasm of the sphincter of Oddi and increase serum amylase concentrations; monitor patients with biliary disease, including acute pancreatitis, for worsening symptoms.
Contraindicated in patients with known or suspected GI obstruction, including paralytic ileus.
Seizures
May aggravate preexisting seizure disorder. Monitor for worsened seizure control.
May increase risk of seizures in other settings associated with seizures.
Dependence and Tolerance
Physical dependence and tolerance can develop during prolonged therapy. Abrupt discontinuance or substantial dosage reduction may result in symptoms of withdrawal (e.g., restlessness, lacrimation, rhinorrhea, yawning, sweating, chills, myalgia, mydriasis, irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, increased BP, respiratory rate, or heart rate). Symptoms may be avoided by tapering the dosage when the drug is discontinued.
Avoid concomitant use of opiate partial agonists. (See Specific Drugs under Interactions.)
Infants born to women who are physically dependent on opiates also will be physically dependent. (See Pregnancy under Cautions.)
CNS Depression
Performance of activities requiring mental alertness and/or physical coordination (e.g., driving, operating machinery) may be impaired. (See Advice to Patients.)
Concurrent use with other CNS depressants may result in profound sedation, respiratory depression, coma, or death. (See Concomitant Use with Benzodiazepines or Other CNS Depressants under Cautions.)
Hypogonadism
Hypogonadism or androgen deficiency reported in patients receiving long-term opiate agonist or opiate partial agonist therapy; causality not established. Manifestations may include decreased libido, impotence, erectile dysfunction, amenorrhea, or infertility. Perform appropriate laboratory testing in patients with manifestations of hypogonadism.
Specific Populations
Pregnancy
Category C.
Analysis of data from the National Birth Defects Prevention Study (large population-based, case-control study) suggests therapeutic use of opiates in pregnant women during organogenesis is associated with a low absolute risk of birth defects, including heart defects, spina bifida, and gastroschisis. Manufacturer states that data for tapentadol are insufficient to establish risk of major birth defects and spontaneous abortion.
In animal studies, embryofetal toxicity observed with tapentadol given at maternally toxic dosages. Based on animal data, apprise patients of potential fetal risk if used during pregnancy.
Use of opiates in pregnant women during labor can result in neonatal respiratory depression. Use of tapentadol immediately before or during labor is not recommended. Monitor neonates exposed to opiates during labor for respiratory depression and excessive sedation; an opiate antagonist should be readily available for reversal of opiate-induced respiratory depression.
Prolonged maternal use of opiates during pregnancy can result in neonatal opiate withdrawal syndrome; in contrast to adults, withdrawal syndrome in neonates may be life-threatening and requires management according to protocols developed by neonatology experts. Syndrome presents with irritability, hyperactivity and abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. Onset, duration, and severity vary depending on the specific opiate used, duration of use, timing and amount of last maternal use, and rate of drug elimination by the neonate.
Lactation
Limited data suggest tapentadol may distribute into milk; risk to nursing infants cannot be ruled out.
Consider benefits of breast-feeding and importance of the drug to the woman; also consider potential adverse effects on the breast-fed infant from the drug or underlying maternal condition. Breast-feeding not recommended during therapy with tapentadol extended-release tablets.
Monitor infants exposed to tapentadol through breast milk for excessive sedation and respiratory depression. Symptoms of withdrawal can occur in opiate-dependent infants when maternal administration of opiates is discontinued or breast-feeding is stopped.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
No overall differences in efficacy of tapentadol in those ≥65 years of age compared with younger adults. Incidence of constipation with conventional tablets was higher in patients ≥65 years of age compared with those <65 years of age (12 versus 7%). (See Special Populations under Pharmacokinetics: Absorption.)
Respiratory depression is the chief risk; monitor closely for CNS and respiratory depression.
Select dosage with caution because of greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy in geriatric patients.
May be useful to monitor renal function; tapentadol clearance may be decreased and risk of adverse effects increased in patients with impaired renal function.
Hepatic Impairment
Higher serum tapentadol concentrations reported in patients with hepatic impairment compared with individuals without impairment. (See Special Populations under Pharmacokinetics: Absorption.) Reduce dosage in patients with moderate hepatic impairment and closely monitor for respiratory and CNS depression. (See Hepatic Impairment under Dosage and Administration.)
Not studied and, therefore, not recommended in patients with severe hepatic impairment.
Renal Impairment
Increased exposure of O-glucuronide metabolite in patients with renal impairment; clinical importance of glucuronide metabolite accumulation not known. Use not recommended in patients with severe renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Nausea, dizziness, vomiting, somnolence, constipation, pruritus, dry mouth, hyperhidrosis, fatigue, headache, vomiting, diarrhea, decreased appetite, anxiety, insomnia, dyspepsia, hot flush. In several clinical studies, adverse GI effects (nausea, vomiting, constipation) reported more commonly with oxycodone than with tapentadol.
Drug Interactions
Metabolized primarily by glucuronidation.
Metabolized to a lesser extent by CYP isoenzymes 2C9, 2C19, and 2D6.
Does not induce CYP isoenzymes 1A2, 2D6, or 3A4 and does not inhibit CYP isoenzymes 1A2, 2A6, 2C9, 2C19, 2E1, or 3A4 in vitro. Inhibits CYP2D6 to a limited extent in vitro.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Clinically relevant CYP-mediated interactions are unlikely.
Drugs Associated with Serotonin Syndrome
Risk of serotonin syndrome when used with other serotonergic agents. May occur at usual dosages. Symptom onset generally occurs within several hours to a few days of concomitant use, but may occur later, particularly after dosage increases. (See Advice to Patients and see Actions.)
If concomitant use of other serotonergic drugs is warranted, monitor patients for serotonin syndrome, particularly during initiation of therapy and dosage increases.
If serotonin syndrome is suspected, discontinue tapentadol, other opiate therapy, and/or any concurrently administered serotonergic agents.
Protein-bound Drugs
Pharmacokinetic interaction unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Acetaminophen did not affect pharmacokinetics of tapentadol |
|
|
Anticholinergic agents |
Possible increased risk of urinary retention and/or severe constipation, which may lead to paralytic ileus |
Monitor for urinary retention or reduced gastric motility |
|
Antidepressants, SSRIs (e.g., citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline), SNRIs (e.g., desvenlafaxine, duloxetine, milnacipran, venlafaxine), tricyclic antidepressants (TCAs), mirtazapine, nefazodone, trazodone, vilazodone |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, the antidepressant, and/or any concurrently administered opiates or serotonergic agents |
|
Antiemetics, 5-HT3 receptor antagonists (e.g., dolasetron, granisetron, ondansetron, palonosetron) |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, the 5-HT3 receptor antagonist, and/or any concurrently administered opiates or serotonergic agents |
|
Aspirin |
Aspirin did not affect pharmacokinetics of tapentadol |
|
|
Antipsychotics (e.g., aripiprazole, asenapine, cariprazine, chlorpromazine, clozapine, fluphenazine, haloperidol, iloperidone, loxapine, lurasidone, molindone, olanzapine, paliperidone, perphenazine, pimavanserin, quetiapine, risperidone, thioridazine, thiothixene, trifluoperazine, ziprasidone) |
Risk of profound sedation, respiratory depression, hypotension, coma, or death |
Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy In patients receiving tapentadol, initiate antipsychotic, if required, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response In patients receiving an antipsychotic, initiate tapentadol, if required, at reduced dosage and titrate based on clinical response Monitor closely for respiratory depression and sedation |
|
Benzodiazepines (e.g., alprazolam, chlordiazepoxide, clobazam, clonazepam, clorazepate, diazepam, estazolam, flurazepam, lorazepam, midazolam, oxazepam, quazepam, temazepam, triazolam) |
Risk of profound sedation, respiratory depression, hypotension, coma, or death |
Whenever possible, avoid concomitant use Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy In patients receiving tapentadol, initiate benzodiazepine, if required for any indication other than epilepsy, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response In patients receiving a benzodiazepine, initiate tapentadol, if required, at reduced dosage and titrate based on clinical response Monitor closely for respiratory depression and sedation Consider prescribing naloxone for patients receiving opiates and benzodiazepines concomitantly |
|
Buspirone |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, buspirone, and/or any concurrently administered opiates or serotonergic agents |
|
CNS depressants (e.g., alcohol, other opiates, anxiolytics, general anesthetics, antiemetics, tranquilizers, phenothiazines) |
Additive CNS depression; increased risk of profound sedation, respiratory depression, hypotension, coma, or death Alcohol: Increased peak plasma concentrations and AUC with extended-release tablets; may result in fatal overdosage |
Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy In patients receiving tapentadol, initiate CNS depressant, if required for any indication other than epilepsy, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response In patients receiving a CNS depressant, initiate tapentadol, if required, at reduced dosage and titrate based on clinical response Monitor closely for respiratory depression and sedation Consider prescribing naloxone for patients receiving opiates and other CNS depressants concomitantly Avoid alcohol use |
|
Dextromethorphan |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, dextromethorphan, and/or any concurrently administered opiates or serotonergic agents |
|
Diuretics |
Opiates may decrease diuretic efficacy by inducing vasopressin release |
Monitor for reduced diuretic and/or BP effects; increase diuretic dosage as needed |
|
5-HT1 receptor agonists (triptans; e.g., almotriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan, zolmitriptan) |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, the triptan, and/or any concurrently administered opiates or serotonergic agents |
|
Lithium |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, lithium, and/or any concurrently administered opiates or serotonergic agents |
|
MAO inhibitors (e.g., isocarboxazid, linezolid, methylene blue, phenelzine, selegiline, tranylcypromine) |
Risk of serotonin syndrome |
Tapentadol contraindicated in patients currently receiving or having recently (within 2 weeks) received MAO inhibitors |
|
Metoclopramide |
Metoclopramide did not affect pharmacokinetics of tapentadol |
|
|
Naproxen |
Naproxen increased tapentadol AUC by 17%; not considered clinically relevant |
Dosage adjustments not necessary |
|
Neuromuscular blocking agents |
Possible enhanced neuromuscular blocking effect resulting in increased respiratory depression |
Monitor for respiratory depression; reduce dosage of one or both agents as necessary |
|
Omeprazole |
Omeprazole did not affect pharmacokinetics of tapentadol |
|
|
Opiate partial agonists (butorphanol, buprenorphine, nalbuphine, pentazocine) |
Possible reduced analgesic effect and/or withdrawal symptoms |
Avoid concomitant use |
|
Probenecid |
Probenecid increased tapentadol AUC by 57%; not considered clinically relevant |
Dosage adjustments not necessary |
|
Sedative/hypnotic agents (e.g., butabarbital, eszopiclone, pentobarbital, ramelteon, secobarbital, suvorexant, zaleplon, zolpidem) |
Risk of profound sedation, respiratory depression, hypotension, coma, or death |
Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy In patients receiving tapentadol, initiate sedative/hypnotic, if required, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response In patients receiving a sedative/hypnotic, initiate tapentadol, if required, at reduced dosage and titrate based on clinical response Monitor closely for respiratory depression and sedation |
|
Skeletal muscle relaxants (e.g., baclofen, carisoprodol, chlorzoxazone, cyclobenzaprine, dantrolene, metaxalone, methocarbamol, orphenadrine, tizanidine) |
Risk of profound sedation, respiratory depression, hypotension, coma, or death Cyclobenzaprine: Risk of serotonin syndrome |
Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy In patients receiving tapentadol, initiate skeletal muscle relaxant, if required, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response In patients receiving a skeletal muscle relaxant, initiate tapentadol, if required, at reduced dosage and titrate based on clinical response Monitor closely for respiratory depression and sedation Cyclobenzaprine: If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, cyclobenzaprine, and/or any concurrently administered opiates or serotonergic agents |
|
St. John’s wort (Hypericum perforatum) |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, St. John's wort, and/or any concurrently administered opiates or serotonergic agents |
|
Tryptophan |
Risk of serotonin syndrome |
If concomitant use warranted, monitor for serotonin syndrome, particularly during initiation of therapy and dosage increases If serotonin syndrome suspected, discontinue tapentadol, tryptophan, and/or any concurrently administered opiates or serotonergic agents |
Tapentadol Pharmacokinetics
Absorption
Bioavailability
Mean absolute bioavailability is approximately 32% following a single oral dose.
Immediate-release preparations: Peak plasma concentrations attained approximately 1.25 hours following oral administration. Peak plasma concentration and AUC are dose proportional over dosing range of 50–150 mg.
Extended-release tablets: Peak plasma concentrations attained 3–6 hours following oral administration. AUC is dose proportional over the therapeutic dosage range. Steady-state tapentadol exposure attained after the third dose (on a twice-daily schedule).
Food
Immediate-release preparations: High-fat, high-calorie meal increases tapentadol AUC by 25% and peak plasma concentration by 16%.
Extended-release tablets: High-fat, high-calorie meal increases tapentadol AUC by 6% and peak plasma concentration by 17%.
Special Populations
Mean peak plasma tapentadol concentrations were 16% lower in geriatric patients compared with younger adults; AUCs were similar.
In patients with mild hepatic impairment, tapentadol AUC and peak plasma concentration were increased 1.7- and 1.4-fold, respectively; in those with moderate hepatic impairment, AUC and peak plasma concentration were increased 4.2- and 2.5-fold, respectively.
Distribution
Extent
Widely distributed throughout the body.
May distribute into human milk.
Plasma Protein Binding
Approximately 20%.
Elimination
Metabolism
Principally undergoes conjugation with glucuronic acid to form inactive metabolites; major inactive metabolite, tapentadol-O-glucuronide, formed via uridine diphosphate-glucuronosyltransferase enzymes (UGT) 1A9 and 2B7.
Metabolized to a lesser extent by CYP2C9 and CYP2C19 to form N-desmethyl tapentadol and by CYP2D6 to form hydroxytapentadol, both of which undergo secondary conjugation.
Elimination Route
Tapentadol and its metabolites are excreted mainly (99%) by the kidneys. Following oral administration, approximately 70% of a dose is excreted in urine as conjugates (55% as O-glucuronide and 15% as sulfate conjugate of tapentadol); 3% of a dose is eliminated as unchanged drug.
Half-life
Immediate-release preparations: Mean terminal half-life is 4 hours.
Extended-release tablets: Mean terminal half-life is 5 hours.
Special Populations
In patients with increased hepatic impairment, rate of formation of tapentadol-O-glucuronide was reduced. Tapentadol half-life was increased 1.2- or 1.4-fold in patients with mild or moderate hepatic impairment, respectively.
In patients with mild, moderate, or severe renal impairment, AUC of tapentadol-O-glucuronide is 1.5-, 2.5-, or 5.5-fold higher, respectively, than AUC in patients with normal renal function.
Stability
Storage
Oral
Conventional Tablets
≤25°C (may be exposed to 15–30°C). Protect from moisture.
Extended-release Tablets
20–25°C (may be exposed to 15–30°C). Protect from moisture.
Oral Solution
≤25°C (may be exposed to 15–30°C). Store bottle upright after opening.
Actions
-
Precise mechanism of analgesic action unknown; thought to be related to agonist activity at the μ-opiate receptor and inhibition of norepinephrine reuptake.
-
Also inhibits serotonin reuptake, but serotonergic activity is much lower than noradrenergic activity.
-
Inhibition of norepinephrine reuptake may work synergistically with μ-receptor activation to enhance analgesic efficacy and/or attenuate adverse effects seen with traditional opiate analgesics (e.g., GI effects) by reducing the requirement for μ-receptor activation.
-
Animal data indicate that tapentadol is almost as potent as venlafaxine in inhibiting the reuptake of norepinephrine.
-
Tapentadol is 2–3 times less potent than morphine in producing analgesia in animals.
-
Possesses a reduced emetogenic potential compared with morphine and produces less physical dependence at equianalgesic doses.
-
Abuse potential is similar to that seen with other potent opiates, including fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, and oxymorphone, but appears to be greater than that seen with tramadol. Tapentadol is subject to control under the Federal Controlled Substances Act of 1970 as a schedule II drug; tramadol originally was not subject to control but currently is a schedule IV drug.
-
Possesses weak antagonist activity for muscarinic receptors.
Advice to Patients
-
Importance of reading the patient information (medication guide) provided by the manufacturer before initiating therapy and each time the prescription is refilled.
-
Importance of taking tapentadol only as directed; do not increase dosage or abruptly discontinue therapy without consulting a clinician; abrupt discontinuance may precipitate withdrawal symptoms.
-
Importance of instructing patients on proper administration of the drug. Importance of always using the calibrated oral syringe when administering tapentadol oral solution; use of a household spoon could result in overdosage.
-
Importance of swallowing extended-release tablets whole with enough water to ensure complete swallowing of the tablet immediately after it is placed in the mouth. Do not cut, crush, chew, or dissolve extended-release tablets.
-
Potential for addiction, abuse, and misuse, which can lead to overdosage or death, even when used as recommended. Protect from theft or misuse; properly dispose of any unused drug, and do not share tapentadol with others.
-
Risk of potentially fatal respiratory depression; most likely to occur following initiation of therapy and dosage increases; may occur at recommended dosages. Importance of seeking immediate medical attention if signs or symptoms of respiratory depression occur. Advise patients of the benefits of naloxone following opiate overdose and of their options for obtaining the drug.
-
Accidental ingestion, especially by a child, may result in respiratory depression or death. Importance of keeping tapentadol out of reach of children.
-
Risk of potentially fatal additive effects (e.g., profound sedation, respiratory depression, coma) if used concomitantly with benzodiazepines or other CNS depressants, including alcohol and other opiates, either therapeutically or illicitly; avoid concomitant use unless such use is supervised by clinician. Advise patients that tapentadol should not be combined with alcohol.
-
Risk of orthostatic hypotension and syncope.
-
Potential for tapentadol to impair mental alertness and/or physical coordination; avoid driving or operating machinery until effects on individual are known.
-
Potential for severe constipation; advise patients on appropriate management.
-
Potential risk of serotonin syndrome with concurrent use of tapentadol and other serotonergic agents. Importance of immediately contacting clinician if manifestations of serotonin syndrome (e.g., agitation, hallucinations, tachycardia, labile BP, fever, excessive sweating, shivering, shaking, muscle stiffness, twitching, loss of coordination, nausea, vomiting, diarrhea) develop.
-
Potential risk of adrenal insufficiency. Importance of contacting clinician if manifestations of adrenal insufficiency (e.g., nausea, vomiting, loss of appetite, fatigue, weakness, dizziness, hypotension) develop.
-
Possible risk (although causality not established) of hypogonadism or androgen deficiency with long-term opiate agonist or partial agonist use. Importance of informing clinician if decreased libido, impotence, erectile dysfunction, amenorrhea, or infertility occurs.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses. Importance of avoiding concomitant therapy with MAO inhibitors.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of informing women that tapentadol may cause fetal harm and that chronic use during pregnancy may result in neonatal opiate withdrawal syndrome, which can be life-threatening if not recognized and treated.
-
Importance of immediately seeking medical attention if an infant exposed to tapentadol through breast milk exhibits symptoms of opiate overdosage (e.g., sedation, difficulty breathing, hypotonia). Advise patients that breast-feeding during therapy with extended-release tapentadol is not recommended.
-
Importance of informing patients with a history of seizures that tapentadol may precipitate seizures and of advising them to use tapentadol with care. Importance of advising patients to discontinue tapentadol if seizures occur and to contact their clinician immediately.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as schedule II (C-II) drug.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
100 mg (of tapentadol) per 5 mL |
Nucynta Oral Solution (C-II) |
Depomed |
|
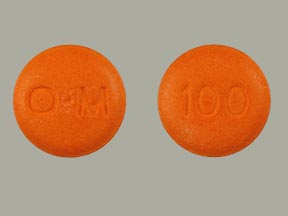
Tablets, extended-release, film-coated |
50 mg (of tapentadol) |
Nucynta ER (C-II) |
Depomed |
|
|
100 mg (of tapentadol) |
Nucynta ER (C-II) |
Depomed |
||
|
150 mg (of tapentadol) |
Nucynta ER (C-II) |
Depomed |
||
|
200 mg (of tapentadol) |
Nucynta ER (C-II) |
Depomed |
||
|
250 mg (of tapentadol) |
Nucynta ER (C-II) |
Depomed |
||
|
Tablets, film-coated |
50 mg (of tapentadol) |
Nucynta (C-II) |
Depomed |
|
|
75 mg (of tapentadol) |
Nucynta (C-II) |
Depomed |
||
|
100 mg (of tapentadol) |
Nucynta (C-II) |
Depomed |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 19, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about tapentadol
- Check interactions
- Compare alternatives
- Reviews (438)
- Side effects
- Dosage information
- During pregnancy
- Drug class: Opioids (narcotic analgesics)
- Breastfeeding
- En español