Relugolix (Monograph)
Brand name: Orgovyx
Drug class: Antigonadotropins
Introduction
Antineoplastic agent; gonadotropin-releasing hormone (GnRH, luteinizing hormone-releasing hormone [LHRH], gonadorelin) antagonist.
Uses for Relugolix
Prostate Cancer
Treatment of advanced prostate cancer in adults.
Medical castration (defined as serum total testosterone concentration <50 ng/dL) achieved sooner with relugolix compared with leuprolide.
Relugolix Dosage and Administration
General
Pretreatment Screening
-
Weigh benefits of androgen deprivation therapy against potential risks in patients with congenital long QT syndrome, CHF, or frequent electrolyte abnormalities, and in patients receiving drugs known to prolong the QT interval.
-
Correct electrolyte abnormalities.
Patient Monitoring
-
Consider periodic monitoring of ECGs and electrolytes.
-
Periodically measure prostate-specific antigen (PSA) concentrations to monitor response to the drug.
-
If serum PSA concentrations increase, measure serum testosterone concentrations.
Administration
Oral Administration
Administer orally with a loading dose on the first day followed by once daily dosing at approximately the same time each day without regard to food. Swallow tablets whole; do not crush or chew.
If a dose is missed, administer the missed dose as soon as it is remembered. If a dose is missed by >12 hours, do not administer the missed dose; instead, resume therapy with the next scheduled dose.
Dosage
Adults
Prostate Cancer
Oral
Initial loading dose of 360 mg, followed by 120 mg once daily. Following development of nonmetastatic or metastatic castration-resistant prostate cancer, therapy with GnRH receptor agonists and antagonists usually is continued.
If relugolix therapy is interrupted for >7 days, reinitiate treatment with a loading dose of 360 mg on the first day, followed by 120 mg once daily.
Dosage Modifications with P-gp Inhibitor Use
Avoid concomitant use of relugolix with oral P-gp inhibitors. If unavoidable, administer relugolix first and separate from the P-gp inhibitor by ≥6 hours. May interrupt relugolix therapy for up to 2 weeks if short-term therapy with a P-gp inhibitor is required.
Dosage Modifications with Combined P-gp and Strong CYP3A Inducer Use
Avoid concomitant use of relugolix with a combined P-gp and strong CYP3A inducer. If unavoidable, increase the relugolix dosage to 240 mg once daily. Resume the recommended relugolix dosage of 120 mg once daily after discontinuation of the combined P-gp and strong CYP3A inducer.
Special Populations
Manufacturer makes no special population dosage recommendations.
Cautions for Relugolix
Contraindications
-
Severe hypersensitivity to relugolix or any of its components.
Warnings/Precautions
Prolongation of QT Interval
Androgen deprivation therapy may prolong the QT interval.
Weigh benefits of androgen deprivation therapy against potential risks in patients with congenital long QT syndrome, CHF, or frequent electrolyte abnormalities and in patients receiving drugs known to prolong the QT interval.
Correct electrolyte abnormalities and consider periodic monitoring of ECGs and electrolytes.
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., pharyngeal edema and other serious cases of angioedema) reported. Temporarily discontinue relugolix and seek immediate medical care if symptoms of angioedema occur. Discontinue relugolix and manage as clinically indicated if a severe hypersensitivity reaction occurs.
Fetal/Neonatal Morbidity and Mortality
Safety and efficacy of relugolix not established in females. May cause fetal harm and loss of pregnancy; embryofetal lethality (abortion, total litter loss, decreased number of live fetuses) demonstrated in animals.
Advise patients of potential for fetal harm and loss of pregnancy. Advise men who have female partners of reproductive potential to use effective methods of contraception during relugolix therapy and for 2 weeks after the last dose of the drug.
Laboratory Testing
Relugolix therapy suppresses pituitary-gonadal system; may affect results of diagnostic tests of pituitary gonadotropic and gonadal functions performed during and after therapy. Periodically measure prostate-specific antigen (PSA) concentrations to monitor response to the drug. If serum PSA concentrations increase, measure serum testosterone concentrations.
Specific Populations
Pregnancy
Safety and efficacy not established in females. No data on use in pregnant women; however, based on animal studies and mechanism of action, relugolix can cause fetal harm.
Lactation
Safety and efficacy at recommended dosage of 120 mg daily not established in females. Not known whether relugolix distributes into human milk, affects breast-fed infants, or affects milk production. Relugolix and/or its metabolites distribute into milk in rats.
Females and Males of Reproductive Potential
Advise patients of potential for fetal harm and loss of pregnancy. Advise men who have female partners of reproductive potential to use effective methods of contraception during relugolix therapy and for 2 weeks after the last dose.
May impair fertility in males of reproductive potential.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
In primary prostate cancer efficacy study, 81% of patients receiving relugolix were ≥65 years of age and 35% were ≥75 years of age. No overall differences in safety or efficacy observed between geriatric patients and younger adults.
Hepatic Impairment
No clinically important differences in pharmacokinetics of relugolix observed in patients with mild to moderate hepatic impairment (Child-Pugh class A or B). Effect of severe hepatic impairment (Child-Pugh class C) on pharmacokinetics of relugolix not established.
Renal Impairment
No clinically important differences in pharmacokinetics of relugolix observed in patients with mild to severe renal impairment (Clcr15–89 mL/minute). Effect of end-stage renal disease with or without hemodialysis on pharmacokinetics of relugolix not established.
Common Adverse Effects
Adverse effects or laboratory abnormalities reported in ≥10 or ≥15%, respectively: Hot flush, musculoskeletal pain, fatigue, constipation, increased glucose concentrations, increased triglyceride concentrations, decreased hemoglobin, increased ALT and AST concentrations.
Drug Interactions
Substrate of CYP3A and CYP2C8. Does not inhibit CYP isoenzyme 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4. Induces CYP3A and CYP2B6; does not induce CYP1A2.
Substrate and inhibitor of P-gp. Inhibitor but not a substrate of breast cancer resistance protein (BCRP). Does not inhibit organic anion transport protein (OATP) 1B1 or 1B3, organic anion transporter (OAT) 1 or 3, organic cation transporter (OCT) 2, multidrug and toxin extrusion transporter (MATE) 1 or 2-K, or bile salt export pump (BSEP).
Drugs Affecting P-gp Transport System
Oral P-gp inhibitors: Increased peak plasma concentrations and AUC of relugolix, which may increase risk of adverse effects. Intestinal P-gp efflux is the primary determinant of relugolix absorption and oral bioavailability. Inhibition of intestinal P-gp efflux appears to be primarily responsible for the increase in relugolix exposure following simultaneous administration of an oral P-gp inhibitor. Avoid concomitant use; if concomitant use cannot be avoided, administer relugolix at least 6 hours before the P-gp inhibitor and monitor more frequently for adverse effects. May interrupt relugolix therapy for up to 2 weeks if short-term P-gp inhibitor therapy required.
Drugs Affecting Hepatic Microsomal Enzymes and P-gp Transport System
Combined P-gp inducer and potent CYP3A inducer: Decreased relugolix exposure, which may reduce efficacy. Avoid concomitant use. If concomitant use cannot be avoided, increase relugolix dosage to 240 mg once daily; following discontinuance of concomitant therapy, reduce relugolix dosage to 120 mg daily.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acid suppressants (e.g., proton-pump inhibitors, histamine H2-receptor antagonists) |
No clinically important effects on pharmacokinetics of relugolix |
|
|
Atorvastatin |
No clinically important effects of atorvastatin (weak CYP3A inhibitor) on pharmacokinetics of relugolix |
|
|
Enzalutamide |
No clinically important effects on pharmacokinetics of relugolix |
|
|
Erythromycin |
Erythromycin (potent P-gp inhibitor and moderate CYP3A inhibitor) increased AUC and peak plasma concentration of relugolix by 6.2-fold |
Avoid concomitant use; if concomitant use required, administer relugolix at least 6 hours before oral erythromycin and monitor more frequently for adverse effects May interrupt relugolix therapy for up to 2 weeks if short-term P-gp inhibitor therapy required |
|
Midazolam |
No clinically important effects on pharmacokinetics of midazolam (CYP3A substrate) |
|
|
Rifampin |
Rifampin (P-gp inducer and potent CYP3A inducer) decreased AUC and peak plasma concentrations of relugolix by 55 and 23%, respectively |
Avoid concomitant use; if concomitant use required, increase relugolix dosage to 240 mg once daily; following discontinuance of rifampin, reduce relugolix dosage to 120 mg once daily |
|
Rosuvastatin |
No clinically important effects on pharmacokinetics of rosuvastatin (BCRP substrate) |
|
|
Voriconazole |
No clinically important effects of voriconazole (potent CYP3A inhibitor without P-gp inhibitory activity) on pharmacokinetics of relugolix |
Relugolix Pharmacokinetics
Absorption
Bioavailability
Intestinal P-gp efflux is primary determinant of relugolix absorption and oral bioavailability. Following oral administration, mean absolute bioavailability is approximately 12%; peak concentrations are achieved at a median of 2.25 hours.
With once-daily oral administration, accumulation of relugolix is approximately twofold.
Food
Administration with high-calorie, high-fat meal decreases relugolix absorption by approximately 20%; effect not considered clinically important.
Distribution
Extent
Distributes into milk in rats.
Plasma Protein Binding
68–71% bound to plasma proteins (mainly albumin and to a lesser extent α1-acid glycoprotein).
Elimination
Metabolism
Metabolized mainly by CYP3A and to a lesser extent by CYP2C8 and other minor pathways.
Elimination Route
Excreted mainly as metabolites in feces (81%) and urine (4.1%); only about 6.4% of dose is recovered as unchanged drug.
Half-life
Mean effective half-life: 25 hours.
Mean terminal elimination half-life: Approximately 61 hours.
Special Populations
Age (45–91 years), race/ethnicity, body weight (41–193 kg), mild to severe renal impairment (Clcr 15–89 mL/minute), and mild to moderate hepatic impairment (Child-Pugh class A or B) have no clinically important effects on pharmacokinetics.
Stability
Storage
Oral
Tablets
Room temperature (≤30°C). Dispense in original container only. Keep bottle tightly closed after first opening.
Actions
-
Oral nonpeptide GnRH antagonist.
-
Rapidly, competitively, and reversibly binds to and blocks GnRH receptors in the pituitary, thereby reducing the release of gonadotropins (i.e., LH, FSH) and, consequently, testosterone without initial stimulation of the hypothalamic-pituitary-gonadal axis and the associated testosterone surge.
Advice to Patients
-
Advise patients to read the manufacturer's patient information for relugolix.
-
Advise patients that relugolix may prolong the QT interval and that they should contact their clinician immediately if signs or symptoms of QT-interval prolongation (e.g., dizziness, fainting, palpitations, chest pain) occur.
-
Inform patients that relugolix may cause serious hypersensitivity reactions including angioedema. Advise patients to discontinue relugolix if hypersensitivity symptoms occur and to promptly contact their clinician.
-
Inform patients of the risk of hot flushes, flushing of the skin, weight gain, decreased sex drive, and difficulties with erectile function.
-
Potential for relugolix to cause fetal harm and loss of pregnancy. Advise male patients with female partners of reproductive potential that they should use effective methods of contraception during relugolix therapy and for 2 weeks after the last dose of the drug.
-
Inform patients that relugolix may cause infertility in males.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., P-gp inhibitors or combined P-gp and strong CYP3A inducers) and OTC drugs and herbal supplements, as well as any concomitant illnesses.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
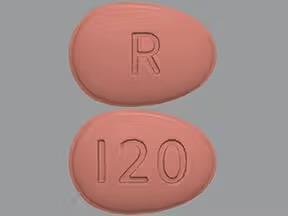
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
120 mg |
Orgovyx |
Sumitomo Pharma America |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about relugolix
- Check interactions
- Compare alternatives
- Reviews (24)
- Side effects
- Dosage information
- During pregnancy
- Drug class: gonadotropin-releasing hormone antagonists
- Breastfeeding
- En español