Prucalopride (Monograph)
Brand name: Motegrity
Drug class: Prokinetic Agents
Chemical name: 4-amino-5-chloro-N-[1-(3-methoxypropyl) piperidin-4-yl]-2,3-dihydro-1-benzofuran-7-carboxamide monobutanedioate
Molecular formula: C18H26ClN3O3•C4H6O4
CAS number: 179474-85-2
Introduction
Selective type 4 serotonin (5-HT4) receptor agonist; GI prokinetic agent.1 2 5 6 7 14
Uses for Prucalopride
Chronic Idiopathic Constipation
Symptomatic treatment of chronic idiopathic constipation.1 2 3 4 6 8 9 10
Prucalopride Dosage and Administration
Administration
Oral Administration
Administer orally once daily without regard to food.1
Dosage
Available as prucalopride succinate; dosage expressed in terms of prucalopride.1
Adults
Chronic Idiopathic Constipation
Oral
2 mg once daily.1
In clinical trials, 81% of patients (geriatric patients) receiving initial dosage of 1 mg daily required increase in dosage to 2 mg daily.1
Prescribing Limits
Adults
Chronic Idiopathic Constipation
Oral
Dosage of 4 mg daily provides no additional benefit over 2 mg daily.7 8
Special Populations
Hepatic Impairment
Hepatic impairment: No dosage adjustment required.1 7
Renal Impairment
Mild or moderate renal impairment (Clcr ≥30 mL/minute): No dosage adjustment required.1
Severe renal impairment (Clcr <30 mL/minute): Reduce dosage to 1 mg once daily.1
End-stage renal disease requiring dialysis: Avoid use.1 (See Special Populations under Pharmacokinetics.)
Geriatric Patients
Base dosage on renal function.1 (See Special Populations under Pharmacokinetics.)
Cautions for Prucalopride
Contraindications
-
Intestinal perforation or obstruction due to structural or functional disorder of the gut wall, obstructive ileus, or severe inflammatory conditions of the intestinal tract (e.g., Crohn's disease, ulcerative colitis, toxic megacolon/megarectum).1
-
Known hypersensitivity to prucalopride.1
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., dyspnea, rash, pruritus, urticaria, facial edema) reported.1
Suicidal Ideation and Behavior
Suicides, suicide attempts, and suicidal ideation reported in clinical studies; however, causal relationship to prucalopride not established.1 Monitor for persistent worsening of depression and for emergence of suicidal thoughts and behaviors.1 (See Advice to Patients.)
Cardiovascular Safety
Although certain nonselective 5-HT4 receptor agonists (i.e., cisapride, tegaserod) have been associated with adverse cardiovascular events,5 12 a retrospective, observational, population-based cohort study revealed no increase in the risk of major adverse cardiovascular events (i.e., MI, stroke, cardiovascular death) in patients receiving prucalopride, a selective 5-HT4 receptor agonist.1 11 (See Actions.)
In double-blind clinical trials, the incidence of major adverse cardiovascular events was 3.5 per 1000 patient-years of prucalopride exposure versus 5.2 per 1000 patient-years of placebo exposure.1
No clinically important QT-interval prolongation observed in healthy individuals at doses of 5 times the recommended dose.1 13
Specific Populations
Pregnancy
Data insufficient to determine whether there is a drug-associated risk for spontaneous abortion, major birth defects, or adverse maternal or fetal outcomes with prucalopride use in pregnant women.1
No evidence of embryofetal developmental toxicity in animal studies.1
Lactation
Distributed into milk.1 During weaning, mean infant exposure estimated to be 1.74 mcg/kg daily (about 6% of the maternal dose) adjusted for body weight.1 (See Distribution under Pharmacokinetics.) No data on effects on the breast-fed child or on milk production.1
Consider benefits of breast-feeding and importance of prucalopride to the woman; also consider potential adverse effects on the breast-fed child from the drug or underlying maternal condition.1
Pediatric Use
Safety and efficacy not established in pediatric patients.1
Geriatric Use
No overall differences in efficacy and safety in patients ≥65 years of age relative to younger adults.1
Exposure may be increased, but this effect appears to be related to decreased renal function.1 Adjust dosage based on renal function.1 (See Renal Impairment under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Hepatic Impairment
Exposure to prucalopride not substantially altered.1
Renal Impairment
Eliminated mainly by the kidneys; mean AUC increased in patients with renal impairment.1 Risk of adverse effects may be increased.1
Reduce dosage in patients with severe renal impairment.1 Avoid use in patients with end-stage renal disease requiring dialysis.1 (See Renal Impairment under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Common Adverse Effects
Headache,1 2 3 4 6 8 9 abdominal pain,1 2 4 6 9 nausea,1 2 3 4 6 8 9 diarrhea,1 2 3 4 6 8 9 abdominal distension,1 dizziness,1 3 vomiting,1 8 flatulence,1 fatigue.1
Drug Interactions
Substrate of CYP3A4,1 P-glycoprotein (P-gp),7 and breast cancer resistance protein (BCRP) in vitro.7
Low potential to inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4 or to induce CYP isoenzymes 1A2, 2B6, and 3A4 at clinically relevant concentrations.1
Low potential to inhibit P-gp, BCRP, organic anion transport protein (OATP) 1B1 or 1B3, organic anion transporter (OAT) 1 or 3, organic cation transporter (OCT) 1 or 2, multidrug and toxin extrusion (MATE) 1 or 2-K transporters, bile salt export pump (BSEP), or multidrug resistance protein (MRP) 2 at clinically relevant concentrations.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cimetidine |
No clinically important effect on pharmacokinetics of prucalopride1 7 |
|
|
Digoxin |
No clinically important effect on pharmacokinetics of digoxin1 7 |
|
|
Erythromycin |
No clinically important effect on pharmacokinetics of prucalopride; 1 peak concentration and AUC of erythromycin increased by 40 and 28%, respectively1 7 |
Interaction unlikely to be clinically important1 |
|
Estrogens and progestins |
Oral contraceptive containing ethinyl estradiol and norethisterone: No clinically important effect on pharmacokinetics of the estrogen or progestin1 |
|
|
Ketoconazole |
Peak concentration and AUC of prucalopride increased by approximately 40%1 |
Interaction unlikely to be clinically important1 |
|
Paroxetine |
No clinically important effect on pharmacokinetics of either drug1 7 |
|
|
Probenecid |
No clinically important effect on pharmacokinetics of prucalopride1 7 |
|
|
Warfarin |
No clinically important effect on pharmacokinetics of warfarin1 7 |
Prucalopride Pharmacokinetics
Absorption
Bioavailability
Following oral administration, bioavailability is >90%; peak plasma concentrations are achieved within 2–3 hours.1
Pharmacokinetics are dose proportional and time independent.1
Food
High-fat meal does not affect oral bioavailability.1
Distribution
Extent
Distributed into milk.1 Milk-to-plasma ratio during weaning was 2.65:1; concentration during weaning may not reflect concentration during full milk production.1
Plasma Protein Binding
Elimination
Metabolism
Seven minor metabolites identified; however, parent drug accounts for 92–94% of plasma exposure.1 Most common metabolite (O-desmethylprucalopride acid) accounts for only 3.2 or 3.1% of an oral dose recovered in urine or feces, respectively.1
Elimination Route
Eliminated mainly by the kidneys by passive filtration and active secretion and to a lesser extent (≤35%) by nonrenal mechanisms.1
Approximately 84.2% of an oral dose excreted in urine (60–65% of the dose excreted in urine as unchanged drug) and 13.3% excreted in feces (5% of the dose excreted in feces as unchanged drug).1
Half-life
Special Populations
Moderate or severe hepatic impairment (Child-Pugh class B or C): Peak plasma concentration and AUC increased by 10–20%; not considered clinically important.1
Mild, moderate, or severe renal impairment (Clcr 60–89, 30–59, or 15–29 mL/minute, respectively): AUC increased by 1.23-, 1.4-, or 2.38-fold, respectively.1 Pharmacokinetics in patients with end-stage renal disease or undergoing dialysis not fully known.1
Geriatric patients: Peak plasma concentration and AUC increased by 26–28%.1 Effect of age appears to be related to decreased renal function.1
Sex, race, and body weight do not appear to affect pharmacokinetics of prucalopride.1
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).1 Keep in original container; protect from moisture.1
Actions
-
Selective 5-HT4 receptor agonist;1 2 5 6 7 14 increases bowel motility by binding with high affinity to 5-HT4 receptors, facilitating release of acetylcholine to enhance the amplitude of contractions and stimulate colonic peristalsis.1 7 14
-
In animal studies, induced contractions starting from the proximal colon to the anal sphincter.1 7
-
In patients with chronic idiopathic constipation, the number of high-amplitude propagating contractions increased during the first 12 hours after dosing; with once-daily administration, mean colonic transit time was reduced by 12 hours from a baseline of 65 hours.1
-
Devoid of effects mediated via type 2A, 2B, or 3 serotonin (5-HT2A, 5-HT2B, or 5-HT3), motilin, or cholecystokinin A receptors in vitro at concentrations exceeding the 5-HT4 receptor affinity by ≥150-fold.1 5 7 12 14
-
In animal studies, no clinically relevant effects on cardiovascular and cardiac electrophysiologic parameters observed at concentrations ≥50 times the therapeutic peak plasma concentration in humans.1 5
-
Certain nonselective 5-HT4 receptor agonists (i.e., cisapride, tegaserod) have been associated with adverse cardiovascular events; cardiac arrhythmias associated with cisapride use attributed to the drug's lack of selectivity for the 5-HT4 receptor (i.e., affinity for human ether-a-go-go gene [hERG]-encoded cardiac potassium channel), but precise mechanism by which tegaserod use may be associated with ischemic cardiovascular events not fully established.5 12 14 (See Cardiovascular Safety under Cautions.)
Advice to Patients
-
Advise patients to read manufacturer’s patient information.1
-
Advise patients and their caregivers and families that suicidal thoughts and behavior have been reported in patients receiving prucalopride.1 Importance of being alert for persistent worsening of symptoms of depression, unusual changes in mood or behavior, and emergence of suicidal thoughts or behavior.1 Importance of immediately discontinuing prucalopride and contacting a clinician if such symptoms occur.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of patients informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
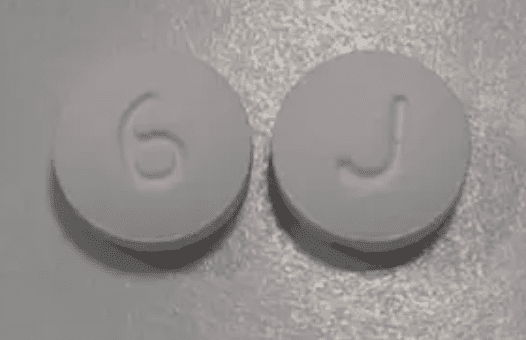
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
1 mg (of prucalopride) |
Motegrity |
Shire |
|
2 mg (of prucalopride) |
Motegrity |
Shire |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 28, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Shire. Motegrity (prucalopride succinate) tablets prescribing information. Lexington, MA; 2018 Dec.
2. Camilleri M, Piessevaux H, Yiannakou Y et al. Efficacy and Safety of Prucalopride in Chronic Constipation: An Integrated Analysis of Six Randomized, Controlled Clinical Trials. Dig Dis Sci. 2016; 61:2357-72. https://pubmed.ncbi.nlm.nih.gov/27056037
3. Yiannakou Y, Piessevaux H, Bouchoucha M et al. A randomized, double-blind, placebo-controlled, phase 3 trial to evaluate the efficacy, safety, and tolerability of prucalopride in men with chronic constipation. Am J Gastroenterol. 2015; 110:741-8. https://pubmed.ncbi.nlm.nih.gov/25869393
4. Piessevaux H, Corazziari E, Rey E et al. A randomized, double-blind, placebo-controlled trial to evaluate the efficacy, safety, and tolerability of long-term treatment with prucalopride. Neurogastroenterol Motil. 2015; 27:805-15. https://pubmed.ncbi.nlm.nih.gov/25808103
5. Conlon K, De Maeyer JH, Bruce C et al. Nonclinical Cardiovascular Studies of Prucalopride, a Highly Selective 5-Hydroxytryptamine 4 Receptor Agonist. J Pharmacol Exp Ther. 2018; 364:156-169. https://pubmed.ncbi.nlm.nih.gov/29180358
6. Quigley EM, Vandeplassche L, Kerstens R et al. Clinical trial: the efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation--a 12-week, randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2009; 29:315-28. https://pubmed.ncbi.nlm.nih.gov/19035970
7. US Food and Drug Administration. Center for Drug Evaluation and Research. Application number 210166Orig1s000. Multi-discipline review. From FDA website. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2018/210166Orig1s000MultidisciplineR.pdf
8. Camilleri M, Kerstens R, Rykx A et al. A placebo-controlled trial of prucalopride for severe chronic constipation. N Engl J Med. 2008; 358:2344-54. https://pubmed.ncbi.nlm.nih.gov/18509121
9. Ke M, Zou D, Yuan Y et al. Prucalopride in the treatment of chronic constipation in patients from the Asia-Pacific region: a randomized, double-blind, placebo-controlled study. Neurogastroenterol Motil. 2012; 24:999-e541. https://pubmed.ncbi.nlm.nih.gov/22882724
10. Tack J, van Outryve M, Beyens G et al. Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Gut. 2009; 58:357-65. https://pubmed.ncbi.nlm.nih.gov/18987031
11. Gilsenan A, Fortuny J, Cainzos-Achirica M et al. Cardiovascular Safety of Prucalopride in Patients with Chronic Constipation: A Multinational Population-Based Cohort Study. Drug Saf. 2019; https://pubmed.ncbi.nlm.nih.gov/31134512
12. Tack J, Camilleri M, Chang L et al. Systematic review: cardiovascular safety profile of 5-HT(4) agonists developed for gastrointestinal disorders. Aliment Pharmacol Ther. 2012; 35:745-67. https://pubmed.ncbi.nlm.nih.gov/22356640
13. Mendzelevski B, Ausma J, Chanter DO et al. Assessment of the cardiac safety of prucalopride in healthy volunteers: a randomized, double-blind, placebo- and positive-controlled thorough QT study. Br J Clin Pharmacol. 2012; 73:203-9. https://pubmed.ncbi.nlm.nih.gov/21848574
14. Omer A, Quigley EMM. An update on prucalopride in the treatment of chronic constipation. Therap Adv Gastroenterol. 2017; 10:877-887. https://pubmed.ncbi.nlm.nih.gov/29147138
Related/similar drugs
Frequently asked questions
More about prucalopride
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (105)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: serotoninergic neuroenteric modulators
- Breastfeeding
- En español