Dapagliflozin Propanediol (Monograph)
Brand name: Farxiga
Drug class: Sodium-glucose Cotransporter 2 (SGLT2) Inhibitors
Introduction
Antidiabetic agent; sodium-glucose cotransporter 2 (SGLT2) inhibitor.
Uses for Dapagliflozin Propanediol
Type 2 Diabetes Mellitus
Glycemic Control
Used as an adjunct to diet and exercise to improve glycemic control in adults and pediatric patients ≥10 years of age with type 2 diabetes mellitus.
In adults, evaluated as monotherapy or in combination with other antidiabetic agents (e.g., metformin, sulfonylurea, thiazolidinedione, dipeptidyl peptidase-4 [DPP-4] inhibitor, glucagon-like peptide 1 [GLP-1] receptor agonist, insulin).
In pediatric patients, evaluated as add-on therapy to metformin and/or insulin.
Commercially available as a single-entity preparation and in fixed combination with extended-release metformin (Xigduo XR) or saxagliptin (Qtern). Dapagliflozin/metformin is indicated for use in adults and pediatric patients ≥10 years of age with type 2 diabetes mellitus, and dapagliflozin/saxagliptin is indicated for use in adults with type 2 diabetes mellitus.
Guidelines from the American Diabetes Association (ADA) and other experts generally recommend the use of SGLT2 inhibitors or glucagon-like peptide 1 receptor agonists in patients with type 2 diabetes and established/high risk of atherosclerotic cardiovascular disease (ASCVD), heart failure, and/or chronic kidney disease. When selecting treatment regimen, consider factors such as cardiovascular and renal comorbidities, drug efficacy and adverse effects, hypoglycemic risk, presence of overweight or obesity, cost, access, and patient preferences. Weight management should be included as a distinct treatment goal and other healthy lifestyle behaviors should also be included in treatment plan.
Not indicated for treatment of type 1 diabetes mellitus.
Not indicated to improve glycemic control in type 2 diabetes mellitus in patients with eGFR <45 mL/minute per 1.73 m2.
Reduction in Heart Failure-related Hospitalization
Used to reduce the risk of hospitalization for heart failure in patients with type 2 diabetes mellitus and established cardiovascular disease or multiple cardiovascular risk factors.
For the treatment of patients with type 2 diabetes mellitus and established ASCVD (or high risk of ASCVD), current clinical practice guidelines generally recommend the use of an SGLT2 inhibitor with proven efficacy in cardiovascular outcome trials.
Beneficial Effects on Renal Function
Beneficial effects on renal function have been observed in patients with type 2 diabetes mellitus and chronic kidney disease (CKD).
For the treatment of patients with type 2 diabetes mellitus and CKD, current clinical practice guidelines generally recommend the use of an SGLT2 inhibitor with proven benefit in reducing adverse renal outcomes.
Heart Failure
Used to reduce the risk of cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in adults with heart failure.
Beneficial effects of dapagliflozin demonstrated in patients with chronic heart failure with or without coexisting type 2 diabetes mellitus.
Current expert guidelines on heart failure recommend guideline-directed medical therapy with a combination of the following drugs to reduce morbidity and mortality: angiotensin-converting enzyme (ACE) inhibitors, SGLT2 inhibitors, angiotensin II receptor antagonists, angiotensin receptor-neprilysin inhibitors (ARNIs), β-adrenergic blocking agents, and mineralocorticoid receptor antagonists. SGLT2 inhibitors are recommended in all patients with heart failure (either reduced ejection fraction or preserved ejection fraction), irrespective of the presence of type 2 diabetes in the absence of contraindications.
Chronic Kidney Disease
Used to reduce the risk of sustained decline in eGFR, end-stage kidney disease, cardiovascular death, and hospitalization for heart failure in adults with chronic kidney disease at risk of progression.
Beneficial effects of dapagliflozin demonstrated in patients with and without coexisting type 2 diabetes mellitus.
Dapagliflozin Propanediol Dosage and Administration
General
Pretreatment Screening
-
Assess renal function prior to initiation.
-
Assess volume status prior to initiation; volume depletion should be corrected prior to initiation.
Patient Monitoring
-
Assess renal function as clinically indicated.
-
Monitor for signs and symptoms of urinary tract infections and genital mycotic infections.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) includes Farxiga (dapagliflozin) and Fetzima (levomilnacipran) on the ISMP List of Confused Drug Names, and recommends using special safeguards to ensure the accuracy of prescriptions for these drugs.
Other General Considerations
-
Hold dapagliflozin therapy for at least 3 days, if possible, prior to major surgery or procedures requiring prolonged fasting. Resume therapy once the patient is clinically stable and has resumed oral intake.
Administration
Oral Administration
Dapagliflozin: Administer once daily in the morning, with or without food.
Fixed combination of dapagliflozin and extended-release metformin: Administer once daily in the morning with food to reduce the adverse GI effects of the metformin component.
Fixed combination of dapagliflozin and saxagliptin: Administer once daily in the morning, with or without food.
See full prescribing information for additional information on administration of the combination products.
If a dose of dapagliflozin is missed, take missed dose as soon as it is remembered followed by resumption of regular schedule. If missed dose is not remembered until the time of the next dose, skip missed dose and resume regular schedule. Do not double dose to replace a missed dose.
Dosage
Dosage of dapagliflozin propanediol is expressed in terms of dapagliflozin.
Pediatric Patients
Type 2 Diabetes Mellitus - Glycemic Control (Patients ≥10 Years of Age)
Dapagliflozin
OralInitially, 5 mg once daily.
May increase dosage to 10 mg once daily in patients who require additional glycemic control.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
OralInitial dosage based on patient's current regimen with dapagliflozin and/or metformin hydrochloride. May gradually increase dosage based on effectiveness and tolerability.
In patients currently not receiving dapagliflozin, initial recommended dosage of the dapagliflozin component is 5 mg once daily. Titrate gradually based on effectiveness and tolerability, up to maximum dosage of 10 mg of dapagliflozin and 2 g of extended-release metformin hydrochloride daily.
Patients who are already receiving extended-release metformin hydrochloride in the evening and are switching to the fixed combination of dapagliflozin and extended-release metformin should skip their last dose of metformin hydrochloride before initiating therapy with the fixed combination the following morning.
Adults
Type 2 Diabetes Mellitus - Glycemic Control
Dapagliflozin
OralInitially, 5 mg once daily.
May increase dosage to 10 mg once daily in patients who require additional glycemic control.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
OralInitial dosage based on patient's current regimen with dapagliflozin and/or metformin hydrochloride. May gradually increase dosage based on effectiveness and tolerability.
In patients currently not receiving dapagliflozin, initial recommended dosage of the dapagliflozin component is 5 mg once daily. Titrate gradually based on effectiveness and tolerability, up to a maximum dosage of 10 mg of dapagliflozin and 2 g of extended-release metformin hydrochloride daily.
Patients who are already receiving extended-release metformin hydrochloride in the evening and are switching to the fixed combination of dapagliflozin and extended-release metformin hydrochloride should skip their last dose of metformin hydrochloride before initiating therapy with the fixed combination the following morning.
Dapagliflozin/Saxagliptin Fixed-combination Therapy
OralRecommended initial dosage in patients not already receiving dapagliflozin therapy is 5 mg of dapagliflozin and 5 mg of saxagliptin once daily in the morning.
In patients requiring additional glycemic control and tolerating initial dosage, may increase dosage of fixed combination to 10 mg of dapagliflozin and 5 mg of saxagliptin once daily.
Do not use fixed combination in patients receiving concomitant therapy with a potent CYP3A4/5 inhibitor (e.g., atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin).
Heart Failure
Dapagliflozin
Oral10 mg once daily.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral10 mg of dapagliflozin once daily.
Chronic Kidney Disease
Dapagliflozin
Oral10 mg once daily.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral10 mg of dapagliflozin once daily.
Special Populations
Hepatic Impairment
Dapagliflozin
Oral
Mild, moderate, or severe hepatic impairment: No dosage adjustment necessary.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral
Avoid use in patients with hepatic impairment.
Dapagliflozin/Saxagliptin Fixed-combination Therapy
Oral
Mild, moderate, or severe hepatic impairment: No dosage adjustment necessary.
Renal Impairment
Dapagliflozin
Oral
Glycemic control: No dosage adjustment necessary for eGFR ≥45 mL/minute per 1.73 m2. Use not recommended if eGFR <45 mL/minute per 1.73 m2.
Reduction in risk of sustained eGFR decline, end stage kidney disease, cardiovascular death or heart failure-related hospitalization with or without type 2 diabetes mellitus: No dosage adjustment necessary for eGFR ≥25 mL/minute per 1.73 m2. If eGFR falls below 25 mL/minute per 1.73 m2, may be continued. Initiation not recommended if eGFR <25 mL/minute per 1.73 m2.
Dapagliflozin/Extended-release Metformin Hydrochloride Fixed-combination Therapy
Oral
Mild renal impairment (eGFR ≥45 mL/minute per 1.73 m2): No dosage adjustment necessary.
Moderate renal impairment: Not recommended if eGFR <45 mL/minute per 1.73 m2. Initiation not recommended if eGFR between 30–45 mL/minute per 1.73 m2. Assess benefit versus risk if eGFR falls persistently below this level.
Severe renal impairment (eGFR <30 mL/minute per 1.73 m2or hemodialysis): Contraindicated.
Dapagliflozin/Saxagliptin Fixed-combination Therapy
Oral
Mild renal impairment (eGFR ≥45 mL/minute per 1.73 m2): No dosage adjustment necessary.
Moderate or severe renal impairment: Contraindicated in patients with an eGFR <45 mL/minute per 1.73 m2.
Geriatric Patients
No dosage adjustment necessary based solely on age.
Cautions for Dapagliflozin Propanediol
Contraindications
-
History of serious hypersensitivity reaction to dapagliflozin. Serious hypersensitivity reactions, including anaphylaxis and angioedema, reported in patients receiving the drug.
Warnings/Precautions
Ketoacidosis
Ketoacidosis requiring hospitalization reported in patients with type 1 or type 2 diabetes mellitus receiving SGLT2 inhibitors; occurred in some cases without markedly elevated blood glucose concentrations (e.g., <250 mg/dL).
Consider monitoring ketones in patients with type 1 diabetes mellitus and other patients who may be at risk of ketoacidosis.
Evaluate for presence of ketoacidosis in patients experiencing signs and symptoms consistent with severe metabolic acidosis regardless of the patient's blood glucose concentration; discontinue dapagliflozin and initiate appropriate treatment if confirmed. Monitor patient for resolution prior to restarting the drug.
Prior to initiating dapagliflozin therapy, consider risk factors that may predispose patients to ketoacidosis (e.g., insulin deficiency, reduced caloric intake, acute febrile illness, ketogenic diet, surgery, volume depletion, alcohol abuse). Risk factors for development of ketoacidosis should be resolved prior to initiation.
Educate all patients on signs and symptoms of ketoacidosis and instruct them to discontinue dapagliflozin and seek medical attention immediately if signs and symptoms occur.
Withhold dapagliflozin therapy if possible in temporary clinical situations that may predispose patients to ketoacidosis; resume therapy once patient is clinically stable and able to resume oral intake. For patients who undergo surgery or procedures associated with prolonged fasting, withhold dapagliflozin therapy for at least 3 days if possible.
Some clinicians suggest monitoring of urine and/or plasma ketone levels if patients feel unwell, regardless of ambient glucose concentrations.
Volume Depletion
May cause intravascular volume depletion. Symptomatic hypotension or acute transient changes in serum creatinine can occur, particularly in patients with impaired renal function (eGFR <60 mL/minute per 1.73 m2), geriatric patients, or patients receiving loop diuretics.
Assess risk factors that may predispose to acute kidney injury (e.g., hypovolemia, chronic renal insufficiency, heart failure, concomitant medications) and correct intravascular volume status prior to initiating dapagliflozin in such patients.
Monitor patients for signs and symptoms of hypotension after initiating therapy.
Renal Effects
Causes intravascular volume contraction and can cause acute kidney injury.
May increase Scr concentration and decrease eGFR; geriatric patients and patients with impaired renal function may be more susceptible to these changes. Adverse reactions related to renal function can occur following initiation of the drug.
Prior to initiating dapagliflozin therapy, consider factors that may predispose patients to acute kidney injury, such as hypovolemia, chronic renal insufficiency, heart failure, and concomitant medications (e.g., diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIAs).
Consider temporarily discontinuing dapagliflozin in any setting of reduced oral intake (e.g., acute illness, fasting) or fluid losses (e.g., GI illness, excessive heat exposure).
Evaluate renal function prior to initiation of dapagliflozin and monitor periodically thereafter. Discontinue dapagliflozin and initiate appropriate treatment if kidney injury occurs.
Urosepsis and Pyelonephritis
May increase the risk of serious urinary tract infections (e.g., urosepsis, pyelonephritis requiring hospitalization).
Prior to initiating dapagliflozin therapy, consider patient factors that may predispose to serious urinary tract infections (e.g., history of difficulty urinating; infection of the bladder, kidneys, or urinary tract).
Monitor patients for signs and symptoms of urinary tract infections and initiate treatment promptly, if indicated.
Hypoglycemia with Concomitant Therapy with Insulin or Insulin Secretagogues
When adding dapagliflozin to therapy with an insulin secretagogue (e.g., a sulfonylurea) or insulin, incidence of hypoglycemia is increased. Consider reducing dosage of the concomitant insulin secretagogue or insulin to reduce the risk of hypoglycemia.
Necrotizing Fasciitis of the Perineum
Fournier gangrene (necrotizing fasciitis of the perineum), a rare but serious and life-threatening bacterial infection requiring urgent surgical intervention, reported during postmarketing surveillance of males and females with type 2 diabetes mellitus receiving an SGLT2 inhibitor.
Assess patient for necrotizing fasciitis if pain or tenderness, erythema, or swelling in the genital or perineal area occurs in addition to fever or malaise.
If Fournier gangrene suspected, discontinue dapagliflozin and initiate treatment immediately with broad-spectrum antibiotics and, if necessary, perform surgical debridement. Closely monitor blood glucose concentrations and initiate alternative antidiabetic therapy to maintain glycemic control.
Genital Mycotic Infections
Possible increased risk of genital mycotic infections in males (e.g., balanitis) and females (e.g., vulvovaginal mycotic infection). Patients with a history of genital mycotic infections were more likely to develop such infections.
Monitor patients for genital mycotic infections and institute appropriate treatment if these infections occur.
Use of Fixed Combinations
When dapagliflozin is used in fixed combination with metformin, saxagliptin, or other drugs, consider the cautions, precautions, contraindications, and interactions associated with the concomitant agent(s) in addition to those associated with dapagliflozin.
Laboratory Test Interference
SGLT2 inhibitors, including dapagliflozin, increase urinary glucose excretion and result in false-positive urine glucose tests. Manufacturer states that 1,5-anhydroglucitol assay unreliable for monitoring glycemic control in patients taking SGLT2 inhibitors. Alternate methods of monitoring glycemic control should be used.
Initiation of therapy may cause small increase in serum creatinine concentration and decreases in eGFR. In patients with normal or mildly impaired renal function, changes in serum creatinine and eGFR generally occur within weeks of initiation and then stabilize. Changes that do not fit this pattern should prompt further evaluation to exclude possibility of acute kidney injury. Acute effect on eGFR reverses after discontinuation, suggesting acute hemodynamic changes play role in changes in renal function.
Specific Populations
Pregnancy
Insufficient data to evaluate drug-associated risk of major birth defects or miscarriage.
Studies in animals indicate that dapagliflozin use during pregnancy may affect renal development and maturation.
Not recommended in pregnant women during the second and third trimesters of pregnancy.
Lactation
No data on presence of dapagliflozin in human milk, effects on breast-fed child, or effects on milk production. Distributed into milk in rats; not known whether distributed into human milk. Use of dapagliflozin in women who are breast-feeding not recommended.
Pediatric Use
Safety and efficacy in type 2 diabetes mellitus established in pediatric patients ≥10 years of age. Safety and efficacy similar to that observed in adults.
Safety and efficacy not established in pediatric patients for other indications.
Geriatric Use
Efficacy in patients with type 2 diabetes mellitus similar in patients <65 years of age and those ≥65 years of age after controlling for renal function (eGFR). Such geriatric patients more likely to experience hypotension.
Hepatic Impairment
Assess benefits versus risks of dapagliflozin or the fixed combination of dapagliflozin and saxagliptin in patients with severe hepatic impairment; safety and efficacy not established in such patients. Avoid use of the fixed-combination preparation containing dapagliflozin and extended-release metformin in patients with clinical or laboratory evidence of hepatic impairment.
Renal Impairment
Patients with an eGFR of 45 to <60 mL/minute per 1.73 m2 receiving dapagliflozin had substantial improvement in glycemic control and experienced adverse effects similar to those without renal impairment. Patients receiving dapagliflozin therapy had a greater reduction in eGFR compared with those receiving placebo; however, renal function generally increased back to baseline values after discontinuing treatment with dapagliflozin. Patients with renal impairment receiving dapagliflozin for glycemic control may be more likely to experience hypotension and may be at an increased risk for acute kidney injury. Patients with an eGFR of 30 to <60 mL/minute per 1.73 m2 receiving dapagliflozin had a greater incidence of bone fractures compared with those receiving placebo.
Assess renal function prior to initiation of therapy and periodically thereafter.
Common Adverse Effects
Dapagliflozin monotherapy (≥5%): Female genital mycotic infections, nasopharyngitis, urinary tract infections.
Dapagliflozin in combination with extended-release metformin hydrochloride (>5%): Female genital mycotic infections, nasopharyngitis, urinary tract infection, diarrhea, headache.
Dapagliflozin in combination with saxagliptin (≥5%): Upper respiratory tract infection, urinary tract infection, dyslipidemia.
Drug Interactions
Metabolism principally mediated by uridine diphosphate-glucuronosyltransferase (UGT) isoenzyme 1A9; minor CYP-mediated metabolism.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Did not inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4 in vitro. Did not induce CYP isoenzymes 1A2, 2B6, or 3A4 in vitro.
Drugs Affecting Efflux Transport Systems
Dapagliflozin 3-O-glucuronide, inactive metabolite of dapagliflozin, is a substrate of organic anion transport (OAT) 3. Dapagliflozin and dapagliflozin 3-O-glucuronide did not meaningfully inhibit OAT1 or OAT3 active transporters; pharmacokinetic interactions unlikely with OAT1 or OAT3 substrates.
Did not meaningfully inhibit organic cation transporter (OCT) 2; pharmacokinetic interactions unlikely with substrates of OCT2.
Weak P-glycoprotein substrate; did not meaningfully inhibit P-glycoprotein. Unlikely to affect pharmacokinetics of concurrently administered P-glycoprotein substrates.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Bumetanide |
Increased bumetanide AUC and peak plasma concentration |
No dosage adjustment necessary |
|
Digoxin |
No clinically meaningful effect on digoxin AUC or peak plasma concentration |
No adjustment of digoxin dosage necessary |
|
Diuretics |
Possible increased incidence of symptomatic hypotension |
Assess and correct intravascular volume prior to dapagliflozin initiation; monitor for signs and symptoms of hypotension after initiating therapy |
|
Glimepiride |
Increased glimepiride AUC |
No dosage adjustment necessary |
|
Hydrochlorothiazide |
No clinically important effect on pharmacokinetics of either drug |
No dosage adjustment necessary |
|
Insulin and Insulin Secretagogues |
Risk of hypoglycemia increased when used concomitantly with insulin secretagogue (e.g., sulfonylurea) or insulin |
Reduced dosage of insulin or insulin secretagogue may be required to reduce the risk of hypoglycemia |
|
Lithium |
May decrease lithium concentrations |
Monitor serum lithium concentrations more frequently during dapagliflozin initiation and dosage changes |
|
Mefenamic acid |
Increased dapagliflozin peak plasma concentration and AUC |
No adjustment of dapagliflozin dosage necessary |
|
Metformin |
No clinically meaningful effect on pharmacokinetics of either drug |
No dosage adjustment necessary |
|
Pioglitazone |
Decreased pioglitazone peak plasma concentration |
No dosage adjustment necessary |
|
Rifampin |
Decreased dapagliflozin peak plasma concentration and AUC |
No adjustment of dapagliflozin dosage necessary |
|
Simvastatin |
Increased simvastatin AUC |
No dosage adjustment necessary |
|
Sitagliptin |
No clinically meaningful effect on pharmacokinetics of either drug (single-dose administration) |
No dosage adjustment necessary |
|
Urine glucose tests (e.g., 1,5-anhydroglucitol assay) |
SGLT2 inhibitors increase urinary glucose excretion and will result in false-positive urine glucose tests; after discontinuation of dapagliflozin 10 mg, elevation in urinary glucose excretion approaches baseline in approximately 3 days |
Use alternative methods to monitor glycemic control |
|
Valsartan |
Decreased peak plasma concentrations of valsartan and dapagliflozin and increased valsartan AUC |
No dosage adjustment necessary |
|
Warfarin |
No clinically meaningful effect on warfarin pharmacokinetics or pharmacodynamics |
No warfarin dosage adjustment necessary |
Dapagliflozin Propanediol Pharmacokinetics
Absorption
Bioavailability
Absolute oral bioavailability: 78%.
Peak plasma concentration usually attained within 2 hours after oral dosing in fasted state.
Food
Administration with a high-fat meal decreased peak plasma concentration by up to 50% and prolonged time to peak plasma concentration by approximately 1 hour, but did not alter AUC; not considered clinically meaningful.
Special Populations
Mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment: No clinically important differences in peak plasma concentration or AUC.
Severe hepatic impairment (Child-Pugh class C): AUC and peak plasma concentration increased by 67 and 40%, respectively, compared with individuals with normal hepatic function following a single 10-mg dose of dapagliflozin.
Mild renal impairment: Geometric mean systemic exposure at steady state increased by 45% compared with individuals with normal renal function.
Moderate renal impairment: Geometric mean systemic exposure at steady state increased 2.04-fold compared with individuals with normal renal function.
Severe renal impairment: Geometric mean systemic exposure at steady state increased 3.03-fold compared with individuals with normal renal function.
Distribution
Extent
Extensively distributed.
Plasma Protein Binding
Approximately 91%.
Special Populations
Renal or hepatic impairment does not meaningfully alter plasma protein binding.
Elimination
Metabolism
Metabolized principally by UGT1A9 to inactive metabolites; CYP-mediated metabolism is a minor clearance pathway.
Elimination Route
75 and 21% of total radioactivity excreted in urine and feces, respectively, with <2% and approximately 15% in urine and feces, respectively, as parent drug.
Half-life
Approximately 12.9 hours following a single oral dose of 10 mg.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted to 15–30°C).
Actions
-
Inhibits SGLT2, a transporter expressed in proximal renal tubules and responsible for majority of reabsorption of filtered glucose from the tubular lumen.
-
Reduces reabsorption of filtered glucose and lowers the renal threshold for glucose in a dose-dependent manner, leading to increased urinary glucose excretion.
-
Increases glucose excretion independent of insulin secretion.
-
Improves muscle insulin sensitivity; however, glucosuria induction appears to increase endogenous glucose production.
-
Endogenous glucose production increases, accompanied by an increase in fasting plasma glucagon concentration.
-
Reduces sodium reabsorption and increases delivery of sodium to distal renal tubule. These actions may influence several physiological functions, including lowering pre- and afterload of the heart and downregulation of sympathetic activity, and decreased intraglomerular pressure, which is thought to be mediated by increased tubuloglomerular feedback.
Advice to Patients
-
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Medication Guide). Importance of patient reading medication guide before initiating therapy and each time the drug is dispensed.
-
When dapagliflozin is used in fixed combination with other drugs, advise the patient on important cautionary information about the concomitant agents.
-
Advise patients on the potential risks and benefits of dapagliflozin and of alternative therapies.
-
Advise patients on the importance of not using dapagliflozin in type 1 diabetes mellitus or diabetic ketoacidosis.
-
Inform patients that ketoacidosis, which can be a life-threatening condition, has been reported with dapagliflozin therapy (sometimes associated with illness or surgery among other risk factors). Advise patients of the signs and symptoms of ketoacidosis (e.g., tachypnea or hyperventilation, anorexia, abdominal pain, nausea, vomiting, lethargy, mental status change) and instruct them to discontinue dapagliflozin and seek medical advice immediately should they experience any such signs or symptoms. Advise patients to use a ketone dipstick to check for ketones in their urine (when possible) if symptoms of ketoacidosis occur, even if blood glucose is not elevated (e.g., <250 mg/dL).
-
Inform patients that symptomatic hypotension may occur with dapagliflozin and advise patients to report such symptoms to their clinicians. Inform patients that dapagliflozin-induced dehydration may increase the risk of hypotension and changes in kidney function and that patients should maintain adequate fluid intake.
-
Inform patients that the incidence of hypoglycemia may increase when dapagliflozin is added to an insulin secretagogue (e.g., sulfonylurea) or insulin. Educate patients on the signs and symptoms of hypoglycemia.
-
Inform patients that acute kidney injury has been reported with dapagliflozin therapy. Advise patients to seek medical attention immediately if they experience decreased urine output or swelling of the legs or feet. Advise patients to seek medical advice immediately if they have reduced oral intake (such as due to acute illness or fasting) or increased fluid losses (such as due to vomiting, diarrhea, or excessive heat exposure), as it may be appropriate to temporarily discontinue dapagliflozin in those settings.
-
Inform patients that necrotizing infections of the perineum (Fournier gangrene) have occurred with SGLT2 inhibitor therapy. Advise patients to promptly seek medical attention if they develop pain or tenderness, redness, or swelling of the genitals or the area from the genitals back to the rectum, in addition to fever (>38°C) or malaise.
-
Inform patients that yeast infection may occur (e.g., vulvovaginitis, balanitis, balanoposthitis). Inform female patients of the signs and symptoms of vaginal yeast infections (e.g., vaginal discharge, odor, itching) and male patients of the signs and symptoms of balanitis or balanoposthitis (e.g., rash or redness of the glans or foreskin of the penis). Advise patients of treatment options and when to seek medical advice.
-
Inform patients of the potential for urinary tract infections, which may be serious, with dapagliflozin therapy. Advise patients of the signs and symptoms of urinary tract infection and the need to contact a clinician promptly if such signs and symptoms occur.
-
Inform patients that due to the mechanism of action of dapagliflozin, patients taking the drug will test positive for glucose in their urine. Inform patients that urine glucose tests should not be used to monitor glycemic status while taking dapagliflozin.
-
Advise patients of the risk of serious hypersensitivity reactions, such as urticaria, anaphylactic reactions, and angioedema, with dapagliflozin therapy. If signs or symptoms of such a reaction occur, inform patients of the importance of discontinuing dapagliflozin and immediately informing a clinician.
-
Inform patients about the importance of adherence to dietary instructions, regular physical activity, periodic blood glucose monitoring and glycosylated hemoglobin (hemoglobin A1c; HbA1c) testing, recognition and management of hypoglycemia and hyperglycemia, and assessment of diabetes complications.
-
Importance of promptly seeking medical advice during periods of stress such as fever, trauma, infection, or surgery as medication requirements may change.
-
Inform patients of the importance of taking dapagliflozin exactly as directed by clinician.
-
Advise women to inform their clinicians immediately if they are or plan to become pregnant or plan to breast-feed. Advise women that breastfeeding is not recommended while taking dapagliflozin.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., severe kidney disease).
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
5 mg (of dapagliflozin)* |
Dapagliflozin Tablets |
|
|
Farxiga |
AstraZeneca |
|||
|
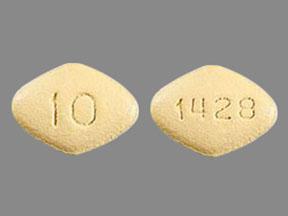
10 mg (of dapagliflozin)* |
Dapagliflozin Tablets |
|||
|
Farxiga |
AstraZeneca |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release |
2.5 mg (of dapagliflozin) with Extended-release Metformin Hydrochloride 1 g |
Xigduo XR |
AstraZeneca |
|
5 mg (of dapagliflozin) with Extended-release Metformin Hydrochloride 500 mg |
Xigduo XR |
AstraZeneca |
||
|
5 mg (of dapagliflozin) with Extended-release Metformin Hydrochloride 1 g* |
Dapagliflozin and Extended-release Metformin Tablets |
|||
|
Xigduo XR |
AstraZeneca |
|||
|
10 mg (of dapagliflozin) with Extended-release Metformin Hydrochloride 500 mg |
Xigduo XR |
AstraZeneca |
||
|
10 mg (of dapagliflozin) with Extended-release Metformin Hydrochloride 1 g* |
Dapagliflozin and Extended-release Metformin Hydrochloride Tablets |
|||
|
Xigduo XR |
AstraZeneca |
|||
|
Tablets, film-coated |
5 mg (of dapagliflozin) with Saxagliptin 5 mg |
Qtern |
AstraZeneca |
|
|
10 mg (of dapagliflozin) with Saxagliptin 5 mg |
Qtern |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Trulicity
Trulicity is an injectable diabetes medicine that is used together with diet and exercise to ...
Lantus
Lantus is a long acting form of insulin used to treat type 1 or type 2 diabetes. Learn about side ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Tresiba
Tresiba (insulin degludec) is used to treat diabetes mellitus. Includes Tresiba side effects ...
Levemir
Levemir (insulin detemir) is a long acting insulin used to treat diabetes in adults and children ...
Victoza
Victoza helps control blood sugar levels and reduce the risk of serious heart problems in people ...
Novolog
NovoLog is a fast-acting insulin used to treat diabetes to control blood sugar levels in adults and ...
Basaglar
Basaglar (insulin glargine) is a long-acting insulin that is used to improve blood sugar control in ...
Soliqua
Soliqua 100/33 (insulin glargine and lixisenatide) is used to treat type 2 diabetes. Includes ...
Toujeo SoloStar
Toujeo (insulin glargine) is an injection used to treat type 1 or type 2 diabetes. Includes Toujeo ...
Frequently asked questions
More about dapagliflozin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (199)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: SGLT-2 inhibitors
- Breastfeeding
- En español