Ethambutol (Monograph)
Brand name: Myambutol
Drug class: Antituberculosis Agents
- Antimycobacterial Agents
VA class: AM500
CAS number: 1070-11-7
Introduction
Antituberculosis agent.103 106 a
Uses for Ethambutol
Tuberculosis
Treatment of active (clinical) tuberculosis (TB) in conjunction with other antituberculosis agents.103 c d e
First-line agent for treatment of pulmonary TB; used in the initial intensive treatment phase.106
First-line agent for management of drug-resistant pulmonary TB.106
For initial treatment of active TB caused by drug-susceptible M. tuberculosis, recommended multiple-drug regimens consist of an initial intensive phase (2 months) and a continuation phase (4 or 7 months).106 109 Although the usual duration of treatment for drug-susceptible pulmonary and extrapulmonary TB (except disseminated infections and TB meningitis) is 6–9 months,106 109 ATS, CDC, and IDSA state that completion of treatment is determined more accurately by the total number of doses and should not be based solely on the duration of therapy.106 A longer duration of treatment (e.g., 12–24 months) usually is necessary for infections caused by drug-resistant M. tuberculosis.106 109
Patients with treatment failure or drug-resistant M. tuberculosis, including multidrug-resistant (MDR) TB (resistant to both isoniazid and rifampin) or extensively drug-resistant (XDR) TB (resistant to both isoniazid and rifampin and also resistant to a fluoroquinolone and at least one parenteral second-line antimycobacterial such as capreomycin, kanamycin, or amikacin), should be referred to or managed in consultation with experts in the treatment of TB as identified by local or state health departments or CDC.106
Mycobacterium avium Complex (MAC) Infections
Treatment of M. avium complex (MAC) infections† [off-label] in conjunction with other antimycobacterials, including infections in HIV-infected adults, adolescents, or children† [off-label].107 c d
For initial treatment of nodular/bronchiectatic pulmonary disease caused by macrolide-susceptible MAC, ATS and IDSA recommend a 3-times weekly regimen of clarithromycin (or azithromycin), ethambutol, and rifampin in most patients.107 For initial treatment of fibrocavitary or severe nodular/bronchiectatic pulmonary disease caused by macrolide-susceptible MAC, ATS and IDSA recommend a daily regimen of clarithromycin (or azithromycin), ethambutol, and rifampin (or rifabutin) and state that consideration can be given to adding amikacin or streptomycin during the first 2–3 months of treatment for extensive (especially fibrocavitary) disease or when previous therapy has failed.107 Although a 2-drug regimen of clarithromycin (or azithromycin) and ethambutol may be adequate for treatment of nodular/bronchiectatic MAC disease in some patients, such regimens should not be used for fibrocavitary disease because of the risk of emergence of macrolide resistance.107
For treatment of disseminated MAC disease, including in HIV-infected individuals, ATS, CDC, NIH, and IDSA recommend a regimen of clarithromycin (or azithromycin) and ethambutol with or without rifabutin.107 c d
Treatment of MAC infections is complicated and should be directed by clinicians familiar with mycobacterial diseases; consultation with a specialist is particularly important when the patient cannot tolerate first-line drugs or when the infection has not responded to prior therapy or is caused by macrolide-resistant MAC.107
Prevention of recurrence (secondary prophylaxis) of disseminated MAC infections† [off-label] in HIV-infected adults, adolescents, and children† [off-label].108 c d USPHS/IDSA, CDC, NIH, IDSA, and others recommend clarithromycin (or azithromycin) given with ethambutol (with or without rifabutin) for secondary prophylaxis after the initial infection has been treated.108 c
Not used for primary prevention (primary prophylaxis) of disseminated MAC infection in HIV-infected individuals.108 Drug of choice for primary prophylaxis is azithromycin or clarithromycin;107 108 rifabutin (with or without azithromycin) is an alternative.107 108
Mycobacterium kansasii and Other Mycobacterial Infections
Treatment of M. kansasii† [off-label] infections in conjunction with other antimycobacterials.107 g ATS and IDSA recommend a regimen of isoniazid, rifampin, and ethambutol for treatment of pulmonary or disseminated infections caused by rifampin-susceptible M. kansasii.107 If rifampin-resistant M. kansasii are involved, ATS and IDSA recommend a 3-drug regimen based on results of in vitro susceptibility, including clarithromycin (or azithromycin), moxifloxacin, ethambutol, sulfamethoxazole, or streptomycin.107
Treatment of M. marinum† infections in conjunction with other antimycobacterials (e.g., clarithromycin and/or rifampin).107 i j l Optimum regimens not identified.107 i j l Monotherapy (minocycline, clarithromycin, doxycycline, co-trimoxazole) may be effective for superficial cutaneous infections,j but a multiple-drug regimen usually used for severe cutaneous infections or infections in immunocompromised individuals.i j
Treatment of M. xenopi† infections in conjunction with other antimycobacterials.107 Optimum regimens not established; in vivo response may not correlate with in vitro susceptibility.107 ATS and IDSA state that a regimen of clarithromycin, rifampin, and ethambutol generally has been used, although rate of relapse is high.107 A regimen of isoniazid, rifampin (or rifabutin), ethambutol, and clarithromycin (with or without streptomycin during initial treatment) also has been suggested.107
Ethambutol Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.103 e
Dosage
Available as ethambutol hydrochloride; dosage expressed in terms of the salt.103 e
Must be used in conjunction with other antimycobacterial agents for treatment of active (clinical) TB,103 108 e treatment or prevention of MAC infections†,107 108 c or treatment of other mycobacterial infections†.107
Can be used in daily or intermittent (e.g., 2 or 3 times weekly) multiple-drug TB regimens.106 109 c d
Pediatric Patients
Tuberculosis
Treatment of Active (Clinical) Tuberculosis in Children†
OralChildren <15 years of age or weighing ≤40 kg†: 15–25 mg/kg once daily recommended by ATS, CDC, IDSA, AAP, and others.106 109 d h If an intermittent regimen is used, 50 mg/kg twice weekly.106 109 d h ATS, CDC, and IDSA recommend that children receive a maximum of 1 g per dose;106 d AAP and others recommend a maximum of 2.5 g per dose.109 h
Treatment of Active (Clinical) Tuberculosis in Adolescents
OralAdolescents ≥15 years of age weighing 40–55 kg: 800 mg daily, 2 g twice weekly, or 1.2 g 3 times weekly recommended by ATS, CDC, and IDSA.106
Adolescents ≥15 years of age weighing 56–75 kg: 1.2 g daily, 2.8 g twice weekly, or 2 g 3 times weekly recommended by ATS, CDC, and IDSA.106
Adolescents ≥15 years of age weighing 76-90 kg: 1.6 g daily, 4 g twice weekly, or 2.4 g 3 times weekly recommended by ATS, CDC, and IDSA.106
Adolescents: AAP and others recommend 15–25 mg/kg (up to 2.5 g) once daily or 50 mg/kg twice weekly (up to 2.5 g per dose).109 h
Mycobacterium avium Complex (MAC) Infections†
Treatment of Disseminated MAC in HIV-infected Children†
Oral15–25 mg/kg (up to 1 g) once daily.d h Used in conjunction with clarithromycin (7.5–15 mg/kg [up to 500 mg] twice daily) or azithromycin (10–12 mg/kg [up to 500 mg] once daily) with or without rifabutin (10–20 mg/kg [up to 300 mg] once daily).d
Treatment of Disseminated MAC in HIV-infected Adolescents†
Oral15 mg/kg once daily in conjunction with either clarithromycin (500 mg twice daily) or azithromycin (500 mg once daily) with or without rifabutin (300 mg once daily).107 c
Prevention of MAC Recurrence (Secondary Prophylaxis) in HIV-infected Children†
Oral15 mg/kg (up to 900 mg) once daily.108 h Used in conjunction with clarithromycin (7.5 mg/kg [up to 500 mg] twice daily) or azithromycin (5 mg/kg [up to 250 mg] once daily) with or without rifabutin (5 mg/kg [up to 300 mg] once daily).108
Secondary prophylaxis to prevent MAC recurrence in HIV-infected children usually continued for life.108 The safety of discontinuing secondary MAC prophylaxis in children whose CD4+ T-cell count increases in response to antiretroviral therapy has not been studied.108
Prevention of MAC Recurrence (Secondary Prophylaxis) in HIV-infected Adolescents†
Oral15 mg/kg (up to 900 mg) once daily.108 c h Used in conjunction with either clarithromycin (500 mg twice daily) or azithromycin (500 mg once daily) with or without rifabutin (300 mg once daily).108 c
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adolescents.108 c
Consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 that has been sustained for ≥6 months.108 c Reinitiate prophylaxis if CD4+ T-cell count decreases to <100/mm3.108 c
Adults
Tuberculosis
Treatment of Active (Clinical) Tuberculosis
OralManufacturers recommend 15 mg/kg once daily in previously untreated adults.103 e In previously treated adults, manufacturers recommend 25 mg/kg once daily for 60 days, followed by 15 mg/kg once daily.103 e
Adults weighing 40–55 kg: 800 mg once daily, 2 g twice weekly, or 1.2 g 3 times weekly recommended by ATS, CDC, and IDSA.106 c
Adults weighing 56–75 kg: 1.2 g once daily, 2.8 g twice weekly, or 2 g 3 times weekly recommended by ATS, CDC, and IDSA.106 c
Adults weighing 76-90 kg: 1.6 g once daily, 4 g twice weekly, or 2.4 g 3 times weekly recommended by ATS, CDC, and IDSA.106 c
Mycobacterium avium Complex (MAC) Infections†
Initial Treatment of Pulmonary MAC Infections (Nodular/bronchiectatic Disease) Caused by Macrolide-susceptible Strains†
Oral25 mg/kg 3 times weekly in conjunction with rifampin (600 mg 3 times weekly) and either clarithromycin (1 g 3 times weekly) or azithromycin (500 mg 3 times weekly) recommended by ATS and IDSA.107 Continue until patient has been culture negative on treatment for 1 year.107
Intermittent (3-times weekly) regimen is not recommended for those with cavitary or moderate or severe disease or those who have been previously treated.107
Initial Treatment of Pulmonary MAC Infections (Fibrocavitary or Severe Nodular/bronchiectatic Disease) Caused by Macrolide-susceptible Strains†
Oral15 mg/kg once daily in conjunction with either rifampin (10 mg/kg [up to 600 mg] once daily) or rifabutin (150–300 mg once daily) and either clarithromycin (0.5–1 g daily) or azithromycin (250 mg once daily) recommended by ATS and IDSA.107 Continue until patient has been culture negative on treatment for 1 year.107 Consideration can be given to including amikacin or streptomycin 3-times weekly during the first 2–3 months of treatment for extensive, especially fibrocavitary, disease or when previous therapy has failed.107
Treatment of Disseminated MAC in HIV-infected and Other Adults†
Oral15 mg/kg once daily in conjunction with either clarithromycin (500 mg twice daily) or azithromycin (500 mg once daily) with or without rifabutin (300 mg once daily) recommended by ATS, CDC, and IDSA.107 c
Prevention of MAC Recurrence (Secondary Prophylaxis) in HIV-infected Adults†
Oral15 mg/kg once daily.108 c Used in conjunction with either clarithromycin (500 mg twice daily) or azithromycin (500 mg once daily) with or without rifabutin (300 mg once daily).108 c
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adults.108
Consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 that has been sustained for ≥6 months.108 c Reinitiate prophylaxis if CD4+ T-cell count decreases to <100/mm3.108 c
Mycobacterium kansasii and Other Mycobacterial Infections†
Treatment of Pulmonary or Disseminated Infections Caused by Rifampin-susceptible M. kansasii†
Oral15 mg/kg once daily in conjunction with rifampin (10 mg/kg [up to 600 mg] daily), isoniazid (5 mg/kg [up to 300 mg] daily), and pyridoxine (50 mg daily) recommended by ATS and IDSA.107
Continue until patient has been culture negative on treatment for 1 year.107 A longer duration may be needed in HIV-infected individuals with disseminated infections.107
Treatment of M. marinum Infections†
Oral15–25 mg/kg daily in conjunction with rifampin (600 mg daily) and/or clarithromycin.107 i j l
Optimal duration of treatment not known; continue for 3–6 months or until at least 1–2 months after resolution of symptoms.107 i j l
Prescribing Limits
Pediatric Patients
Tuberculosis
Treatment of Active (Clinical) Tuberculosis in Children†
OralMaximum 1 g per dose recommended by ATS, CDC, and IDSA for once-daily or twice-weekly regimens;106 d maximum 2.5 g per dose recommended by AAP and others for once-daily or twice-weekly regimens.109 h
Mycobacterium avium Complex (MAC) Infections in Children†
Oral
Maximum 1 g once daily for treatment of disseminated MAC infections.d Maximum 900 mg once daily for prevention of MAC recurrence (secondary prophylaxis).108
Special Populations
Renal Impairment
Reduce dosage based on degree of renal impairment and serum concentrations of the drug.103 106 c e h
Some experts recommend 15 mg/kg once every 24–36 hours in adults with Clcr 10–50 mL/minute, 15 mg/kg once every 48 hours in those with Clcr <10 mL/minute, and 15 mg/kg 3 times weekly (after hemodialysis) in those undergoing hemodialysis.c Others recommend 15–20 mg/kg 3 times weekly (after dialysis) in adults with end-state renal disease (Clcr <30 mL/minute, on hemodialysis).106
In children with renal impairment, some experts recommend that the usual dose be given once every 24 hours in those with Clcr >50 mL/minute or once every 24–36 hours in those with Clcr 10–50 mL/minute.h In children with Clcr <10 mL/minute, these experts recommend that a decreased dose be given once every 48 hours.h Supplemental doses are recommended after hemodialysis.h
Cautions for Ethambutol
Contraindications
-
Known hypersensitivity to ethambutol or any ingredient in the formulation.103 e
-
Optic neuritis, unless clinical judgment deems it necessary to use the drug.103 e
-
Patients unable to appreciate and report visual adverse effects or changes in vision (e.g., young children, unconscious patients).103 (See Pediatric Use under Cautions.)
Warnings/Precautions
Warnings
Ocular Effects
Decreased visual acuity, constriction of visual fields, central and peripheral scotomas, and loss of red-green color discrimination reported.103 106 a e May be due to optic neuritis, but has occurred in the absence of a diagnosis of optic or retrobulbar neuritis.103 e May be related to dose and duration of treatment.103 106 e
Perform ophthalmic evaluation (ophthalmoscopy, finger perimetry, test for color discrimination) at baseline and periodically during treatment.103 106 e Test each eye separately and together since change in visual acuity may be unilateral or bilateral.103 e Evaluate monthly in patients receiving >15 mg/kg daily, in those receiving the drug for >2 months, and in those with renal impairment.103 106 e
Use with caution in patients with ocular defects (e.g., cataracts, recurrent ocular inflammatory conditions, optic neuritis, diabetic retinopathy) that make visual changes difficult to detect or evaluate; weigh benefits versus possible visual deterioration in these patients.103 e
Discontinue if substantial changes in visual acuity occur.103 e Changes in visual acuity usually reversible (over several weeks or months), but irreversible blindness has been reported.103 e
Hepatic Effects
Liver toxicities, including fatalities, have been reported.103
Perform baseline and periodic assessment of hepatic function.103 e
Sensitivity Reactions
Anaphylactoid reactions, dermatitis, pruritus reported.103
General Precautions
Precautions Related to Treatment of Tuberculosis
Should not be used alone for the treatment of active TB; must be given in conjunction with other antituberculosis agents.106
Clinical specimens for microscopic examination and mycobacterial cultures and in vitro susceptibility testing should be obtained prior to initiation of antituberculosis therapy and periodically during treatment to monitor therapeutic response.106 The antituberculosis regimen should be modified as needed.106 Patients with positive cultures after 4 months of treatment should be considered to have failed treatment (usually as the result of noncompliance or drug-resistant TB).106
Compliance with the full course of antituberculosis therapy and all drugs included in the multiple-drug regimen is critical.106 Missed doses increase the risk of treatment failure and increase the risk that M. tuberculosis will develop resistance to the antituberculosis regimen.106
To ensure compliance, ATS, CDC, IDSA, and AAP recommend that directly observed (supervised) therapy (DOT) be used for treatment of active (clinical) TB whenever possible, especially when intermittent regimens are used, when the patient is immunocompromised or infected with HIV, or when drug-resistant M. tuberculosis is involved.106 109 c d
Laboratory Monitoring
Assess organ system function (e.g., renal, hepatic, hematopoietic) at baseline and periodically during treatment.103 e
Specific Populations
Pregnancy
Category C.103
Ophthalmic abnormalities have been reported in infants born to women who received antituberculosis regimens that included ethambutol during pregnancy.103
The ATS, CDC, IDSA, AAP and others consider ethambutol safe for use in pregnant women;106 108 109 AAP states potential benefits outweigh the risks to the infant.109
Lactation
Distributed into milk; use only if possible benefits outweigh potential risks.103
AAP considers ethambutol compatible with breast-feeding.b
Pediatric Use
Safety not established in children <13 years of age; manufacturers do not recommend use in this age group.103 e Has been used in pediatric patients without unusual adverse effects.d
ATS, CDC, IDSA, and AAP state that ethambutol can be used safety in older children, but should be used with caution in children in whom it may be difficult to monitor visual acuity (e.g., <5 years of age).106 109 If used in pediatric patients, perform ophthalmic evaluations once monthly during treatment.d
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity in this age group cannot be ruled out.103
Hepatic Impairment
ATS, CDC, and IDSA state that ethambutol can be used safely in patients with hepatic disease.106
Renal Impairment
Use with caution; dosage reduction based on serum concentrations is advised.103 e Closely monitor visual acuity and color discrimination (i.e., monthly).103 106 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Ophthalmic effects (decreased visual acuity, scotoma, color blindness, visual defect), joint pain, GI effects (anorexia, nausea, vomiting, GI upset, abdominal pain), fever, malaise, headache, dizziness, mental confusion.103 e
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Aluminum-containing antacids: Decreased ethambutol serum concentrations and urinary excretion; possible decreased oral absorption of the antimycobacterial103 |
Administer aluminum-containing antacids ≥4 hours after ethambutol103 |
|
Rifabutin |
Pharmacokinetic interaction unlikelyf |
Ethambutol Pharmacokinetics
Absorption
Bioavailability
75–80% of an oral dose is absorbed from the GI tract;a peak plasma concentrations achieved within 2–4 hours.103 e
Food
Food does not appear to affect absorption.103 e
Special Populations
Serum concentrations are higher in patients with renal impairment.a
Distribution
Extent
Widely distributed into most body tissues and fluids.a Highest concentrations are found in erythrocytes, kidneys, lungs, and saliva; lower drug concentrations are found in ascitic fluid, pleural fluid, brain, and CSF.a
Crosses the placenta and is distributed into cord blood and amniotic fluid.100
Distributed into milk.103
Plasma Protein Binding
8–22%.a
Elimination
Metabolism
Undergoes oxidation in the liver to an aldehyde intermediate which is converted to a dicarboxylic acid derivative.103 e
Elimination Route
Excreted in urine as unchanged drug (50%) and metabolites (8–15%) and in feces as unchanged drug (20–22%).103 e
Removed by peritoneal dialysis and to a lesser extent by hemodialysis.a
Half-life
3.3 hours.a
Special Populations
Half-life prolonged in patients with impaired renal or hepatic function.a Half-life may be ≥7 hours in patients with renal failure.a
Stability
Storage
Oral
Tablets
15–30°Ce or 20–25°C103 , depending on the manufacturer. Protect from light and moisture.e
Actions and Spectrum
-
Bacteriostatic in action.a
-
Appears to inhibit the synthesis of one or more metabolites in susceptible bacteria resulting in impairment of cellular metabolism, arrest of multiplication, and cell death.103 e
-
A highly specific agent; active only against Mycobacterium.103 a Active against M. tuberculosis,a M. avium complex (MAC),a M. bovis,a M. kansasii,107 a g and some strains of M. fortuitum.a Although M. marinum may be susceptible,107 a resistance has been reported.k Active in vitro against M. gordonae,107 M. malmoense,107 and M. smegmatis.107 Has limited activity against M. genavense.107 M. haemophilum107 and some strains of M. xenopi are resistant.107
-
Natural and acquired resistance to ethambutol demonstrated in vitro and in vivo in strains of M. tuberculosis.103 a
-
No evidence of cross-resistance with other currently available antimycobacterials.103 e
Advice to Patients
-
Advise patients that poor compliance with antituberculosis regimens can result in treatment failure and development of drug-resistant TB, which can be life-threatening and lead to other serious health risks.106
-
Importance of completing full course of therapy; importance of not missing any doses.103
-
Importance of promptly informing clinicians of any change in visual acuity.103 e
-
Importance of informing clinicians of existing or contemplated therapy, including prescription and OTC drugs, as well as any concomitant illnesses.103
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.103
-
Importance of informing patients of other important precautionary information.103 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
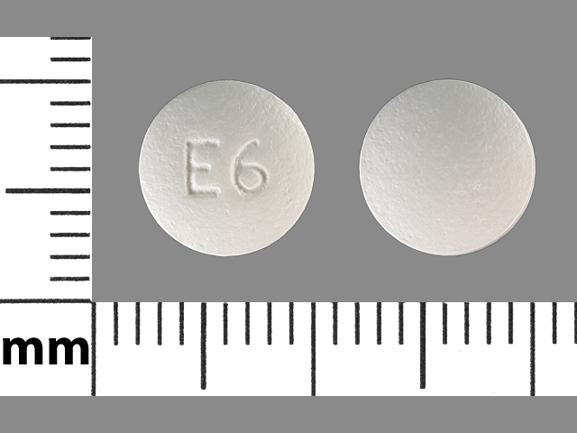
Oral |
Tablets, film-coated |
100 mg |
Ethambutol Tablets |
VersaPharm |
|
Myambutol |
X-Gen |
|||
|
400 mg |
Ethambutol Tablets |
Barr |
||
|
Myambutol (scored) |
X-Gen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 1, 2008. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
100. Holdiness MR. Transplacental pharmacokinetics of the antituberculosis drugs. Clin Pharmacokinet. 1987; 13:125-9. https://pubmed.ncbi.nlm.nih.gov/3304771
102. Brock PG, Roach M. Antituberculosis drugs during pregnancy. Lancet. 1981; 1:102.
103. X-Gen. Myambutol (ethambutol hydrochloride) tablets USP prescribing information. Northport, NY; 2004 Jun.
104. Gulliford M, Mackay AD, Prowse K. Cholestatic jaundice caused by ethambutol. BMJ. 1986; 292:866. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1339973/ https://pubmed.ncbi.nlm.nih.gov/3083914
105. US Centers for Disease Control and Prevention. Initial therapy for tuberculosis in the era of multidrug resistance. Recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1993; 42(RR-7):1-8. https://www.cdc.gov/mmwr/PDF/rr/rr4207.pdf
106. Centers for Disease Control and Prevention. Treatment of tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR Recomm Rep. 2003; 52(No. RR-11):1-77. https://www.cdc.gov/mmwr/PDF/rr/rr5211.pdf
107. Griffith DE, Aksamit T, Brown-Elliott BA et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367-416. https://pubmed.ncbi.nlm.nih.gov/17277290
108. US Public Health Service (USPHS) and Infectious Diseases Society of America (IDSA) Prevention of Opportunistic Infections Working Group. 2001 USPHS/IDSA guidelines for the prevention of opportunistic infections in persons with human immunodeficiency virus. From the US Department of Health and Human Services HIV/AIDS Information Services (AIDSinfo) website http://aidsinfo.nih.gov
109. American Academy of Pediatrics. 2006 Red Book: Report of the Committee on Infectious Diseases. 27th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2006.
a. AHFS drug information 2007. McEvoy GK. Ethambutol. Bethesda, MD. American Society of Health-System Pharmacists;2007:550-2.
b. Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation. 6th ed. Philadelphia; PA: Lippincott Wiliams & Wilkins; 2002:509-10.
c. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Recomm Rep. 2004; 53(RR-15):1-112. https://www.cdc.gov/mmwr/PDF/rr/rr5315.pdf
d. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-exposed and infected children: recommendations from CDC, the National Institutes of Health, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2004; 53(RR-14):1-92. https://www.cdc.gov/mmwr/PDF/rr/rr5314.pdf
e. VersaPharm. Ethambutol hydrochloride tablets USP prescribing information. Marietta, GA; 2001 Feb.
f. Pfizer. Mycobutin (rifabutin) capsules USP prescribing information. New York, NY; 2006 Feb.
g. Shitrit D, Baum GL, Priess R et al. Pulmonary Mycobacterium kansasii infection in Israel, 1999-2004: clinical features, drug susceptibility, and outcome. Chest. 2006; 129:771-6. https://pubmed.ncbi.nlm.nih.gov/16537880
h. Robertson J, Shilkofski N, eds. The Harriet Lane handbook: a manual for pediatric house officers. 17th ed. Philadelphia, PA: Elsevier Mosby: 2005:808-9,1058.
i. Lewis FM, Marsh BJ, von Reyn CF. Fish tank exposure and cutaneous infections due to Mycobacterium marinum: tuberculin skin testing, treatment, and prevention. Clin Infect Dis. 2003; 37:390-7. https://pubmed.ncbi.nlm.nih.gov/12884164
j. Rallis E, Koumantaki-Mathioudaki E. Treatment of Mycobacterium marinum cutaneous infections. Exp Opin Pharmacother. 2007; 8:2965-78.
k. Aubry A, Jarlier V, Escolano S et al. Antibiotic susceptibility pattern of Mycobacterium marinum. Antimicrob Agents Chemother. 2000; 44:3133-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC101616/ https://pubmed.ncbi.nlm.nih.gov/11036036
l. Edelstein H. Mycobacterium marinum skin infections. Report of 31 cases and review of the literature. Arch Intern Med. 1994; 154:1359-64. https://pubmed.ncbi.nlm.nih.gov/8002687
Related/similar drugs
More about ethambutol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antituberculosis agents
- Breastfeeding
- En español