Ethambutol Dosage
Medically reviewed by Drugs.com. Last updated on Apr 14, 2025.
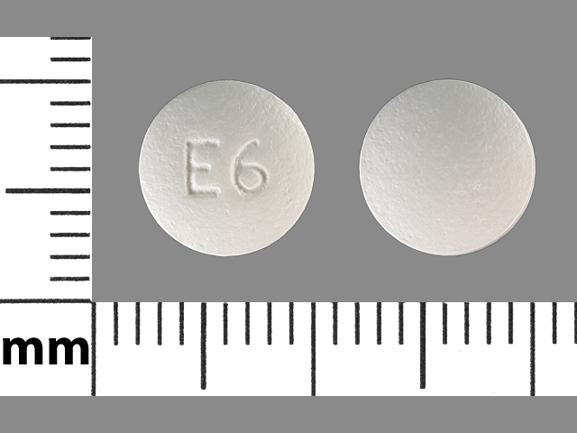
Applies to the following strengths: 100 mg; 400 mg
Usual Adult Dose for:
- Tuberculosis - Active
- Mycobacterium avium-intracellulare - Treatment
- Mycobacterium avium-intracellulare - Prophylaxis
- Mycobacterium kansasii
Usual Pediatric Dose for:
- Tuberculosis - Active
- Mycobacterium avium-intracellulare - Treatment
- Mycobacterium avium-intracellulare - Prophylaxis
Additional dosage information:
Usual Adult Dose for Tuberculosis - Active
Patients without previous antituberculous treatment (Initial treatment): 15 mg/kg orally once a day
Patients with previous antituberculous treatment (Retreatment):
Initial dose: 25 mg/kg orally once a day for 60 days
Maintenance dose: 15 mg/kg orally once a day
Comments:
- This drug should be used with at least 1 other antituberculosis agent (e.g., aminosalicylic acid, cycloserine, ethionamide, isoniazid, pyrazinamide, streptomycin, viomycin). Retreatment should include at least 1 of the susceptible second line drugs not previously administered to the patient.
- Treatment should be continued until bacteriological conversion has become permanent and maximal clinical improvement has occurred.
Use: Treatment of pulmonary tuberculosis
US Department of Health and Human Services (US HHS), National Institutes of Health (NIH), Health Resources and Services Administration (HRSA), and US Centers for Disease Control and Prevention (US CDC) Recommendations:
DRUG-SUSCEPTIBLE TUBERCULOSIS:
Initial Phase: 15 to 25 mg/kg orally once a day PLUS isoniazid, rifampin/rifabutin, and pyrazinamide
- Duration of therapy: 2 months
DRUG-RESISTANT TUBERCULOSIS:
Initial phase: 15 to 25 mg/kg orally once a day PLUS moxifloxacin/levofloxacin, rifampin/rifabutin, and pyrazinamide
- Duration of therapy: 2 months
Continuation phase: 15 to 25 mg/kg orally once a day PLUS moxifloxacin/levofloxacin, and rifampin/rifabutin
- Duration of therapy: 7 months
Weight-based dosing recommendations:
Patients 40 to 55 kg: 800 mg orally once a day
- Patients 56 to 75 kg: 1200 mg orally once a day
- Patients 76 to 90 kg: 1600 mg orally once a day
- Patients greater than 90 kg: 1600 mg/day
Use: First-line drug for the treatment of Mycobacterium tuberculosis
Infectious Diseases Society of America (IDSA), US CDC, and American Thoracic Society (ATS) Recommendations:
Daily dosing:
Infectious Diseases Society of America (IDSA), US CDC, and American Thoracic Society (ATS) Recommendations:
Daily dosing:
- Patients 40 to 55 kg: 800 mg orally once a day
- Patients 56 to 75 kg: 1200 mg orally once a day
- Patients 76 to 90 kg: 1600 mg orally once a day
2 times a week dosing recommendations:
- Patients 40 to 55 kg: 2000 mg orally 2 times a week
- Patients 56 to 75 kg: 2800 mg orally 2 times a week
- Patients 76 to 90 kg: 4000 mg orally 2 times a week
3 times a week dosing recommendations:
- Patients 40 to 55 kg: 1200 mg orally 3 times a week
- Patients 56 to 75 kg: 2000 mg orally 3 times a week
- Patients 76 to 90 kg: 2400 mg orally 3 times a week
Use: First-line drug for the treatment of drug-susceptible tuberculosis
Usual Adult Dose for Mycobacterium avium-intracellulare - Treatment
US HHS, NIH, HRSA, and US CDC Recommendations:
15 mg/kg orally once a day PLUS clarithromycin
- Duration of therapy: 12 months
Comments:
- Treatment may be discontinued if there are no signs/symptoms of Mycobacterium avium complex (MAC) disease AND the patient has a sustained (greater than 6 months) CD4 count greater than 100 cells/microliter in response to antiretroviral therapy.
- This drug may be given with azithromycin in patients with interaction or intolerance that precludes the use of clarithromycin.
Uses:
- Initial treatment of MAC disease
- Secondary prophylaxis/chronic suppressive/maintenance therapy of disseminated MAC disease in HIV-infected patients
IDSA, US CDC, and ATS Recommendations:
Initial Therapy for Nodular/Bronchiectatic Disease (Intermittent Therapy): 25 mg/kg orally 3 times a week PLUS rifampin and clarithromycin/azithromycin
Initial Therapy for Cavitary Disease, Advanced/Severe OR Previously Treated Disease: 15 mg/kg orally once a day PLUS rifampin/rifabutin and clarithromycin/azithromycin
Comments:
- Patients with severe and extensive (multilobar) disease may require additional treatment with streptomycin or amikacin for the first 2 to 3 months.
- Some experts recommend beginning treatment with the macrolide first, then starting this drug at an attenuated dose, with gradual dose increases to the desired therapeutic level over 1 to 2 weeks.
Uses:
- Initial treatment regimen for patients with nodular/bronchiectatic MAC lung disease
- Initial regimen for fibrocavitary or severe nodular/bronchiectatic MAC lung disease
- Preferred treatment with clarithromycin and rifabutin of disseminated MAC disease in HIV-infected patients
- Alternative treatment (with azithromycin and rifabutin) of disseminated MAC disease in HIV-infected patients
Usual Adult Dose for Mycobacterium avium-intracellulare - Prophylaxis
US HHS, NIH, HRSA, and US CDC Recommendations:
15 mg/kg orally once a day PLUS clarithromycin
- Duration of therapy: 12 months
Comments:
- Treatment may be discontinued if there are no signs/symptoms of Mycobacterium avium complex (MAC) disease AND the patient has a sustained (greater than 6 months) CD4 count greater than 100 cells/microliter in response to antiretroviral therapy.
- This drug may be given with azithromycin in patients with interaction or intolerance that precludes the use of clarithromycin.
Uses:
- Initial treatment of MAC disease
- Secondary prophylaxis/chronic suppressive/maintenance therapy of disseminated MAC disease in HIV-infected patients
IDSA, US CDC, and ATS Recommendations:
Initial Therapy for Nodular/Bronchiectatic Disease (Intermittent Therapy): 25 mg/kg orally 3 times a week PLUS rifampin and clarithromycin/azithromycin
Initial Therapy for Cavitary Disease, Advanced/Severe OR Previously Treated Disease: 15 mg/kg orally once a day PLUS rifampin/rifabutin and clarithromycin/azithromycin
Comments:
- Patients with severe and extensive (multilobar) disease may require additional treatment with streptomycin or amikacin for the first 2 to 3 months.
- Some experts recommend beginning treatment with the macrolide first, then starting this drug at an attenuated dose, with gradual dose increases to the desired therapeutic level over 1 to 2 weeks.
Uses:
- Initial treatment regimen for patients with nodular/bronchiectatic MAC lung disease
- Initial regimen for fibrocavitary or severe nodular/bronchiectatic MAC lung disease
- Preferred treatment with clarithromycin and rifabutin of disseminated MAC disease in HIV-infected patients
- Alternative treatment (with azithromycin and rifabutin) of disseminated MAC disease in HIV-infected patients
Usual Adult Dose for Mycobacterium kansasii
IDSA, US CDC, and ATS Recommendations:
15 mg/kg orally once a day
Duration of therapy: 18 months
Comment: Patients should have at least 12 months of negative sputum cultures.
Use: Treatment of nontuberculous mycobacterial pulmonary disease caused by Mycobacterium kansasii
Usual Pediatric Dose for Tuberculosis - Active
13 years and older:
Patients without previous antituberculous treatment (Initial treatment): 15 mg/kg orally once a day
Patients with previous antituberculous treatment (Retreatment):
Initial dose: 25 mg/kg orally once a day for 60 days
Maintenance dose: 15 mg/kg orally once a day
Comments:
- This drug should be used with at least 1 other antituberculosis agent (e.g., aminosalicylic acid, cycloserine, ethionamide, isoniazid, pyrazinamide, streptomycin, viomycin). Retreatment should include at least 1 of the susceptible second line drugs not previously administered to the patient.
- Treatment should be continued until bacteriological conversion has become permanent and maximal clinical improvement has occurred.
Use: Treatment of pulmonary tuberculosis
US HHS, NIH, HRSA, and US CDC Recommendations:
DRUG-SUSCEPTIBLE TUBERCULOSIS:
Intensive phase: 15 to 25 mg/kg orally once a day PLUS isoniazid, rifampin, and pyrazinamide
Maximum dose: 2.5 grams/day
Duration of therapy: 2 months
DRUG-RESISTANT TUBERCULOSIS:
Initial phase: 15 to 25 mg/kg orally once a day PLUS moxifloxacin/levofloxacin, rifampin/rifabutin, and pyrazinamide
- Duration of therapy: 2 months
Continuation phase: 15 to 25 mg/kg orally once a day PLUS moxifloxacin/levofloxacin, and rifampin/rifabutin
- Duration of therapy: 7 months
Weight-based dosing recommendations:
Patients 40 to 55 kg: 800 mg orally once a day
- Patients 56 to 75 kg: 1200 mg orally once a day
- Patients 76 to 90 kg: 1600 mg orally once a day
- Patients greater than 90 kg: 1600 mg/day
Comment: Lymph node tuberculosis may be treated as minimal intrathoracic disease.
Uses:
- First-line drug for the treatment of intrathoracic tuberculosis caused by susceptible strains of M tuberculosis
- First-line drug for the treatment of drug-resistant M tuberculosis
American Academy of Pediatrics (AAP), IDSA, US CDC, and ATS Recommendations:
Infants, Children, and Adolescents: 15 to 25 mg/kg orally once a day OR 50 mg/kg orally 2 times a week
Maximum dose: 2.5 grams/dose
Duration of therapy: 2 months
Uses:
- First-line drug for the treatment of drug-susceptible tuberculosis
- Treatment of pulmonary and extrapulmonary M tuberculosis infection (except meningitis)
Usual Pediatric Dose for Mycobacterium avium-intracellulare - Treatment
US HHS, NIH, HRSA, and US CDC Recommendations:
15 to 25 mg/kg orally once a day PLUS clarithromycin
Maximum dose: 2.5 grams/day
Duration of therapy: At least 12 months
Comments:
- Treatment may be discontinued if there are no signs/symptoms of Mycobacterium avium complex (MAC) disease AND the patient has a sustained (greater than 6 months) CD4 count greater than 100 cells/microliter in response to antiretroviral therapy.
- This drug may be given with azithromycin in patients with interaction or intolerance that precludes the use of clarithromycin.
- Chronic suppressive therapy is recommended in patients following initial treatment.
Use: Initial treatment of MAC disease
Usual Pediatric Dose for Mycobacterium avium-intracellulare - Prophylaxis
US HHS, NIH, HRSA, and US CDC Recommendations:
Secondary Prophylaxis (Chronic Suppressive Therapy):
15 to 25 mg/kg orally once a day PLUS clarithromycin and/or rifabutin
Maximum dose: 2.5 grams
Secondary prophylaxis may be discontinued if the following are met:
- At least 6 months of combination antiretroviral therapy are completed
- At least 12 months of MAC treatment are completed
- Asymptomatic for signs/symptoms of MAC
- Aged 2 to less than 6 years with CD4 counts greater than 200 cells/mm3 for at least 6 consecutive months OR aged at least 6 years with CD4 counts greater than 100 cells/mm3 for at least 6 consecutive months
Comments:
- Rifabutin should be added to patients over 5 years of age.
- This drug may be taken without regard to food.
- Secondary prophylaxis should be restarted in patients 2 to 6 years with CD4 counts less than 200 cells/mm3 OR at least 6 years with CD4 counts less than 100 cells/mm3.
Uses:
- First choice (with clarithromycin) for chronic suppressive therapy in patients with prior MAC disease
- Alternative secondary prophylaxis with azithromycin in patients with prior MAC disease
Renal Dose Adjustments
Dose adjustment(s) may be required; however, no specific guidelines have been suggested. Caution recommended.
US HHS, NIH, HRSA, and US CDC Recommendations:
CrCl 10 to 50 mL/min: 15 to 25 mg/kg orally every 24 to 36 hours
CrCl less than 10 mL/min: 15 to 25 mg/kg orally every 48 hours
ATS, US CDC, and IDSA Recommendations:
Drug-susceptible Tuberculosis:
CrCl less than 30 mL/min: 15 to 25 mg/kg orally 3 times a week
Comment: Therapeutic drug monitoring should be considered to guide dosing.
Liver Dose Adjustments
Data not available
ATS, US CDC, and IDSA Recommendations:
Patients with liver disease:
Treatment without pyrazinamide: 15 to 25 mg/kg orally once a day PLUS isoniazid and rifampin
- Duration of therapy: 2 months, followed by 7 months of isoniazid and rifampin
Treatment without isoniazid: 15 to 25 mg/kg orally once a day PLUS rifampin, pyrazinamide, with/without a fluoroquinolone
- Duration of therapy: At least 6 months
Patients with severe, unstable liver disease:
15 to 25 mg/kg orally once a day PLUS moxifloxacin/levofloxacin, cycloserine, and a second-line injectable
- Duration of therapy: 18 to 24 months
Weight-based dosing recommendations:
Patients 40 to 55 kg: 800 mg orally once a day
- Patients 56 to 75 kg: 1200 mg orally once a day
- Patients 76 to 90 kg: 1600 mg orally once a day
- Patients greater than 90 kg: 1600 mg/day
Precautions
CONTRAINDICATIONS:
- Hypersensitivity to the active component or any of the ingredients
- Patients with known optic neuritis unless clinical judgment determines that it may be used
- Patients who are unable to appreciate and report visual side effects or changes in vision (e.g., young children, unconscious patients)
Safety and efficacy have not been established in patients younger than 13 years; this drug is not recommended for use in these patients.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
US HHS, NIH, HRSA, and US CDC Recommendations:
Hemodialysis: 15 to 25 mg/kg orally 3 times a week after hemodialysis
Comment: Therapeutic drug monitoring should be considered to guide dosing.
Other Comments
Administration advice:
- This drug may be given without regard to food.
- Oral liquid formulations may be prepared by crushing the appropriate number of tablet(s) and then mixing with water or apple juice.
- Aluminum hydroxide-containing products should be avoided for at least 4 hours following administration.
Storage requirements:
- Store in light-resistant containers.
General:
- This drug has been shown to treat primary tuberculosis and extrapulmonary forms of tuberculosis (e.g. military, tuberculous meningitis, bones and joints, genitourinary, skin, eye diseases).
Monitoring:
- Hepatic: Baseline and periodic assessments should be performed
- Hematologic: Baseline and periodic assessments should be perfumed
- Ocular: Monthly eye exams (including visual acuity and color vision), especially at doses of 25 mg/kg/day and/or with treatment longer than 2 months
- Renal: Baseline and periodic assessments should be performed
Patient advice:
- Inform patients that this drug may cause dizziness, disorientation, blurred vision, numbness, paresthesia, and/or somnolence, and they should avoid driving or operating machinery if these side effects occur.
- Patients should be told to promptly report any change in visual acuity.
- Advise patients to speak to their healthcare provider if they become pregnant, intend to become pregnant, or are breastfeeding.
More about ethambutol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- During pregnancy
- Drug class: miscellaneous antituberculosis agents
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.