clomiPRAMINE (Monograph)
Brand name: Anafranil
Drug class: Tricyclics and Other Norepinephrine-reuptake Inhibitors
VA class: CN601
Chemical name: 3-Chloro-10,11-dihydro-N,N-dimethyl -5H-dibenz[b,f]azepine-5-propanamine monohydrochloride
Molecular formula: C19H23ClN2•HCl
CAS number: 17321-77-6
Warning
- Suicidality
-
Antidepressants may increase risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need.d e Clomipramine is not approved for use in pediatric patients except patients with obsessive-compulsive disorder.1 (See Pediatric Use under Cautions.)
-
In pooled data analyses, risk of suicidality was not increased in adults >24 years of age and apparently was reduced in adults ≥65 years of age with antidepressant therapy compared with placebo.d e
-
Depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide.d e f
-
Appropriately monitor and closely observe all patients who are started on clomipramine therapy for clinical worsening, suicidality, or unusual changes in behavior; involve family members and/or caregivers in this process.d e f (See Worsening of Depression and Suicidality Risk under Cautions.)
Introduction
Tricyclic antidepressant (TCA);1 2 3 235 pharmacologic profile resembles that of other TCAs,235 238 SSRIs, and trazodone.2 3 4 212 213 214 220 221
Uses for clomiPRAMINE
Obsessive-Compulsive Disorder (OCD)
Among the drugs of choice for the management of OCD.69 289 293 296 297
Reduces but does not completely eliminate obsessions and compulsions.96 271 292 300
Panic Disorder
Has been used effectively for the management of panic disorder† [off-label] with or without agoraphobia† [off-label].2 3 4 104 105 106 107 108 109 110 116 347
Major Depressive Disorder
Has been used effectively for the management of major depressive disorder† [off-label].2 3 254 255 256 257 258 259 260 267 277 278 282 288
Despite comparable efficacy,2 3 255 256 257 258 260 277 282 283 the adverse effect profile (e.g., anticholinergic effects) of clomipramine may limit its usefulness relative to other antidepressants (e.g., TCAs, SSRIs).2 257 258 277 282 283 288 289
Effective antidepressant when obsessive manifestations accompany episode of major depressive disorder.288
Chronic Pain
Has been used for the management of chronic pain† [off-label] (e.g., central pain, idiopathic pain disorder, tension headache, diabetic peripheral neuropathy, cancer pain) alone or as adjunct to conventional analgesics.2 3 52 111 112 113 114 115 118 119 120 121 122 123 124 125 343 344
Cataplexy and Associated Narcolepsy
Has been used for the symptomatic management of cataplexy† [off-label] in a limited number of patients with cataplexy† and associated narcolepsy†.3 132 133 279
Autistic Disorder
Has been used for the management of repetitive and obsessive-compulsive behaviors and hyperactivity associated with autistic disorder†;134 135 141 285 286 does not treat core symptoms of autistic disorder.b
Trichotillomania
Has been used for the management of trichotillomania† (an urge to pull out one’s hair) in a limited number of patients with the disorder;3 136 137 138 139 relapse reported in some patients receiving long-term therapy.140
Onychophagia
Has been used for the management of severe onychophagia† (nail biting) without a history of OCD.142
Associated with relatively high dropout rate because of adverse effects and drug intolerance; not considered first-line therapy in most patients with onychophagia.142 341
Eating Disorders
Has been used for the management of anorexia nervosa† in a limited number of patients with the disorder.229 230 231
Initial therapeutic effects (e.g., improved eating behavior, weight gain) not sustained with long-term therapy (e.g., ≥8 weeks).229 230 231 234
Avoid use in underweight individuals and in those exhibiting suicidal ideation.288 341
Premature Ejaculation
Has been used for the management of premature ejaculation†.3 128 129 130 131
Premenstrual Syndrome
Has been used for the management of premenstrual syndrome†.261 262 263 264
clomiPRAMINE Dosage and Administration
General
-
Allow at least 2 weeks to elapse between discontinuance of therapy with an MAO inhibitor and initiation of clomipramine and vice versa.1 Also allow at least 5 weeks to elapse when switching from fluoxetine.1
-
Monitor for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustments.d e f (See Worsening of Depression and Suicidality Risk under Cautions.)
-
Sustained therapy may be required;2 4 33 78 80 81 82 148 341 use lowest effective dosage and monitor periodically for need for continued therapy.1 299
-
Avoid abrupt discontinuance of therapy.1 2 78 148 301 To avoid withdrawal reactions, taper dosage gradually (e.g., over a period of approximately 2 weeks).1 2 78 148 301
Panic Disorder†
-
Transient increase in the number and intensity of panic attacks may occur during initial therapy with the drug.4 104 105 106 288
Administration
Oral Administration
Administer orally; initially, in divided doses with meals to lessen adverse GI effects.1 After initial dosage titration, the total daily dose may be given once daily at bedtime1 2 4 271 to minimize adverse effects (e.g., sedation) during waking hours1 2 and enhance patient compliance.2
Also has been administered IM† or IV†, but a parenteral dosage form is not commercially available in the US.4 272
Dosage
Available as clomipramine hydrochloride; dosage is expressed in terms of the salt.1
Individualize dosage carefully according to individual requirements and response.1
Allow 2–3 weeks to elapse between any further dosage adjustments after the initial dosage titration period for achievement of steady-state plasma concentrations.1
Pediatric Patients
OCD
Oral
Children >10 years of age: initially, 25 mg daily.1 Gradually increase dosage, as tolerated, during the first 2 weeks of therapy up to a maximum of 3 mg/kg or 100 mg daily, whichever is lower.1 2 242 Titrate dosage carefully.1 If necessary, dosages may be increased gradually during the next several weeks up to a maximum of 3 mg/kg or 200 mg daily (whichever is lower).1 2 3 4 66 67
Optimum duration not established; 1 78 271 some clinicians recommend that therapy be continued in responding patients at the minimally effective dosage for at least 18 months before attempting to discontinue.1 271 299
Adults
OCD
Oral
Initially, 25 mg daily.1 Gradually increase dosage, as tolerated, during the first 2 weeks of therapy to approximately 100 mg daily.1 If necessary, dosages may be increased gradually during the next several weeks up to a maximum of 250 mg daily.1 2 3 4 66 67
Optimum duration not established; 1 78 271 some clinicians recommend that therapy be continued in responding patients at the minimally effective dosage for at least 18 months before attempting to discontinue.1 271 299
Panic Disorder†
Oral
Usual dosage: ≤50 mg daily (range: 12.5–150 mg daily);2 4 104 105 106 107 108 110 116 272 patients with agoraphobia may require higher dosage.4 104 105 106
Major Depressive Disorder†
Oral
100–250 mg daily.2 272 277 278 288
Chronic Pain†
Oral
100–250 mg daily.2 115 272 288
Cataplexy and Associated Narcolepsy†
Oral
25–200 mg daily.132 133 272 279
Prescribing Limits
Pediatric Patients
OCD
Oral
Maximum 3 mg/kg or 200 mg daily, whichever is lower.1 2 3 4 66 67
Adults
OCD
Oral
Maximum 250 mg daily.1 2 3 4 66 67
Panic Disorder†
Oral
Maximum 200 mg daily.2 4 104 105 106 107 108 110 116 272
Special Populations
Geriatric Patients
Manufacturer makes no specific recommendation for dosage adjustment1 41 240 but lower clomipramine hydrochloride dosages are recommended by some clinicians at least during initial therapy.2 4 272 282
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.1
Cautions for clomiPRAMINE
Contraindications
-
Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor.1 (See Specific Drugs under Interactions.)
-
During the acute recovery phase following MI.1
-
Known hypersensitivity to clomipramine or other TCAs.1
Warnings/Precautions
Warnings
Seizures
Risk of seizure; use with caution in patients with a history of seizures or other predisposing factors (e.g., brain damage of various etiology, alcoholism, concurrent use of other drugs that lower the seizure threshold).1
Risk may be dose related.1 (See Prescribing Limits under Dosage and Administration.)
Worsening of Depression and Suicidality Risk
Possible worsening of depression and/or emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior in both adult and pediatric patients, whether or not they are taking antidepressants; may persist until clinically important remission occurs.d e f g However, suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide.d e f
Appropriately monitor and closely observe patients receiving clomipramine for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments.d e f (See Boxed Warning and also see Pediatric Use under Cautions.)
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania may be precursors to emerging suicidality.e f Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if severe, abrupt in onset, or not part of patient’s presenting symptoms.d e f (See General under Dosage and Administration and also see Withdrawal Reactions under Cautions.)
Prescribe in smallest quantity consistent with good patient management to reduce risk of overdosage.1 e
Observe these precautions for patients with psychiatric (e.g., major depressive disorder, OCD) or nonpsychiatric disorders.e
Bipolar Disorder
May unmask bipolar disorder.e (See Activation of Mania or Hypomania under Cautions.) Clomipramine is not approved for use in treating bipolar depression.1
Screen for risk of bipolar disorder by obtaining detailed psychiatric history (e.g., family history of suicide, bipolar disorder, depression) prior to initiating therapy.e
General Precautions
Cardiovascular Effects
Modest orthostatic decreases in BP,1 193 modest tachycardia,1 and/or ECG abnormalities (e.g., VPCs, ST-T wave changes, intraventricular conduction abnormalities) reported; use with caution in patients with known cardiovascular disease.1
Titrate dosage carefully.1
Neuropsychiatric Effects
Variety of neuropsychiatric manifestations (e.g., delusions, hallucinations, psychotic episodes, confusion, paranoia) reported.1 3 155 156 238
May precipitate an acute psychotic episode in patients with unrecognized schizophrenia.1 3 155 156 295
Activation of Mania or Hypomania
Risk of activation of mania or hypomania in patients with affective disorder.1 3 155 156 295 (See Bipolar Disorder under Cautions.)
Anticholinergic Effects
Use with caution in patients for whom excess anticholinergic activity could be harmful (e.g., history of urinary retention, increased intraocular pressure, angle-closure glaucoma).1
Interactions
More than 30 cases of hyperthermia reported,1 most cases occurring in patients receiving clomipramine in combination with other drugs (e.g., antipsychotic agents).1 157 199 When clomipramine and an antipsychotic agent were used concomitantly, the cases sometimes were considered to be examples of neuroleptic malignant syndrome (NMS).1 157 199
Hepatic Effects
Potentially clinically important elevations (e.g., >3 times ULN) in serum ALT1 65 and AST1 concentrations;1 severe hepatic injury and/or death rarely reported.1
Possible cross hepatotoxicity (e.g., elevated values on hepatic function tests, abdominal pain) involving different TCAs including clomipramine.207 (See Hepatic Impairment under Cautions.)
Hematologic Effects
Bone marrow depression1 227 (e.g., leukopenia,1 agranulocytosis,1 3 162 164 165 166 thrombocytopenia,1 anemia,1 pancytopenia)1 3 163 rarely reported.1 227
Obtain leukocyte and differential blood cell counts if fever and sore throat occur during therapy.1
Sexual Dysfunction
Relatively high risk of sexual dysfunction1 3 180 (e.g., libido change,1 65 189 251 ejaculatory failure,1 65 180 188 251 impotence1 65 189 245 270 ) in male patients with OCD.1
Normal sexual functioning usually returns within a few days after discontinuing therapy.2 3 180
Weight Changes
Possible weight gain1 242 245 247 249 or weight loss.1
Withdrawal Reactions
Withdrawal reactions (e.g., dizziness, nausea, vomiting, headache, malaise, sleep disturbance, hyperthermia, sweating, irritability, seizures, worsening of psychiatric status) reported following abrupt discontinuance of therapy.1 2 78 148 301
To avoid withdrawal reactions, taper dosage gradually and monitor patients carefully.1 2 78 148 301
Electroconvulsive Therapy (ECT)
Possible increased ECT risks; limit to patients for whom concomitant use is essential.1
Elective Surgery
Discontinue therapy for as long as is clinically feasible prior to surgery and advise the anesthetist of such action.1
Thyroid Disease
Use with caution in hyperthyroid patients or patients receiving thyroid agents because of the possibility of cardiac toxicity.1 1
Adrenal Medulla Tumors
Use with caution in patients with tumors of the adrenal medulla, in whom hypertensive crises may be provoked.1
Specific Populations
Pregnancy
Category C.1
Possible withdrawal symptoms (e.g., jitteriness,1 71 152 158 tremor,1 71 153 154 seizures1 3 152 153 ) in neonates whose mothers received clomipramine throughout pregnancy;1 avoid use during late pregnancy whenever possible.153
Lactation
Distributed into milk;1 4 22 55 60 62 71 150 discontinue nursing or the drug.1 62 149 150 151
Pediatric Use
Safety and efficacy for OCD not established in children <10 years of age.1
Potential risks associated with long-term use (e.g., effects on growth, development, or maturation) not systematically evaluated in children and adolescents.1
Adverse effects in children and adolescents >10 years of age generally similar to those in adults.1
FDA warns that a greater risk of suicidal thinking or behavior (suicidality) occurred during first few months of antidepressant treatment (4%) compared with placebo (2%) in children and adolescents with major depressive disorder, OCD, or other psychiatric disorders based on pooled analyses of 24 short-term placebo-controlled trials of 9 antidepressant drugs (SSRIs and others).e However, a more recent meta-analysis of 27 placebo-controlled trials of 9 antidepressants (SSRIs and others) in patients <19 years of age with major depressive disorder, OCD, or non-OCD anxiety disorders suggests that the benefits of antidepressant therapy in treating these conditions may outweigh the risks of suicidal behavior or suicidal ideation.g No suicides occurred in these pediatric trials.e g
Carefully consider these findings when assessing potential benefits and risks of clomipramine in a child or adolescent for any clinical use.d e f g (See Worsening of Depression and Suicidality Risk under Cautions.)
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.1
In pooled data analyses, a reduced risk of suicidality was observed in adults ≥65 years of age with antidepressant therapy compared with placebo.d e (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Possible increased sensitivity to anticholinergic (e.g., dry mouth, constipation, vision disturbance), cardiovascular, orthostatic hypotension, and sedative effects of TCAs.h i j k
Hepatic Impairment
Use with caution in patients with clinically important hepatic disease; periodically monitor hepatic enzyme concentrations.1
Renal Impairment
Use with caution in patients with clinically important renal impairment.1
Common Adverse Effects
Adverse GI (e.g., dry mouth, constipation, nausea, dyspepsia, anorexia, increased appetite), nervous system (e.g., somnolence, tremor, dizziness, nervousness, fatigue, myoclonus), or genitourinary (e.g., changed libido, ejaculatory failure, impotence, micturition disorder) effects; sweating; weight gain; visual changes.1 2 35 65 242
Drug Interactions
Extensively metabolized in the liver by various CYP isoenzymes (e.g., CYP1A2,346 CYP2C,73 CYP2D6,72 73 CYP3A4).c
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP2D6 and/or 1A2: Potential pharmacokinetic interaction (increased plasma clomipramine concentrations).a Monitor plasma clomipramine concentrations whenever a CYP2D6 inhibitor is added or discontinued and adjust dosages as needed.a
Drugs Associated with Serotonin Syndrome
Potential pharmacologic (serotonin syndrome) interaction with serotonergic agents.1 175 302 303 Avoid such use whenever clinically possible.1 302 303
Drugs Affecting the Seizure Threshold
Use caution with concurrent administration of clomipramine and drugs (e.g., other antidepressants, antipsychotic agents) that lower the seizure threshold.1
Protein-bound Drugs
Potential for clomipramine to displace or to be displaced by other protein-bound drugs.1 Observe patients for adverse effects.1 2
Specific Drugs
|
Drug |
Interaction |
Comments |
|
Alcohol |
Potential for increased CNS effects of alcohol1 Limited data suggest that demethylation of clomipramine may be reduced with chronic alcohol consumption55 60 63 64 |
Advise patients of risks of such concomitant use1 |
|
Alprazolam |
||
|
Antiarrhythmics: class 1C (e.g., flecainide, propafenone) |
Potential for decreased clomipramine metabolisma |
Monitor for TCA toxicitya |
|
Anticholinergic agents |
||
|
Antipsychotic agents (e.g., phenothiazines) |
Hyperthermia and adverse effects resembling NMS1 157 199 Potential for decreased clomipramine metabolismc |
Dosage adjustment may be neededc |
|
Barbiturates (e.g., phenobarbital) |
May be additive with or may potentiate CNS effects1 159 Possible decreased plasma clomipramine concentrations1 159 Increased plasma phenobarbital concentrations reported1 |
Advise patients of risks associated with such concomitant use1 |
|
Cimetidine |
Potential increased plasma clomipramine concentrations1 159 c |
Use with caution; dosage adjustment may be neededc |
|
CNS depressants (e.g., alcohol, sedatives, hypnotics) |
Use with cautionc |
|
|
Digoxin |
Possible altered protein binding of clomipramine or digoxin1 2 |
|
|
Haloperidol |
Potential for increased plasma clomipramine concentrations1 2 |
Use with caution; dosage adjustment may be neededc |
|
Hypotensive agents (e.g., clonidine, guanethidine) |
Monitor BPc |
|
|
Levodopa |
May interfere with levodopa absorptionc |
Monitor levodopa dosage carefullyc |
|
Lithium |
||
|
MAO inhibitors (e.g., phenelzine) |
Potentially life-threatening serotonin syndrome1 2 159 160 Status epilepticus reported with concomitant phenelzine use2 3 161 |
Concomitant use contraindicated1 c Allow at least 14 days to elapse when switching to or from these drugs1 c |
|
Methylphenidate |
||
|
Oral contraceptives |
No evidence of interference with clomipramine therapeutic effects159 |
|
|
Phenytoin |
||
|
SSRIs (e.g., fluoxetine, fluvoxamine) |
Possible serotonin syndromec Potential decreased clomipramine metabolism and increased plasma concentrationsa c Possible seizures with concomitant fluoxetine use170 Severalfold elevation of plasma clomipramine concentration with concomitant fluvoxamine use171 |
Use with caution;c monitor for TCA toxicitya Allow at least 5 weeks to elapse when switching from fluoxetinea c |
|
Smoking |
Possible decreased plasma clomipramine concentrations1 2 41 55 60 |
|
|
Sympathomimetic agents (e.g., amphetamines, epinephrine, isoproterenol, norepinephrine, phenylephrine) |
Increased vasopressor, cardiac effectsc |
Use with caution; dosage adjustment may be requiredc |
|
Thyroid agents (e.g., levothyroxine, liothyronine) |
May accelerate the onset of therapeutic effects of TCAc Possible cardiac arrhythmiasc |
Use with cautionc |
|
Valproic acid |
Possible elevated serum clomipramine concentrations; may precipitate seizures in predisposed individuals298 |
|
|
Warfarin |
Possible altered protein binding of clomipramine or warfarin1 2 |
clomiPRAMINE Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration,2 3 4 5 10 55 with peak plasma concentrations usually attained within 2–6 hours (mean: 4.7 hours).1 10 11 12 25 29
Oral bioavailability is about 50% because of extensive first-pass metabolism.1 2 25 55
Onset
Therapeutic response in OCD generally occurs within 2–6 weeks, with maximal effects after 3–4 months.33 66 99 103
Food
Food does not appear to substantially affect bioavailability from capsules.1 29
Special Populations
In geriatric patients, plasma concentrations of clomipramine and its major active metabolite (desmethylclomipramine) are substantially higher than those in younger adults (18–40 years of age).1 41 60
In children <15 years of age, plasma concentration-dose ratios of clomipramine are substantially lower than those of adults.1 43
In smokers, steady-state plasma clomipramine concentrations are substantially lower than in nonsmokers;1 41 55 60 smoking appears to have less effect on plasma concentrations of desmethylclomipramine.60
Distribution
Extent
Clomipramine and desmethylclomipramine widely distributed in body tissues, with moderate to high concentrations occurring in organs such as the lungs, adrenals, kidneys, heart, and brain.1 3 5 10 53
Crosses the blood-brain barrier; desmethylclomipramine concentration in CSF is about 2.6 times higher than in plasma.1
Crosses the placenta and distributes into milk.1 4 22 55 60 62 71
Plasma Protein Binding
Approximately 97–98%, principally to albumin and possibly to α1-acid glycoprotein (α1-AGP).1 2 4 29 55 56
Elimination
Metabolism
Extensively metabolized to active metabolites1 2 3 4 5 19 20 55 61 72 73 by various CYP isoenzymes (e.g., CYP1A2,346 CYP2C,73 CYP2D6,72 73 CYP3A4).c
Exhibits nonlinear pharmacokinetics at dosages >150 mg daily.1 8 Metabolism of clomipramine and desmethylclomipramine may be capacity limited (saturable).1 8 55
Elimination Route
Clomipramine and metabolites excreted in urine and in feces (via biliary elimination).1 4 5 11 21 29 55 73
Half-life
Elimination half-lives of clomipramine and desmethylclomipramine are approximately 32 hours (range: 19–37 hours) and 69 hours (range: 54–77 hours), respectively, after a 150-mg oral dose.1 2
Elimination half-lives may be considerably prolonged at dosages near upper limit of recommended dosage range (i.e., 200–250 mg daily).1 8
Special Populations
Effects of renal and hepatic impairment on the disposition of clomipramine have not been fully elucidated.1 60
Hemodialysis, peritoneal dialysis, forced diuresis, and/or exchange transfusion are unlikely to remove clomipramine and desmethylclomipramine substantially because of the drug’s rapid distribution into body tissues.1
Stability
Storage
Oral
Capsules
Tightly closed container at ≤30°C.1 Protect from moisture.1
Actions
-
Mechanism of action in the management of OCD unknown but may involve inhibition of reuptake of serotonin.1 2 3 213 214 220
-
Desmethylclomipramine inhibits norepinephrine reuptake;2 3 4 48 212 213 214 220 221 235 therefore, clomipramine also shares pharmacologic profile of other tricyclic antidepressants.235 238
-
Exhibits marked anticholinergic activity, which may account for 3 4 288 289 sedation,1 65 238 242 adverse cardiovascular effects,1 2 193 222 235 339 and reduced seizure threshold (particularly at relatively high dosages).1 210
Advice to Patients
-
Risk of suicidality; importance of patients, family, and caregivers being alert to and immediately reporting emergence of suicidality, worsening depression, or unusual changes in behavior, especially during the first few months of therapy or during periods of dosage adjustment.d e f FDA recommends providing written patient information (medication guide) explaining risks of suicidality each time the drug is dispensed.d e f
-
Importance of informing patients about the risk of seizures associated with the drug.1
-
Importance of discussing with patients the risk of serious injury to themselves or others resulting from sudden loss of consciousness (e.g., because of seizures) while engaged in certain complex and hazardous activities (e.g., operation of complex machinery, driving a motor vehicle, swimming, climbing).1
-
Importance of cautioning patients about the use of alcohol, barbiturates, or other CNS depressants (see Interactions).1 243
-
Importance of informing male patients about the relatively high incidence of sexual dysfunction associated with the drug.1 3 180
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
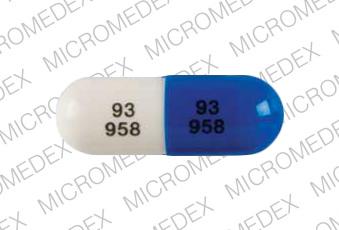
25 mg* |
Anafranil (with parabens) |
Mallinckrodt |
|
clomiPRAMINE Hydrochloride Capsules |
Mylan |
|||
|
50 mg* |
Anafranil (with parabens) |
Mallinckrodt |
||
|
clomiPRAMINE Hydrochloride Capsules |
Mylan |
|||
|
75 mg* |
Anafranil (with parabens) |
Mallinckrodt |
||
|
clomiPRAMINE Hydrochloride Capsules |
Mylan |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 1, 2007. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Novartis Pharmaceuticals. Anafranil (clomipramine hydrochloride) capsules prescribing information (dated 1998 Apr). In: Physician’s desk reference. 54th ed. Montvale, NJ: Medical Economics Company Inc; 2000:1988-92.
2. Peters MD II, Davis SK, Austin LS. Clomipramine: an antiobsessional tricyclic antidepressant. Clin Pharm. 1990; 9:165-78. https://pubmed.ncbi.nlm.nih.gov/2180623
3. Kelly MW, Myers CW. Clomipramine: a tricyclic antidepressant effective in obsessive compulsive disorder. DICP. 1990; 24:739-44. https://pubmed.ncbi.nlm.nih.gov/2197816
4. McTavish D, Benfield P. Clomipramine: an overview of its pharmacological properties and a review of its therapeutic use in obsessive compulsive disorder and panic disorder. Drugs. 1990; 39:136-53. https://pubmed.ncbi.nlm.nih.gov/2178909
5. Faigle JW, Dieterle W. The metabolism and pharmacokinetics of clomipramine (Anafranil). J Int Med Res. 1973; 1:281-90.
6. Luscombe DK, Wright J, Stern RS et al. Plasma concentrations of clomipramine and desmethylclomipramine in obsessive-compulsive neurosis. Postgrad Med J. 1980; 56(Suppl 1):140-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425517/ https://pubmed.ncbi.nlm.nih.gov/7393825
7. Luscombe DK, Marks IM. Pharmacokinetic studies in obsessional patients. J Int Med Res. 1977; 5(Suppl 5):91-6. https://pubmed.ncbi.nlm.nih.gov/598610
8. Kuss HJ, Jungkunz G. Nonlinear pharmacokinetics of chlorimipramine after infusion and oral administration in patients. Prog Neuropschopharmacol Biol Psychiatry. 1986; 10:739-48.
9. Burch JE, Shaw DM, Michalakeas A et al. Time course of plasma drug levels during once-daily oral administration of clomipramine. Psychopharmacology. 1982; 77:344-7. https://pubmed.ncbi.nlm.nih.gov/6813895
10. Luscombe DK. Pharmacokinetics of clomipramine. Br J Clin Pract. 1979; 33(Suppl 3):35-50.
11. Jones RB, Luscombe DK. Single dose studies with clomipramine in normal subjects. Postgrad Med J. 1976; 52(Suppl 3):62-7. https://pubmed.ncbi.nlm.nih.gov/959092
12. Jones RB, Luscombe DK. Plasma levels of clomipramine and its N- desmethyl metabolite following oral administration of clomipramine in man. Br J Pharmacol. 1976 Jul;57(3):430P.
13. Gringras M, Luscombe DK, Jones RB et al. A clinical trial of a 50 mg formulation of clomipramine (Anafranil) with steady-state plasma level measurements. J Int Med Res. 1977; 5(Suppl 1):119-24. https://pubmed.ncbi.nlm.nih.gov/863081
14. Jones RB, Luscombe DK. Plasma level studies with clomipramine (Anafranil). J Int Med Res. 1977; 5(Suppl 1):89-107.
15. Alfredsson G, Wiesel FA, Fyro B et al. Mass fragmentographic analysis of clomipramine and its mono-demthylated metabolite in human plasma. Psychopharmacology. 1977; 52:25-30. https://pubmed.ncbi.nlm.nih.gov/403553
16. Stern RS, Cobb JP, Marks IM et al. A preliminary report on clinical response and plasma levels of clomipramine and desmethylclomipramine in obsessive-compulsive neurosis. Postgrad Med J. 1977; 53(Suppl 4):97-103. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2496633/ https://pubmed.ncbi.nlm.nih.gov/341110
17. Carnis G, Godbillon J, Metayer JP. Determination of clomipramine and desmethyl-clomipramine in plasma or urine by the double-radioisotope derivative technique. Clin Chem. 1976; 22:817-23. https://pubmed.ncbi.nlm.nih.gov/6163
18. Broadhurst AD, James HD, Della Corte L et al. Clomipramine plasma level and clinical response. Postgrad Med J. 1977; 53(Suppl 4):139-45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2496476/
19. Linnoila M, Insel T, Kilts C et al. Plasma steady-state concentrations of hydroxylated metabolites of clomipramine. Clin Pharmacol Ther. 1982; 32:208-11. https://pubmed.ncbi.nlm.nih.gov/7094507
20. Nagy A, Johansson R. The demethylation of imipramine and clomipramine as apparent from their plasma kinetics. Psychopharmacology. 1977; 54:125-31. https://pubmed.ncbi.nlm.nih.gov/412206
21. Dubois JP, Kung W, Theobald W et al. Measurement of clomipramine, N-desmethylclomipramine, imipramine, and dehydroimipramine in biological fluids by selective ion monitoring, and pharmacokinetics of clomipramine. Clin Chem. 1976; 22:892-7. https://pubmed.ncbi.nlm.nih.gov/1277478
22. Takemura M, Toshida S, Fuchino K. Excretion of clomipramine and desmethylclomipramine in human breast milk. Seishin Igaku. 1982; 24: 749- 53.
23. Vandel B, Vandel S, Jounet JM et al. Relationship between the plasma concentration of clomipramine and desmethylclomipramine in depressive patients and the clinical response. Eur J Clin Pharmacol. 1982; 22:15-20. https://pubmed.ncbi.nlm.nih.gov/7094971
24. Moody JP. The biological availability of clomipramine (Anafranil). J Int Med Res. 1973; 1:325-30.
25. Evans LEJ, Bett JHN, Cox JR et al. The bioavailability of oral and parenteral chlorimipramine (Anafranil). Prog Neuro-pychopharmacol Biol Psychiatry. 1980; 4:293-302.
26. Bertilsson L, Braithwaite R, Tybring G et al. Techniques for plasma protein binding of demethylchlorimipramine. Clin Pharmacol Ther. 1979; 26:265-71. https://pubmed.ncbi.nlm.nih.gov/455895
27. Jones RB, Luscombe DK. Plasma concentrations of clomipramine and its N-desmethyl metabolite in depressive patients following treatment with various dosage regimes of clomipramine. Postgrad Med Journal. 1977; 53(Suppl 4):63-76.
28. Mellstrom B, Tybring G. Ion-pair liquid chromatography of steady-state plasma levels of chlorimipramine and demethylchlorimipramine. Journal of Chromatography. 1977; 143:597-605. https://pubmed.ncbi.nlm.nih.gov/914950
29. Jermain DM, Crismon ML. Pharmacotherapy of obsessive-compulsive disorder. Pharmacotherapy. 1990; 10:175-98. https://pubmed.ncbi.nlm.nih.gov/2196535
30. Stern RS, Marks IM, Mawson D et al. Clomipramine and exposure for compulsive rituals: II. plasma levels, side effects and outcome. Br J Psychiatry. 1980; 136:161-6. https://pubmed.ncbi.nlm.nih.gov/7370482
31. Stern RS, Marks IM, Wright J et al. Clomipramine: plasma levels, side effects and outcome in obsessive-compulsive neurosis. Postgrad Med J. 1980; 56(Suppl 1):134-9. https://pubmed.ncbi.nlm.nih.gov/7393824
32. Kasvikis Y, Marks IM. Clomipramine in obsessive-compulsive ritualisers treated with exposure therapy: relations betweeen dose, plasma levels, outcome and side effects. Psychopharmacology. 1988; 95:113-8. https://pubmed.ncbi.nlm.nih.gov/3133689
33. Insel TR, Murphy DL, Cohen RM et al. Obsessive-compulsive disorder: a double-blind trial of clomipramine and clorgyline. Arch Gen Psychiatry. 1983; 40:605-12. https://pubmed.ncbi.nlm.nih.gov/6342562
34. Thoren P, Asberg M, Bertilsson L et al. Clomipramine treatment of obsessive-compulsive disorder: II. biochemical aspects. Arch Gen Psychiatry. 1980; 37:1289-94. https://pubmed.ncbi.nlm.nih.gov/6159865
35. Flament MF, Rapoport JL, Berg CJ et al. Clomipramine treatment of childhood obsessive-compulsive disorder: a double-blind controlled study. Arch Gen Psychiatry. 1985; 42:977-83. https://pubmed.ncbi.nlm.nih.gov/3899048
36. Mavissakalian MR, Jones B, Olson S et al. Clomipramine in obsessive- compulsive disorder: clinical response and plasma levels. J Clin Psychopharmacol. 1990; 10:261-8. https://pubmed.ncbi.nlm.nih.gov/2286699
37. Mavrissakalian M, Jones B, Olson S et al. The relationship of plasma clomipramine and N-desmethylclomipramine to response in obsessive-compulsive disorder. Psychopharmacol Bull. 1990; 26:119-22. https://pubmed.ncbi.nlm.nih.gov/2371366
38. Della Corte L, Broadhurst AD, Sgaragli GP et al. Clinical response and tricyclic plasma levels during treatment with clomipramine. Br J Psychiatry. 1979; 134:390-400. https://pubmed.ncbi.nlm.nih.gov/444789
39. Dutt JE. On the clinical response/plasma level relationship for clomipramine. Br J Psychiatry. 1982; 140:105. https://pubmed.ncbi.nlm.nih.gov/7059735
40. Dawling S, Braithwaite RA, McAuley R et al. Single oral dose pharmacokinetics of clomipramine in depressed patients. Postgrad Med J. 1980; 56(Suppl 1):115-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425519/ https://pubmed.ncbi.nlm.nih.gov/7393820
41. John VA, Luscombe DK, Kemp H. Effects of age, cigarette smoking and the oral contraceptive on the pharmacokinetics of clomipramine and its desmethyl metabolite during chronic dosing. J Int Med Res. 1980; 8(Suppl 3):88-95. https://pubmed.ncbi.nlm.nih.gov/7202824
42. Luscombe DK, John V. Influence of age, cigarette smoking and the oral contraceptive on plasma concentrations of clomipramine. Postgrad Med J. 1980; 56(Suppl 10:99-102.
43. Dugas M, Zarifian E, Leheuzey MF et al. Preliminary observations of the significance of monitoring tricyclic antidepressant plasma levels in the pediatric patient. Therapeutic Drug Monitoring. 1980; 2:307-14. https://pubmed.ncbi.nlm.nih.gov/7222184
44. Miller P, Luscombe DK, Jones RB et al. Relationships between clinical response, plasma levels and side-effects of clomipramine (Anafranil) in general practitioner trials. J Int Med Res. 1977; 5(Suppl 1):108-18. https://pubmed.ncbi.nlm.nih.gov/863079
45. Montgomery SA, McAuley R, Montgomery DB et al. Plasma concentration of clomipramine and desmethylclomipramine and clinical response in depressed patients. Postgrad Med J. 1980; 56(Suppl 1):130-3. https://pubmed.ncbi.nlm.nih.gov/7393823
46. Moyes ICA, Ray RL, Moyes RB. Plasma levels and clinical improvement - a comparative study of clomipramine and amitriptyline in depression. Postgrad Med J. 1980; 56(Suppl 1):127-9. https://pubmed.ncbi.nlm.nih.gov/7393822
47. Reisby N, Gram LF, Bech P et al. Clomipramine: plasma levels and clinical effects. Commun Psychopharmacol. 1979; 3:341-51. https://pubmed.ncbi.nlm.nih.gov/548213
48. Traskman L, Asberg M, Bertilsson L et al. Plasma levels of chlorimipramine and its demethyl metabolite during treatment of depression. Clin Pharmacol Ther. 1979; 26:600-10. https://pubmed.ncbi.nlm.nih.gov/498703
49. Mulgirigama LD, Pare CMB, Turner P et al. Clinical response in depressed patients in relation to plasma levels of tricyclic antidepressants and tyramine pressor response. Postgrad Med J. 1977; 53(Suppl 4):155-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2496471/ https://pubmed.ncbi.nlm.nih.gov/341104
50. Faravelli C, Ballerini A, Broadhurst AD et al. Relevance of plasma levels during clomipramine treatment of primary depression. J Affect Disord. 1982; 4:163-5. https://pubmed.ncbi.nlm.nih.gov/6213693
51. Faravelli C, Ballerini A, Ambonetti A et al. Plasma levels and clinical response during treatment with clomipramine. J Affect Disord. 1984; 6:95-107. https://pubmed.ncbi.nlm.nih.gov/6231334
52. Montastruc JL, Tran MA, Blanc M et al. Measurement of plasma levels of clomipramine in the treatment of chronic pain. Clin Neuropharmacol. 1985; 8:78-82. https://pubmed.ncbi.nlm.nih.gov/3978652
53. Pounder DJ, Jones GR. Post-mortem drug redistribution - a toxicological nightmare. Forensic Sci Int. 1990; 45:253-63. https://pubmed.ncbi.nlm.nih.gov/2361648
54. Hullin RP. Variation in plasma concentrations of clomipramine and desmethylclomipramine during clomipramine therapy. Postgrad Med J. 1980; 56(Suppl 1):117-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425509/ https://pubmed.ncbi.nlm.nih.gov/7190279
55. Balant-Gorgia AE, Gex-Fabry M, Balant LP. Clinical pharmacokinetics of clomipramine. Clin Pharmacokinet. 1991; 20:447-62. https://pubmed.ncbi.nlm.nih.gov/2044329
56. Martensson E, Axelsson R, Nyberg G et al. Pharmacokinetic properties of the antidepressant drugs amitriptyline, clomipramine, and imipramine: a clinical study. Curr Ther Res. 1984; 36:228-38.
57. Balant-Gorgia AE, Balant LP, Genet C et al. Importance of oxidative polymorphism and levomepromazine treatment on the steady-state blood concentrations of clomipramine and its major metabolites. Eur J Clin Pharmacol. 1986; 31:449-55. https://pubmed.ncbi.nlm.nih.gov/2880723
58. Balant-Gorgia AE, Balant LP, Garrone G. High blood concentrations of imipramine or clomipramine and therapeutic failure: a case report study using drug monitoring data. Ther Drug Monit. 1989; 11:415-20. https://pubmed.ncbi.nlm.nih.gov/2741190
59. Balant-Gorgia AE, Balant L, Zysset T. High plasma concentrations of desmethylclomipramine after chronic administration of clomipramine to a poor metabolizer. Eur J Clin Pharmacol. 1987; 32:101-2. https://pubmed.ncbi.nlm.nih.gov/3582462
60. Goodnick PJ. Pharmacokinetic optimisation of therapy with newer antidepressants. Clin Pharmacokinet. 1994; 27:307-330. https://pubmed.ncbi.nlm.nih.gov/7834966
61. Nielsen KK, Brosen K. High-performance liquid chromatography of clomipramine and metabolites in human plasma and urine. Ther Drug Monit. 1993; 15:122-8. https://pubmed.ncbi.nlm.nih.gov/8503140
62. Wisner KL, Perel JM, Foglia JP. Serum clomipramine and metabolite levels in four nursing mother-infant pairs. J Clin Psychiatry. 1995; 56:17-20. https://pubmed.ncbi.nlm.nih.gov/7836334
63. Gex-Fabry M, Balant-Gorgia AE, Balant LP et al. Clomipramine metabolism: model-based analysis of variability factors from drug monitoring data. Clin Pharmacokinet. 1990; 19:241-55. https://pubmed.ncbi.nlm.nih.gov/2394063
64. Balant-Gorgia AE, Gay M, Gex-Fabry M et al. Persistent impairment of clomipramine demethylation in recently detoxified alcoholic patients. Ther Drug Monit. 1992; 14:119-24. https://pubmed.ncbi.nlm.nih.gov/1585395
65. The Clomipramine Collaborative Study Group. Clomipramine in the treatment of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1991; 48:730-8. https://pubmed.ncbi.nlm.nih.gov/1883256
66. DeVeaugh-Geiss J, Landau P, Katz R. Treatment of obsessive compulsive disorder with clomipramine. Psychiatric Annals. 1989; 19:97- 101.
67. DeVeaugh-Geiss J, Landau P, Katz R. Preliminary results from a multicenter trial of clomipramine in obsessive-compulsive disorder. Psychopharmacol Bull. 1989; 25:36-40. https://pubmed.ncbi.nlm.nih.gov/2672070
68. Pigott TA, Pato MT, Bernstein SE et al. Controlled comparisons of clomipramine and fluoxetine in the treatment of obsessive-compulsive disorder: behavioral and biological results. Arch Gen Psychiatry. 1990; 47:926-32. https://pubmed.ncbi.nlm.nih.gov/2222131
69. Greist JH, Jefferson JW, Kobak KA et al. Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder: a meta-analysis. Arch Gen Psychiatry. 1995; 52:53-60. https://pubmed.ncbi.nlm.nih.gov/7811162
70. Katz RJ, DeVeaugh-Geiss J, Landau P. Clomipramine in obsessive- compulsive disorder. Biol Psychiatry. 1990; 28:401-14. https://pubmed.ncbi.nlm.nih.gov/2207219
71. Schimmell MS, Katz EZ, Shaag Y et al. Toxic neonatal effects following maternal clomipramine therapy. J Toxicol Clin Toxicol. 1991; 29:479-84. https://pubmed.ncbi.nlm.nih.gov/1749054
72. Nielsen KK, Brosen K, Gram LF et al. Steady-state plasma levels of clomipramine and its metabolites: impact of the sparteine/debrisoquine oxidation polymorphism. Eur J Clin Pharmacol. 1992; 43:405-11. https://pubmed.ncbi.nlm.nih.gov/1451721
73. Nielsen KK, Brosen K, Hansen MGJ et al. Single-dose kinetics of clomipramine: relationship to the sparteine and S-mephenytoin oxidation polymorphisms. . Clin Pharmacol Ther. 1994; 55:518-27.
74. Nielsen KK, Brosen K, Hansen MGJ et al. Gluconidation clearance of 8- hydroxyclomipramine in relation to sparteine and mephenytoin phenotype. Eur J Clin Pharmacol. 1994; 47:209-10. https://pubmed.ncbi.nlm.nih.gov/7859811
75. Allen JJ, Rack PH, Vaddadi KS. Differences in the effects of clomipramine on English and Asian volunteers. prelimminary report on a pilot study. Postgrad Med J. 1977; 53(Suppl 4):79-86. https://pubmed.ncbi.nlm.nih.gov/341109
76. Shimoda K, Minowada T, Noguchi T et al. Interindividual variations of desmethylation and hydroxylation of clomipramine in an oriental psychiatric population. J Clin Psychopharmacol. 1993; 13:181-8. https://pubmed.ncbi.nlm.nih.gov/8354734
77. Ackerman DL, Greenland S, Bystritsky A et al. Predictors of treatment response in obsessive-compulsive disorder: multivariate analyses from a multicenter trial of clomipramine. J Clin Psychopharmacol. 1994; 14:247- 54. https://pubmed.ncbi.nlm.nih.gov/7962680
78. Pato MT, Zohar-Kadouch R, Zohar J et al. Return of symptoms after discontinuation of clomipramine in patients with obsessive-compulsive disorder. Am J Psychiatry. 1988; 145:1521-5. https://pubmed.ncbi.nlm.nih.gov/3057923
79. Katz RJ, DeVeaugh-Geiss J. The antiobsessional effects of clomipramine do not require concomitant affective disorder. Psychiatry Res. 1990; 31:121-9. https://pubmed.ncbi.nlm.nih.gov/2183254
80. Marks IM, Stern RS, Mawson D et al. Clomipramine and exposure for obsessive-compulsive rituals: I. Br J Psychiatry. 1980; 136:1-25. https://pubmed.ncbi.nlm.nih.gov/6986939
81. Thoren P, Asberg M, Cronholm B et al. Clomipramine treatment of obsessive-compulsive disorder: I. a controlled clinical trial. Arch Gen Psychiatry. 1980; 37:1281-5. https://pubmed.ncbi.nlm.nih.gov/7436690
82. Leonard HL, Swedo SE, Lenane MC et al. A double-blind desipramine substitution during long-term clomipramine treatment in children and adolescents with obsessive-compulsive disorder. Arch Gen Psychiatry. 1991; 48:922-7. https://pubmed.ncbi.nlm.nih.gov/1929762
83. Freeman CPL, Trimble MR, Deakin JFW et al. Fluvoxamine versus clomipramine in the treatment of obsessive compulsive disorder: a multicenter, randomized, double-blind, parallel group comparison. J Clin Psychiatry. 1994; 55:301-5. https://pubmed.ncbi.nlm.nih.gov/8071291
84. Marks IM, Lelliott P, Basoglu M et al. Clomipramine, self-exposure and therapist-aided exposure for obsessive-compulsive rituals. Br J Psychiatry. 1988; 152:522-34. https://pubmed.ncbi.nlm.nih.gov/3167404
85. Berman I, Sapers BL, Chang HHJ et al. Treatment of obsessive- compulsive symptoms in schizophrenic patients with clomipramine. J Clin Psychopharmacol. 1995; 15:206-10. https://pubmed.ncbi.nlm.nih.gov/7635998
86. Tejera CA, Mayerhoff DI, Ramos-Lorenzi J. Clomipramine for obsessive-compulsive symptoms in schizophrenia. J Clin Psychopharmacol. 1993; 13:290-1. https://pubmed.ncbi.nlm.nih.gov/8376620
87. O’sullivan G, Noshirvani H, Marks I et al. Six-year follow-up after exposure and clomipramine therapy for obsessive compulsive disorder. J Clin Psychiatry. 1991; 52:150-5. https://pubmed.ncbi.nlm.nih.gov/2016246
88. Yaryura-Tobias JA, Neziroglu F, Bergman L. Chlorimipramine, for obsessive-compulsive neurosis: an organic approach. Curr Ther Res. 1976; 20:541-8.
89. Greist JH, Jefferson JW, Rosenfeld R et al. Clomipramine and obsessive compulsive disorder: a placebo-controlled double-blind study of 32 patients. J Clin Psychiatry. 1990; 51:292-7. https://pubmed.ncbi.nlm.nih.gov/2195006
90. Lee S. Clomipramine in obsessive compulsive disorder. J Clin Psychiatry. 1991; 52:183-4. https://pubmed.ncbi.nlm.nih.gov/2016256
91. Greist JH, Jefferson JW. Drs. Greist and Jefferson reply. J Clin Psychiatry. 1991; 52:184-5.
92. Jenike MA, Baer L, Summergrad P et al. Obsessive-compulsive disorder: a double-blind, placebo-controlled trial of clomipramine in 27 patients. Am J Psychiatry. 1989; 146:1328-30. https://pubmed.ncbi.nlm.nih.gov/2675643
93. Yaryura-Tobias JA. Chlorimipramine in Gilles de la Tourette’s disease. Am J Psychiatry. 1975; 132:1221. https://pubmed.ncbi.nlm.nih.gov/1058644
94. Ratzoni G, Hermesh H, Brandt N et al. Clomipramine efficacy for tics, obsessions, and compulsions in Tourette’s syndrome and obsessive-compulsive disorder: a case study. Biol Psychiatry. 1990; 27:95-8. https://pubmed.ncbi.nlm.nih.gov/2297555
95. Caine ED, Polinsky RJ, Ebert MH et al. Trial of chlorimipramine and desipramine for Gilles de la Tourette syndrome. Ann Neurol. 1979; 5:305- 6. https://pubmed.ncbi.nlm.nih.gov/375806
96. Koran LM, McElroy SL, Davidson JRT et al. Fluvoxamine versus clomipramine for obsessive-compulsive disorder: a double-blind comparison. J Clin Psychopharmacol. 1996; 16:121-9. https://pubmed.ncbi.nlm.nih.gov/8690827
97. Rasmussen SA. Lithium and tryptophan augmentation in clomipramine- resistant obsessive-compulsive disorder. Am J Psychiatry. 1984; 141:1283- 5. https://pubmed.ncbi.nlm.nih.gov/6435460
98. Feder R. Lithium augmentation of clomipramine. J Clin Psychiatry. 1988; 49:458. https://pubmed.ncbi.nlm.nih.gov/3141389
99. Pigott TA, Pato MT, L’Heureux F et al. A controlled comparison of adjuvant lithium carbonate or thyroid hormone in clompramine-treated patients with obsessive-compulsive disorder. J Clin Psychopharmacol. 1991; 11:242-8. https://pubmed.ncbi.nlm.nih.gov/1918422
100. Tamimi RR, Mavissakalian MR. Are effective antiobsessional drugs interchangeable? Arch Gen Psychiatry. 1991; 48:857-8. Letter.
101. Pigott TA, Murphy DL. Are effective antiobsessional drugs interchangeable? Arch Gen Psychiatry. 1991; 48:858-9. Letter.
102. Bark N, Lindenmayer JP. Ineffectiveness of clomipramine for obsessive-compulsive symptoms in a patient with schizophrenia. Am J Psychiatry. 1992; 149:136-7. https://pubmed.ncbi.nlm.nih.gov/1728163
103. Stroebel CF, Szarek BL, Glueck BC. Use of clomipramine in treatment of obsessive-compulsive symptomatology. J Clin Psychopharmacol. 1984; 4:98-100. https://pubmed.ncbi.nlm.nih.gov/6707247
104. Gloger S, Grunhaus L, Gladic D et al. Panic attacks and agoraphobia: low dose clomipramine treatment. J Clin Psychopharmacol. 1989; 9:28-32. https://pubmed.ncbi.nlm.nih.gov/2651491
105. Gloger S, Grunhaus L, Birmacher B et al. Treatment of spontaneous panic attacks with chlomipramine. Am J Psychiatry. 1981; 138:1215-7. https://pubmed.ncbi.nlm.nih.gov/7270727
106. Grunhaus L, Gloger S, Birmacher B. Clomipramine treatment for panic attacks in patients with mitral valve prolapse. J Clin Psychiatry. 1984; 45:25-7. https://pubmed.ncbi.nlm.nih.gov/6363396
107. Kahn RS, Westenberg HGM, Verhoeven WMA et al. Effect of a serotonin precursor and uptake inhibitor in anxiety disorders: a double-blind comparison of 5-hydroxytryptophan, clomipramine and placebo. Int Clin Psychopharmacol. 1987; 2:33-45. https://pubmed.ncbi.nlm.nih.gov/3312397
108. den Boer JA, Westenberg HGM, Kamerbeek WDJ et al. Effect of serotonin uptake inhibitors in anxiety disorders; a double-blind comparison of clomipramine and fluvoxamine. Int Clin Psychopharmacol. 1987; 2:21-32. https://pubmed.ncbi.nlm.nih.gov/3117876
109. Cassano GB, Petracca A, Perugi G et al. Clomipramine for panic disorder: I. the first 10 weeks of a long-term comparison with imipramine. J Affect Disord. 1988; 14:123-7. https://pubmed.ncbi.nlm.nih.gov/2966825
110. Johnston DG, Troyer IE, Whitsett SF. Clomipramine treatment of agoraphobic women: an eight-week controlled trial. Arch Gen Psychiatry. 1988; 453-9. (IDIS 241074)
111. Langohr HD, Stohr M, Petruch F. An open and double-blind cross-over study on the efficacy of clomipramine (Anafranil) in patients with painful mono- and polyneuropathies. Eur Neurol. 1982; 21:309-17. https://pubmed.ncbi.nlm.nih.gov/6126361
112. Ganvir P, Beaumont G, Seldrup J. A comparative trial of clomipramine and placebo as adjunctive therapy in arthralgia. J Int Med Res. 1980; 8(Suppl 3):60-6. https://pubmed.ncbi.nlm.nih.gov/7009255
113. Gerson GR, Jones RB, Luscombe DK. Studies on the concomitant use of carbamazepine and clomipramine for the relief of post-herpetic neuralgia. Postgrad Med J. 1977; 53(Suppl 4):104-9. https://pubmed.ncbi.nlm.nih.gov/304576
114. Carasso RL, Yehuda S, Streifler M. Clomipramine and amitriptyline in the treatment of severe pain. Int J Neurosci. 1979; 9:191-4. https://pubmed.ncbi.nlm.nih.gov/489262
115. Eberhard G, von Knorring L, Nilsson HL et al. A double-blind randomized study of clomipramine versus maprotiline in patients with idiopathic pain syndromes. Neuropsychobiology. 1988; 19:25-34. https://pubmed.ncbi.nlm.nih.gov/3054623
116. Modigh K, Westberg P, Eriksson E. Superiority of clomipramine over imipramine in the treatment of panic disorder: a placebo-controlled trial. J Clin Psychopharmacol. 1992; 12:251-61. https://pubmed.ncbi.nlm.nih.gov/1527228
117. Hoffart A, Due-Madsen J, Lande B et al. Clomipramine in the treatment of agoraphobic inpatients resistant to behavioral therapy. J Clin Psychiatry/. 1993; 54:481-7.
118. Magni G. The use of antidepressants in the treatment of chronic pain: a review of the current evidence. Drugs. 1991; 42:730-48. https://pubmed.ncbi.nlm.nih.gov/1723371
119. Langohr HD, Gerber WD, Koletzky E et al. Clomipramine and metaprolol in migraine prophylaxis—a double-blind crossover study. Headache. 1985; 25:107-13. https://pubmed.ncbi.nlm.nih.gov/3886599
120. Noone JF. Clomipramine in the prevention of migraine. J Int Med Res. 1980; 8(Suppl 3):49-52. https://pubmed.ncbi.nlm.nih.gov/7009254
121. Loldrup D, Langemark M, Hansen HJ et al. Clomipramine and mianserin in chronic idiopathic pain syndrome: a placebo controlled study. Psychopharmacology. 1989; 99:1-7. https://pubmed.ncbi.nlm.nih.gov/2506594
122. Langemark M, Lodrup D, Bech P et al. Clomipramine and mianserin in the treatment of chronic tension headache. a double-blind, controlled study. Headache. 1990; 30:118-21. https://pubmed.ncbi.nlm.nih.gov/2182566
123. Rummans TA. Nonopioid agents for treatment of acute and subacute pain. Mayo Clin Proc. 1994; 69:481-90. https://pubmed.ncbi.nlm.nih.gov/8080514
124. Panerai AE, Monza G, Movilia P et al. A randomized, within-patient, cross-over, placebo-controlled trial on the efficacy and tolerability of the tricyclic antidepressants chlorimipramine and nortriptyline in central pain. Acta Neurol Scand. 1990; 82:34-8. https://pubmed.ncbi.nlm.nih.gov/2239134
125. Sindrup SH, Gram LF, Skjold T et al. Clomipramine vs desipramine vs placebo in the treatment of diabetic neuropathy symptoms. a double-blind cross- over study. Br J Clin Pharmacol. 1990; 30:683-91. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1368167/ https://pubmed.ncbi.nlm.nih.gov/2271367
126. Calissi PT, Jaber LA. Peripheral diabetic neuropathy: current concepts in treatment. Ann Pharmacother. 1995; 29:769-77. https://pubmed.ncbi.nlm.nih.gov/8520095
127. Wright JM. Review of the symptomatic treatment of diabetic neuropathy. Pharmacotherapy. 1994; 14:689-97. https://pubmed.ncbi.nlm.nih.gov/7885972
128. Eaton H. Clomipramine (Anafranil) in the treatment of premature ejaculation. J Int Med Res. 1973; 1:432-4.
129. Goodman RE. An assessment of clomipramine (Anafranil) in the treatment of premature ejaculation. J Int Med Res. 1980; 8(Suppl 3):53-9. https://pubmed.ncbi.nlm.nih.gov/7193614
130. Girgis SM, El-Haggar S, El-Hermouzy S. A double-blind trial of clomipramine in premature ejaculation. Andrologia. 1982; 14:364-8. https://pubmed.ncbi.nlm.nih.gov/6751156
131. Althof SE, Levine SB, Corty EW et al. A double-blind crossover trial of clomipramine for rapid ejaculation in 15 couples. J Clin Psychiatry. 1995; 56:402-7. https://pubmed.ncbi.nlm.nih.gov/7665538
132. Shapiro WR. Treatment of cataplexy with clomipramine. Arch Neurol. 1975; 32:653-6. https://pubmed.ncbi.nlm.nih.gov/170899
133. Schachter M, Parkes JD. Fluvoxamine and clomipramine in the treatment of cataplexy. J Neurol Neurosurg Psychiatry. 1980; 43:171-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC490494/ https://pubmed.ncbi.nlm.nih.gov/6766990
134. Gilman JT, Tuchman RF. Autism and associated behavioral disorders: pharmacotherapeutic intervention. Ann Pharmacother. 1995; 29:47-56. https://pubmed.ncbi.nlm.nih.gov/7711345
135. Gordon CT, Rapoport JL, Hamburger SD et al. Differential response of seven subjects with autistic disorder to clomipramine and desipramine. Am J Psychiatry. 1992; 149:363-6. https://pubmed.ncbi.nlm.nih.gov/1536276
136. Swedo SE, Leonard HL, Rapoport JL et al. A double-blind comparison of clomipramine and desipramine in the treatment of trichotillomania (hair pulling). N Engl J Med. 1989; 321:497-501. https://pubmed.ncbi.nlm.nih.gov/2761586
137. Swedo SE, Lenane MC, Leonard HL. Long-term treatment of trichotillomania (hair pulling). N Engl J Med. 1993; 329:141-2. https://pubmed.ncbi.nlm.nih.gov/8510704
138. Black DW, Blum N. Trichotillomania treated with clomipramine and a topical steroid. Am J Psychiatry. 1992; 149:842-3. https://pubmed.ncbi.nlm.nih.gov/1303620
139. Gupta S, Freimer M. Trichotillomania, clomipramine, topical steroids. Am J Psychiatry. 1993; 150:524. https://pubmed.ncbi.nlm.nih.gov/8434676
140. Pollard CA, Ibe IO, Krojanker DN et al. Clomipramine treatment of trichotillomania: a floow-up report on four cases. J Clin Psychiatry. 1991; 52:128-30. https://pubmed.ncbi.nlm.nih.gov/2005076
141. Gordon CT, State RC, Nelson JE et al. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry. 1993; 50:441-7. https://pubmed.ncbi.nlm.nih.gov/8498878
142. Leonard HL, Lenane MC, Swedo SE et al. A double-blind comparison of clomipramine and desipramine treatment of severe onychophagia (nail biting). Arch Gen Psychiatry. 1991; 48:821-7. https://pubmed.ncbi.nlm.nih.gov/1929772
143. Gordon CT, Cotelingam GM, Stager S et al. A double-blind comparison of clomipramine and desipramine in the treatment of developmental stuttering. J Clin Psychiatry. 1995; 56:238-42. https://pubmed.ncbi.nlm.nih.gov/7775365
144. Matthew HJS. The management of self-poisoning due to clomipramine (Anafranil). J Int Med Res. 1973; 1:485-8.
145. Fraser AD, Isner AF, Moss MA. A fatality involving clomipramine. J Forensic Sci. 1986; 31:762-7. https://pubmed.ncbi.nlm.nih.gov/2872264
146. Haqqani MT, Gutteridge DR. Two cases of clomipramine hydrochloride (Anafranil) poisoning. Forensic Sci. 1974; 3:83-7. https://pubmed.ncbi.nlm.nih.gov/4426550
147. Meatherall RC, Guay DRP, Chalmers JL. A fatal overdose with clomipramine. J Anal Toxicol. 1983; 7:168-71. https://pubmed.ncbi.nlm.nih.gov/6632798
148. Diamond BI, Borison RL, Katz R et al. Rebound withdrawal reactions due to clomipramine. Psychopharmcol Bull. 1989; 25:209-12.
149. Committee on Drugs. The transfer of drugs and other chemicals into human milk. Pediatrics. 1994; 93:137-50. https://pubmed.ncbi.nlm.nih.gov/8265310
150. Eidelman AI, Schimmel MS. Drugs and breast milk. Pediatrics. 1995; 95:956-7. https://pubmed.ncbi.nlm.nih.gov/7761234
151. Berlin CM Jr. Drugs and breast milk. Pediatrics. 1995; 95:957-8. https://pubmed.ncbi.nlm.nih.gov/7761235
152. Cowe L, Lloyd DJ, Dawling S. Neonatal convulsions caused by withdrawal from maternal clomipramine. BMJ. 1982; 284:1837-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1498765/ https://pubmed.ncbi.nlm.nih.gov/6805722
153. Singh S, Gulati S, Narang A et al. Non-narcotic withdrawal syndrome in a neonate due to maternal clomipramine therapy. J Paediatr Child Health. 1990; 26:110. https://pubmed.ncbi.nlm.nih.gov/2361068
154. Ostergaard GZ, Pedersen SE. Neonatal effects of maternal clomipamine treatment. Pediatrics. 1982; 69:233-4. https://pubmed.ncbi.nlm.nih.gov/7058100
155. van Scheyen JD, van Kammen DP. Clomipramine-induced mania in unipolar depresssion. Arch Gen Psychiatry. 1979; 36:560-5. https://pubmed.ncbi.nlm.nih.gov/435016
156. van Kammen DP, van Scheyen JD, Murphy DL. Platelet monoamine oxidase activity and clomipramine-induced mania in unipolar depressed patients. Biol Psychiatry. 1980; 15:565-73. https://pubmed.ncbi.nlm.nih.gov/7397287
157. Ansseau M, Reynolds CF III, Kupfer DJ et al. Central dopaminergic and noradrenergic receptor blockade in a patient with neuroleptic malignant syndrome. J Clin Psychiatry. 1986; 47:320-1. https://pubmed.ncbi.nlm.nih.gov/3011760
158. Ben Musa A, Smith CS. Neonatal effects of maternal clomipramine therapy. Arch Dis Child. 1979; 54:405. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1545555/ https://pubmed.ncbi.nlm.nih.gov/486239
159. Beaumont G. Drug interactions with clomipramine (Anafranil). J Int Med Res. 1973; 1:480-4.
160. Tackley RM, Tregaskis B. Fatal disseminated intravascular coagulation following a monoamine oxidase inhibitor/tricyclic interaction. Anaesthesia. 1987; 42:760-3. https://pubmed.ncbi.nlm.nih.gov/3631476
161. Pascual J, Combarros O, Berciano J. Partial status epilepticus following single low dose of clorimipramine in a patient on MAO-inhibitor treatment. Clin Neuropharmacol. 1987; 10:565-7. https://pubmed.ncbi.nlm.nih.gov/3427564
162. Souhami RL, Ashton CR, Lee-Potter JP. Agranulocytosis and sytemic candidiasis following clomipramine therapy. Postgrad Med J. 1976; 52:472- 4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2496401/ https://pubmed.ncbi.nlm.nih.gov/967767
163. Magni G, Urbani A, Silvestro A et al. Clomipramine-induced pancytopenia. J Nerv Ment Dis. 1987; 175:309-10. https://pubmed.ncbi.nlm.nih.gov/3572384
164. Gravenor DS, Leclerc JR, Blake G. Tricyclic antidepressant agranulocytosis. Can J Psychiatry. 1986; 31:661. https://pubmed.ncbi.nlm.nih.gov/3779595
165. Hunt KA, Resnick MP. Clomipamine-induced agranulocytosis and its treatment with G-CSF. Am J Psychiatry. 1993; 150:522-3. https://pubmed.ncbi.nlm.nih.gov/7679557
166. Alderman CP, Atchison MM, McNeece JI. Concurrent agranulocytosis and hepatitis secondary to clomipramine therapy. Br J Psychiatry. 1993; 162:688-9. https://pubmed.ncbi.nlm.nih.gov/8149124
167. Roberge RJ, Martin TG, Hodgman M et al. Acute chemical pancreatitis associated with a tricyclic antidepressant (clomipramine) overdose. Clinical Toxicology. 1994; 32:425-9. https://pubmed.ncbi.nlm.nih.gov/8057402
168. Hulten BA, Adams R, Askenasi R et al. Predicting severity of tricyclic antidepressant overdose. Clinical Toxicology. 1992; 30:161-70. https://pubmed.ncbi.nlm.nih.gov/1588666
169. Bromiker R, Kaplan M. Apparent intrauterine fetal withdrawal from clomipramine hydrochloride. JAMA. 1994; 272:1722-3. https://pubmed.ncbi.nlm.nih.gov/7966912
170. Sternbach H. Fluoxetine-clomipramine interaction. J Clin Psychiatry. 1995; 56:171-2. https://pubmed.ncbi.nlm.nih.gov/7713858
171. Bertschy G, Vandel S, Vandel B et al. Fluvoxamine-tricyclic antidepressant interaction. Eur J Clin Pharmacol. 1991; 40:119-20. https://pubmed.ncbi.nlm.nih.gov/1905641
172. Nirenberg DW, Semprebon M. The central nervous system serotonin syndrome. /Clin Pharmacol Ther. 1993; 53:84-8.
173. Neuvonen PJ, Pohjola-Sintonen S, Tacke U et al. Five fatal cases of serotonin syndrome after moclobemide-citalopram or moclobemide-clomipramine overdoses. Lancet. 1993; 342:1419. https://pubmed.ncbi.nlm.nih.gov/7901695
174. Kojima H, Terao T, Yoshimura R. Serotonin syndrome during clomipramine and lithium treatment. Am J Psychiatry. 1993; 150:1897. https://pubmed.ncbi.nlm.nih.gov/8238650
175. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991; 148:705-13. https://pubmed.ncbi.nlm.nih.gov/2035713
176. Insel TR, Roy BF, Cohen RM et al. Possible development of the serotonin syndrome in man. Am J Psychiatry. 1982; 139:954-5. https://pubmed.ncbi.nlm.nih.gov/7091416
177. Spigset O, Mjorndal T. Serotonin syndrome caused by a moclobemide- clomipramine interaction. BMJ. 1993; 306:248. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1676747/ https://pubmed.ncbi.nlm.nih.gov/8443525
178. Cano-Munoz JL, Montejo-Iglesias ML, Yanez -Saez RM et al. Possible serotonin syndrome following the combined administration of clomipramine and alprazolam. J Clin Psychiatry. 1995; 56:122. https://pubmed.ncbi.nlm.nih.gov/7883731
179. Henry JA. Serotonin syndrome. Lancet. 1994; 343:607. https://pubmed.ncbi.nlm.nih.gov/7906365
180. Monteiro WO, Noshirvani HF, Marks IM et al. Anorgasmia from clomipramine in obsessive-compulsive disorder: a controlled trial. Br J Psychiatry. 1987; 151:107-12. https://pubmed.ncbi.nlm.nih.gov/3315086
181. McLean JD, Forsythe RG, Kapkin IA. Unusual side effects of clomipramine associated with yawning. Can J Psychiatry. 1983; 28:569-70. https://pubmed.ncbi.nlm.nih.gov/6652610
182. Fraser AR. Sexual dysfunction following antidepressant drug therapy. J Clin Psychopharmacol. 1984; 4:62-3. https://pubmed.ncbi.nlm.nih.gov/6693585
183. Quirk KC, Einarson TR. Sexual dysfunction and clomipramine. Can J Psychiatry. 1982; 27:228-31. https://pubmed.ncbi.nlm.nih.gov/7201341
184. Riley AJ, Riley EJ. Cyproheptadine and antidepressant-induced anorgasmia. Br J Psychiatry. 1986; 148:217-8. https://pubmed.ncbi.nlm.nih.gov/3697592
185. Price J, Grunhaus LJ. Treatment of clomipramine-induced anorgasmia with yohmibine: a case report. J Clin Psychiatry. 1990; 51:32-3. https://pubmed.ncbi.nlm.nih.gov/2295589
186. Anand VS. Clomipramine-induced galactorrhoea and amenorrhoea. Br Psychiatry. 1985; 147:87-8.
187. Fowlie S, Burton J. Hyperprolactinaemia and nonpuerperal lactation associated with clomipramine. Scott Med J. 1987; 32:52. https://pubmed.ncbi.nlm.nih.gov/3602989
188. Beaumont G. Sexual side-effects of clomipramine (Anafranil). J Int Med Res. 1973; 1:469-72.
189. Yassa R. Sexual disorders in the course of clomipramine treatment: a report of three cases. Can J Psychiatry. 1982; 27:148-9. https://pubmed.ncbi.nlm.nih.gov/7066846
190. Aizenberg D, Zemishlany Z, Hermesh H et al. Painful ejaculation associated with antidepressants in four patients. J Clin Psychiatry. 1991; 52:461-3. https://pubmed.ncbi.nlm.nih.gov/1744063
191. Myers BA, Klerman GL, Hartmann E. Nocturnal cataclysms with myoclonus: a new side effect of clomipramine. Am J Psychiatry. 1986; 143:1490-1. https://pubmed.ncbi.nlm.nih.gov/3777258
192. Pledger DR, Mathew H. Hyponatremia and clomipramine therapy. Br J Psychiatry. 1989; 154:263-4. https://pubmed.ncbi.nlm.nih.gov/2775959
193. Szarek BL, Goethe JW. Orthostatic hypotension as an indicator of response to clomipramine. Curr Ther Res. 1984; 36:54-7.
194. Ananth J, Assalian P. Intolerable side effects of clomipramine. J Clin Psychopharmacol. 1982; 2:215-6. https://pubmed.ncbi.nlm.nih.gov/7096611
195. Hermesh H, Aizenberg D, Weizman A et al. Clomipramine-induced urinary dysfunction in an obsessive-compulsive adolescent. Drug Intell Clin Pharm. 1987; 21:877-9. https://pubmed.ncbi.nlm.nih.gov/3678059
196. Casas M, Garcia-Ribera C, Alvarez E et al. Myoclonic movements as a side-effect of treatment with therapeutic doses of clomipramine. Int Clin Psychopharmacol. 1987; 2:333-6. https://pubmed.ncbi.nlm.nih.gov/3693873
197. Fukuzako H, Hokazono Y, Tominaga H et al. Jerk-locked averaging and somatosensory evoked potential in tricyclic-induced myoclonus: a case report. Japanese Journal of Psychiatry and Neurology. 1989; 43:645-9. https://pubmed.ncbi.nlm.nih.gov/2637391
198. Gersten SP. Tardive dyskinesia-like syndromes with clomipramine. Am J Psychiatry. 1993; 150:165-6. https://pubmed.ncbi.nlm.nih.gov/8417563
199. Domingo P, Munoz J, Bonastre M et al. Benign type of malignant syndrome. Lancet. 1989; 1:50. https://pubmed.ncbi.nlm.nih.gov/2563035
200. Chithiramohan RN, Ballard CG, Measey LG. Acute dystonia induced by clomipramine therapy. Irish Journal of Psychological Medicine. 1990; 7:141-2.
201. Bental E, Lavie P, Sharf B. Severe hypermotility during sleep in treatment of cataplexy with clomipramine. Isr J Med Sci. 1979; 15:607-9. https://pubmed.ncbi.nlm.nih.gov/478825
202. Moshe K, Iulian I, Seth K et al. Clomipramine-induced Tourettism in obsessive-compulsive disorder: clinical and theoretical implications. Clin Neuropharmacol. 1994; 17:338-43. https://pubmed.ncbi.nlm.nih.gov/9316681
203. Robinson ML. Epileptic fit after clomipramine. Br J Psychiatry. 1978; 132:525-6.
204. Hessov I. Hypertension during chlorimipramine therapy. Br Med J. 1971; 1:406. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1795008/ https://pubmed.ncbi.nlm.nih.gov/5541936
205. Tunca Z, Tunca MI, Dilsiz U et al. Clomipramine-induced pseudocyanotic pigmentation. Am J Psychiatry. 1989; 146:552-3.
206. Marley J. Acute polyradiculoneuropathy after amitriptyline overdose. BMJ. 1987; 294:1616. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1246760/
207. Larrey D, Rueff B, Pessayre D et al. Cross hepatotoxicity between tricyclic antidepressants. Gut. 1986; 27:726-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1433318/ https://pubmed.ncbi.nlm.nih.gov/3721296
208. DeVries MW, Peeters F. Dental caries with longterm use of antidepressants. Lancet. 1995; 346:1640. https://pubmed.ncbi.nlm.nih.gov/7500792
209. Schlingemann RO, Smit AAJ, Verduyn Lunel HFE et al. Amaurosis fugax on standing and angle-closure glaucoma with clomipramine. Lancet. 1996; 347:465.
210. Rosenstein DL, Nelson JC, Jacobs SC. Seizures associated with antidepressants: a review. J Clin Psychiatary. 1993; 54:289-99.
211. Lejoyeux M, Fineyre F, Ades J. The serotonin syndrome. Am J Psychiatry. 1992; 149:1410-1. https://pubmed.ncbi.nlm.nih.gov/1530086
212. Zohar J, Insel TR, Zohar-Kadouch RC et al. Serotonergic responsivity in obsessive-compulsive disorder: effects of chronic clomipramine treatment. Arch Gen Psychiatry. 1988; 45:167-72. https://pubmed.ncbi.nlm.nih.gov/3276283
213. Benkelfat C, Murphy DL, Zohar J et al. Clomipramine in obsessive- compulsive disorder: further evidence for a serotonergic mechanism of action. Arch Gen Psychiatry. 1989; 46:23-8. https://pubmed.ncbi.nlm.nih.gov/2910220
214. Flament MF, Rapoport JL, Murphy DL et al. Biochemical changes during clomipramine treatment of childhood obsessive-compulsive disorder. Arch Gen Psychiatry. 1987; 44:219-25. https://pubmed.ncbi.nlm.nih.gov/3548637
215. Benkelfat C, Nordahl TE, Semple WE et al. Local cerebral glucose metabolic rates in obsessive-compulsive disorder: patients treated with clomipramine. Arch Gen Psychiatry. 1990; 47:840-8. https://pubmed.ncbi.nlm.nih.gov/2393342
216. Swedo SE, Pietrini P, Leonard HL et al. Cerebral glucose metabolism in childhood-onset obsessive-compulsive disorder: revisualization during pharmacotherapy. Arch Gen Psychiatry. 1992; 49:690-4. https://pubmed.ncbi.nlm.nih.gov/1514873
217. Pigott TA, Pato MT, Bernstein SE et al. Controlled comparisons of clomipramine and fluoxetine in the treatment of obsessive-compulsive disorder: behavior and biological results. Arch Gen Psychiatry. 1990; 47:926-32. https://pubmed.ncbi.nlm.nih.gov/2222131
218. Altemus M, Swedo SE, Leonard HL et al. Changes in cerebrospinal fluid neurochemistry during treatment of obsessive-compulsive disorder with clomipramine. Arch Gen Psychiatry. 1994; 51:794-803. https://pubmed.ncbi.nlm.nih.gov/7524463
219. Swedo SE, Leonard HL, Kruesi MJP et al. Cerebrospinal fluid neurochemistry in children and adolescents with obsessive-compulsive disorder. Arch Gen Psychiatry. 1992; 49:29-36. https://pubmed.ncbi.nlm.nih.gov/1370197
220. Asberg M, Ringberger V, Sjoqvist F, et al Monoamine metabolites in cerebrospinal fluid and serotonin uptake inhibition during treatment with chlorimipramine. Clin Pharmacol Ther. 1977; 21:201-7. (IDIS 92830)
221. Bertilsson L Asberg M, Thoren P. Differntial effect of chlorimipramine and nortriptyline on cerebrospinal fluid metabolites of serotonin and noradrenaline in depression. Eur J Clin Pharmaol. 1974; 7:365-8.
222. Leonard HL, Meyer MC, Swedo SE et al. Electrocardiographic changes during desipramine and clomipramine treatment in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1995; 34:1460-8. https://pubmed.ncbi.nlm.nih.gov/8543513
223. Golden RN, Hsiao J, Lane E et al. The effects of intravenous clomipramine on neurohormones in normal subjects. J Clin Endocrinol Metab. 1989; 68:632-7. https://pubmed.ncbi.nlm.nih.gov/2537340
224. Golden RN, Ekstrom D, Brown TM et al. Neuroendocrine effects of intravenous clomipramine in depressed patients and healthy subjects. Am J Psychiatry. 1992; 149:1168-75. https://pubmed.ncbi.nlm.nih.gov/1323933
225. Ackerman DL, Greenland S, Bystritsky A et al. Relationship between early side effects and therapeutic effects of clomipramine therapy in obsessive- compulsive disorder. J Clin Psychopharmcol. 1996; 16:324-8.
226. Sanchez LE, Campbell M, Small AM et al. A pilot study of clomipramine in young autistic children. J Am Acad Child Adolesc Psychiatry. 1996; 35:537-44. https://pubmed.ncbi.nlm.nih.gov/8919717
227. Pers C, Kristiansen JE, Jonsson V et al. Rothia dentocariosa septicaemia in a patient with chronic lymphocytic leukaemia and toxic granulocytopenia. Dan Med Bull. 1987; 34:322-3. https://pubmed.ncbi.nlm.nih.gov/3436159
228. Piccinelli M, Pini S, Bellantuono C et al. Efficacy of drug treatment in obsessive-compulsive disorder: a meta-analytic review. Br J Psychiatry. 1995; 166:424-43. https://pubmed.ncbi.nlm.nih.gov/7795913
229. Crisp AH, Lacey JH, Crutchfield M. Clomipramine and drive in people with anorexia nervosa: an in-patient study. Br J Psychiatry. 1987; 150:355-8. https://pubmed.ncbi.nlm.nih.gov/3664105
230. Lacey JH, Crisp AH. Hunger, food intake and weight: the impact of clomipramine on a refeeding anorexia nervosa population. Postgrad Med J. 1980; 56(Suppl 1):79-85. https://pubmed.ncbi.nlm.nih.gov/6994086
231. Fava M, Copeland PM, Schweiger U et al. Neurochemical abnormalities of anorexia nervosa and bulimia nervosa. Am J Psychiatry. 1989; 146:963-71. https://pubmed.ncbi.nlm.nih.gov/2568763
232. Segraves RT. Reversing anorgasmia associated with serotonin uptake inhibitors. JAMA. 1991; 266:2279. https://pubmed.ncbi.nlm.nih.gov/1920732
233. Hollander E, McCarley A. Yohibine treatment of sexual side effects induced by serotonin reuptake blockers. JClin Psychiatry. 1992; 53:207-9.
234. Kennedy SH, Goldbloom DS. Current Perspectives on drug therapies for anorexia nervosa and bulimia nervosa. Drugs. 1991; 41:367-77. https://pubmed.ncbi.nlm.nih.gov/1711444
235. Baldessarini RJ. Drugs and the treatment of psychiatric disorders: depression and mania. In: Hardman JG, Limbird LE, Molinoff PB et al, eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 9th ed. New York: McGraw-Hill; 1995:431-59.
236. Furlanut M, Benetello P, Spina E. Pharmacokinetic optimisation of tricyclic antidepressant therapy. Clin Pharmacokinet. 1993; 24:301-18. https://pubmed.ncbi.nlm.nih.gov/8491058
237. Harper G. Suicidality with clomipramine. J Am Acad Child Adolesc Psychiatry. 1992; 31:369-70. https://pubmed.ncbi.nlm.nih.gov/1564041
238. Alarcon RD, Johnson BR, Lucas JP. Paranoid and aggressive behavior in two obsessive-compulsive adolescents treated with clomipramine. J Am Acad Child Adolesc Psychiatry. 1991; 30:999-1002. https://pubmed.ncbi.nlm.nih.gov/1757451
239. Ljunggren B, Bojs G. A case of photosensitivity and contact allergy to systemic tricyclic drugs, with unusual features. Contact Dermatitis. 1991; 24:259-65. https://pubmed.ncbi.nlm.nih.gov/1831106
240. Clayton AH. Antidepressant-induced tardive dyskinesia: review and case report. Psychopharmacol Bull. 1995; 31:259-64. https://pubmed.ncbi.nlm.nih.gov/7491377
241. Lejoyeux M, Rouillon F, Ades J. Prospective evaluation of the serotonin syndrome in depressed inpatients treated with clomipramine. Acta Psychiatr Scand. 1993; 88:369-71. https://pubmed.ncbi.nlm.nih.gov/8296581
242. DeVeaugh-Geiss J, Moroz G, Biederman J et al. Clomipramine hydrochloride in childhood and adolescent obsessive-compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry. 1992; 31:45-9. https://pubmed.ncbi.nlm.nih.gov/1537780
243. Berlin I, Cournot A, Zimmer R et al. Evaluation and comparison of the interaction between alcohol and moclobemide or clomipramine in healthy subjects. Psychopharmacology. 1990; 100:40-5. https://pubmed.ncbi.nlm.nih.gov/2296627
244. Allen D, Curran HV, Lader M. The effects of repeated doses of clomipramine and alprazolam on physiological, psychomotor and cognitive functions in normal subjects. Eur J Clin Pharmacol. 1991; 40:355-62. https://pubmed.ncbi.nlm.nih.gov/2050170
245. Ananth J, Pecknold JC, Van Den Steen N et al. Double-blind comparative study of clomipramine and amitriptyline in obsesive neurosis. Prog Neuropsychopharmacol. 1981; 5:257-62. https://pubmed.ncbi.nlm.nih.gov/7022517
246. Capstick N. Clomipramine in the treatment of the true obsessional state: a report on four patients. Psychosomatics. 1975; 16:21-5. https://pubmed.ncbi.nlm.nih.gov/1178805
247. Volavka J, Neziroglu F, Yaryura-Tobias JA. Clomipramine and imipramine in obsessive-compulsive disorder. Psychiatry Res. 1985; 14:85- 93. https://pubmed.ncbi.nlm.nih.gov/3887445
248. Waxman D. A general practitioner investigation on the use of clomipramine (Anafranil) in obsessional and phobic disorders: an interim report. J Int Med Res. 1973; 1:417-20.
249. Ananth J, Solyom L, Bryntwick S et al. Chlorimipramine therapy for obsessive-compulsive neurosis. Am J Psychiatry. 1979; 136:700-1. https://pubmed.ncbi.nlm.nih.gov/434251
250. Wyndowe J, Solyom L, Ananth J. Anafranil in obsessive compulsive neurosis. Curr Ther Res. 1975; 18:611-7. https://pubmed.ncbi.nlm.nih.gov/812637
251. Yaryura-Tobias, Neziroglu F. The action of chlorimipramine in obsessive-compulsive neurosis: a pilot study. Curr Ther Res. 1975; 17:111- 6. https://pubmed.ncbi.nlm.nih.gov/806424
252. Leonard HL, Swedo SE, Rapoport JL et al. Treatment of obsessive-compulsive disorder with clomipramine and desipramine in children and adolescents: a double-blind crossover comparison. Arch Gen Psychiatry. 1989; 46:1088-92. https://pubmed.ncbi.nlm.nih.gov/2686576
253. Pato MT, Hill JL, Murphy DL. A clomipramine dosage reduction study in the course of long-term treament of obsessive-compulsive disorder patients. Psychopharmacol Bull. 1990; 26:211-4. https://pubmed.ncbi.nlm.nih.gov/2236458
254. Carney MWP, Black P. A preliminary investigation of monochlor- imipramine in the treatment of depression. Int J Neuropsychiatry. 1967; 3:179-81. https://pubmed.ncbi.nlm.nih.gov/6043631
255. Gore CP. Clomipramine (Anafrail), Tofranil (imipramine) and placebo: a comparative study in relation to electroconvulsive therapy. J Int Med Res. 1973; 1:347-51.
256. Hynes MV. A comparative clinical trial of oral clomipramine (Anafranil) against amitrityline. J Int Med Res. 1973; 1:338-42.
257. Manna V, Martucci N, Agnoli A. Double-blind controlled study on the clinical efficacy and safety of fluoxetine vs clomipramine in the treatment of major depressive disorders. Int Clin Psychopharmacol. 1989; 4(Suppl 1):81-8. https://pubmed.ncbi.nlm.nih.gov/2644342
258. Ropert R. Fluoxetine versus clomipramine in major depressive disorders. Int Clin Psychopharmacol. 1989; 4(Suppl 1):89-95. https://pubmed.ncbi.nlm.nih.gov/2644343
259. Wolfersdorf M, Binz U, Wendt G et al. Double-blind study of oxaprotiline versus clomipramine in the treatment of depressive inpatients. Neuropsychobiology. 1987; 17:41-8. https://pubmed.ncbi.nlm.nih.gov/3306439
260. Kornhaber A, Horwitz IM. A comparison of clomipramine and doxepin in neurotic depression. J Clin Psychiatry. 1984; 45:337-41. https://pubmed.ncbi.nlm.nih.gov/6378895
261. Sundblad C, Hedberg MA, Eriksson E. Clomipramine administered during the luteal phase reduces the symptoms of premenstrual syndrome: a placebo-controlled trial. Neuropsychopharmacology. 1993; 9:133-45. https://pubmed.ncbi.nlm.nih.gov/8216696
262. Sundblad C, Modigh K, Andersch B et al. Clomipramine effectively reduces premenstrual irritability and dysphoria: a placebo-controlled trial. Acta Psychiatr Scand. 1992; 85:39-47. https://pubmed.ncbi.nlm.nih.gov/1546547
263. Eriksson E, Lisjo P, Sundblad C et al. Effect of clomipramine on premenstrual syndrome. Acta Psychiatr Scand. 1990; 81:87-8. https://pubmed.ncbi.nlm.nih.gov/2330836
264. Moline ML. Pharmacologic strategies for managing premenstrual syndrome. Clin Pharm. 1993; 12:181-96. https://pubmed.ncbi.nlm.nih.gov/8491076
265. Allen JE. Drug-induced photosensitivity. Clin Pharm. 1993; 12:580-7. https://pubmed.ncbi.nlm.nih.gov/8222522
266. Dale O, Hole A. Biphasic time-course of serum concentrations of clomipramine and desmethylclomipramine after a near-fatal overdose. Vet Hum Toxicol. 1994; 36:309-10. https://pubmed.ncbi.nlm.nih.gov/7975135
267. Linnoila M, Seppala T, Mattila MJ et al. Clomipramine and doxepin in depressive neurosis: plasma levels and therapeutic response. Arch Gen Psychiatry. 1980; 37:1295-9. https://pubmed.ncbi.nlm.nih.gov/7436691
268. Harrison W, Stewart J, McGrath PJ et al. Unusual side effects of clomipramine associated with yawning. Can J Psychiatry. 1984; 29:546. https://pubmed.ncbi.nlm.nih.gov/6541521
269. Murphy M. Down-regulation of post-synaptic serotonin receptors as a mechanism for clomipramine-induced anorgasmia. Br J Psychiatry. 1987; 151:704. https://pubmed.ncbi.nlm.nih.gov/3446321
270. Beaumont G. Sexual side-effects of clomipramine (Anafranil). J Int Med Res. 1977; 5(Suppl 1):37-44. https://pubmed.ncbi.nlm.nih.gov/863089
271. Zohar J, Zohar-Kadouch RC, Kindler S. Current concepts in the pharmacological treatment of obsessive-compulsive disorder. Drugs. 1992; 43:210-8. https://pubmed.ncbi.nlm.nih.gov/1372219
272. Ciba Geigy Limited, Pharmaceuticals Division. Anafranil (clomipramine hydrochloride) capsules brief prescribing information. In: MIMS Middle East. Surrey, UK: A.E. Morgan Publications Ltd.; 1996:86.
273. Haensel SM, Rowland DL, Kallan KT. Clomipramine and sexual function in men with premature ejaculation and controls. J Urol. 1996; 156:1310-5. https://pubmed.ncbi.nlm.nih.gov/8808861
274. Balon R. Antidepressants in the treatment of premature ejaculation. J Sex Marital Ther. 1996; 22:85-96. https://pubmed.ncbi.nlm.nih.gov/8743620
275. Montorsi F, Guazzoni G, Trimboli F et al. Clomipramine for premature ejaculation: a randomized, double-blind, placebo controlled study. Acta Urol Ital. 1995; 9:5-6.
276. Ananth J, Pecknold JC, van der Steen N et al. Double-blind comparison study of chlorimipramine in obsessive neurosis. Curr Ther Res. 1979; 25:703-9.
277. Arfwidsson L, D Elia G, Laurell B et al. Comparison of chlorimipramine and imipramine in ambulatory treatment of depression. Acta Psychiatr Scand. 1972; 48:367-76. https://pubmed.ncbi.nlm.nih.gov/4571649
278. Cattiez PH, Dierick M, Troisfontaines B et al. Moclobemide (Ro 11- 1163) vs. clomipramine in the treatment of depression: a double-blind multicenter study in Belgium. Drug Develop Res. 1990; 21:325-331.
279. Chen CN. The use of clomipramine as an REM sleep suppressant in narcolepsy. Postgrad Med J. 1980; 56(Suppl. 1):86-9. https://pubmed.ncbi.nlm.nih.gov/7393833
280. Lipsedge MS, Prothero W. Clonidine and clomipramine in obsessive- compulsive disorder. Am J Psychiatry. 1987; 144:965-6. https://pubmed.ncbi.nlm.nih.gov/3605413
281. Golden RN, Morris JE, Sack DA. Combined lithium-tricyclic treatment of obsessive-compulsive disorder. Biol Psychiatry. 1988; 23:181-5. https://pubmed.ncbi.nlm.nih.gov/3334887
282. Guillbert E, Pelicier Y, Archambault JC et al. A double-blind, multicenter study of paroxetine versus clomipramine in depressed elderly patients. Acta Psychiatr Scand. 1989; 350(Suppl.):132-4.
283. Ginestet D and the Multicenter Study. Fluoxetine in endogenous depression and melancholia versus clomipramine. Int Clin Psychopharmacol. 1989; 4(Suppl. 1): 37-40.
284. Gostik N, Beaumont G, Grieve A. Clomipramine and smoking: an interaction study- clinical findings. J Int Med Res. 1980; 8(Suppl. 3):85-7. https://pubmed.ncbi.nlm.nih.gov/7202823
285. Brasic JR, Barnett JY, Kaplan D et al. Clomipramine ameliorates adventitious movements and compulsions in prepubertal boys with autistic disorder and severe mental retardation. Neurology. 1994; 44:1309-12. https://pubmed.ncbi.nlm.nih.gov/8035936
286. McDougle CJ, Price LH, Volkmar FR et al. Clomipramine in autism: preliminary evidence of efficacy. J Am Acad Child Adolesc Psychiatry. 1992; 31:746-50. https://pubmed.ncbi.nlm.nih.gov/1644740
287. Segraves RT, Saran A, Segraves K et al. Clomipramine versus placebo in the treatment of premature ejaculation: a pilot study. J Sex Marital Ther. 1993; 19:198-200. https://pubmed.ncbi.nlm.nih.gov/8246275
288. American Psychiatric Association. American Psychiatric Association Practice Guidelines. 1st ed. Washington, D.C.: American Psychiatric Association; 1996:52-53,96-102,110-111.
289. Carpenter LL, McDougle CJ, Epperson CN et al. A risk-benefit assessment of drugs used in the management of obsessive-compulsive disorder. Drug Saf. 1996; 15:116-34. https://pubmed.ncbi.nlm.nih.gov/8884163
290. Pigott TA. OCD: where the serotonin selectivity story begins. J Clin Psychiatry. 1996; 57(Suppl. 6):11-20. https://pubmed.ncbi.nlm.nih.gov/8647793
291. Harris MG, Benfield P. Fluoxetine: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in older patients with depressive illness. Drugs Aging. 1995; 6:64-84. https://pubmed.ncbi.nlm.nih.gov/7696780
292. DeVeaugh-Geiss J. Pharmacologic therapy of obsessive compulsive disorder. Adv Pharmacol. 1994; 30:35-52. https://pubmed.ncbi.nlm.nih.gov/7833296
293. Dominguez RA, Mestre SM. Management of treatment-refractory obsessive compulsive disorder patients. J Clin Psychiatry. 1994; 55(Suppl.):86-92. https://pubmed.ncbi.nlm.nih.gov/7961537
294. Francois B, Marquet P, Desachy A et al. Serotonin syndrome due to an overdose of moclobemide and clomipramine: a potentially life-threatening association. Intensive Care Med. 1997; 23:122-4. https://pubmed.ncbi.nlm.nih.gov/9037653
295. Rihmer Z, Barsi J, Belso N et al. Antidepressant-induced hypomania in obsessive-compulsive disorder. Int Clin Psychopharmacol. 1996; 11(Suppl. 5):203-5. https://pubmed.ncbi.nlm.nih.gov/8923100
296. Montgomery SA. Long-term management of obsessive-compulsive disorder. Int Clin Psychopharmacol. 1996; 11(Suppl. 5):23-9. https://pubmed.ncbi.nlm.nih.gov/9032001
297. Fineberg N. Refining treatment approaches in obsessive-compulsive disorder. Int Clin Psychopharmacol. 1996; 11(Suppl. 5):13-22. https://pubmed.ncbi.nlm.nih.gov/9032000
298. DeToledo JC, Haddad H, Ramsay RE. Status epilepticus associated with the combination of valproic acid and clomipramine. Ther Drug Monit. 1997; 19:1-10. https://pubmed.ncbi.nlm.nih.gov/9029739
299. Mundo E, Bareggi SR, Pirola R et al. Long-term pharmacotherapy of obsessive-compulsive disorder: a double-blind controlled study. J Clin Psychopharmacol. 1997; 17:4-10. https://pubmed.ncbi.nlm.nih.gov/9004050
300. Lopez-Ibor JJ Jr, Saiz J, Cottraux J et al. Double-blind comparison of fluoxetine versus clomipramine in the treatment of obsessive compulsive disorder. Eur Neuropsychopharmacol. 1996; 6:111-8. https://pubmed.ncbi.nlm.nih.gov/8791036
301. Coupland NJ, Bell CJ, Potokar JP. Serotonin reuptake inhibitor withdrawal. J Clin Psychopharmacol. 1996; 16:356-62. https://pubmed.ncbi.nlm.nih.gov/8889907
302. Nierenberg DW, Semprebon M. The central nervous system serotonin syndrome. Clin Pharmacol Ther. 1993; 53:84-8. https://pubmed.ncbi.nlm.nih.gov/8257462
303. Mills KC. Serotonin syndrome. Am Fam Physician. 1995; 52:1475-82. https://pubmed.ncbi.nlm.nih.gov/7572570
304. Reynolds RD. Serotonin syndrome: what family physicians need to know. Am Fam Physician. 1995; 52:1263-71. https://pubmed.ncbi.nlm.nih.gov/7572545
305. Lappin RI, Auchincloss EL. Treatment of the serotonin syndrome with cyproheptadine. N Engl J Med. 1994; 331:1021-2. https://pubmed.ncbi.nlm.nih.gov/8084345
306. Sporer KA. The serotonin syndrome: implicated drugs, pathophysiology and management. Drug Safety. 1995; 13:94-104. https://pubmed.ncbi.nlm.nih.gov/7576268
307. Brodribb TR, Downey M, Gilbar PJ. Efficacy and adverse effects of moclobemide. Lancet. 1994; 343:475. https://pubmed.ncbi.nlm.nih.gov/7905962
308. Somerset Pharmaceuticals. Eldepryl (selegiline) tablets prescribing inforamtion (dated 1994 Sep). In: Physician s desk reference. 49th ed. Montvale, NJ: Medical Economics Company, Inc; 1995(Suppl. A):A157-8.
309. Bhatara VS, Bandettini FC. Possible interaction between sertraline and tranylcypromine. Clin Pharm. 1993; 12:222-5. https://pubmed.ncbi.nlm.nih.gov/8491079
310. American Psychiatric Association. DSM-IV™: diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994:417-23.
311. Benfield P, Heel RC, Lewis SP. Fluoxetine: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in depressive illness. Drugs. 1986; 32:481-508. https://pubmed.ncbi.nlm.nih.gov/2878798
312. Sommi RW, Crismon ML, Bowden CL. Fluoxetine: a serotonin-specific, second-generation antidepressant. Pharmacotherapy. 1987; 7:1-15. https://pubmed.ncbi.nlm.nih.gov/3554156
313. Fuller RW, Wong DT. Serotonin reuptake blockers in vitro and in vivo. J Clin Psychopharmacol. 1987; 7(Suppl):36-43S.
314. Sulser F. Mode of action of antidepressant drugs. J Clin Psychiatry. 1983; 44:14-20. https://pubmed.ncbi.nlm.nih.gov/6406444
315. Mishra R, Janowsky A, Sulser F. Subsensitivity of the norepinephrine receptor-coupled adenylate cyclase system in brain: effects of nisoxetine versus fluoxetine. Eur J Pharmacol. 1979; 60:379-82. https://pubmed.ncbi.nlm.nih.gov/316774
316. Charney DS, Menkes DB, Heninger GR. Receptor sensitivity and the mechanism of action of antidepressant treatment: implications for the etiology and therapy of depression. Arch Gen Psychiatry. 1981; 38:1160-80. https://pubmed.ncbi.nlm.nih.gov/6271089
317. Banerjee SP, Kung LS, Riggi SJ et al. Development of β-adrenergic receptor subsensitivity by antidepressants. Nature. 1977; 268:455-6. https://pubmed.ncbi.nlm.nih.gov/197419
318. Bergstrom DA, Kellar KJ. Adrenergic and serotonergic receptor binding after chronic desmethylimipramine treatment. J Pharmacol Exp Ther. 1979; 209:256-61. https://pubmed.ncbi.nlm.nih.gov/220405
319. Wolfe BB, Harden TK, Sporn JR et al. Presynaptic modulation of beta adrenergic receptors in rat cerebral cortex after treatment with antidepressants. J Pharmacol Exp Ther. 1978; 207:446- 57. https://pubmed.ncbi.nlm.nih.gov/213556
320. Maggi A, U’Prichard DC, Enna SJ. Differential effects of antidepressant treatment on brain monoaminergic receptors. Eur J Pharmacol. 1980; 61:91-8. https://pubmed.ncbi.nlm.nih.gov/6101555
321. Enna SJ, Kendall DA. Interaction of antidepressants with brain neurotransmitter receptors. J Clin Psychopharmacol. 1981; 1(Suppl):12-6S.
322. Peroutka SJ, Snyder SH. Long-term antidepressant treatment decreases spiroperidol-labeled serotonin receptor binding. Science. 1980; 210:88-90. https://pubmed.ncbi.nlm.nih.gov/6251550
323. Kendall DA, Duman R, Slopis J et al. Influence of adrenocorticotropin hormone and yohimbine on antidepressant-induced declines in rat brain neurotransmitter receptor binding and function. J Pharmacol Exp Ther. 1982; 222:566-71. https://pubmed.ncbi.nlm.nih.gov/6286924
324. Peroutka SJ, Snyder SH. Regulation of serotonin2(5-HT2) receptors labeled with [3H] spiroperidol by chronic treatment with the antidepressant amitriptyline. J Pharmacol Exp Ther. 1980; 215:582-7. https://pubmed.ncbi.nlm.nih.gov/6255132
325. Fuller RW. Functional consequences of inhibiting serotonin uptake with fluoxetine in rats. In: Ho BT, Schoolar JC, Usdin E, eds. Serotonin in biological psychiatry. New York: Raven Press; 1982:219-28.
326. Wong DT, Bymaster FP, Horng JS et al. A new selective inhibitor for uptake of serotonin into synaptosomes of rat brain:3-(p-trifluoromethylphenoxy)-N-methyl-3-phenylprolylamine. J Pharmacol Exp Ther. 1975; 193:804-11. https://pubmed.ncbi.nlm.nih.gov/1151730
327. Wander TJ, Nelson A, Okazaki H et al. Antagonism by antidepressants of serotonin S1 and S2 receptors ofnormal human brain in vitro. Eur J Pharmacol. 1986;132:115-21.
328. Wong DT, Horng JS, Bymaster FP et al. A selective inhibitor of serotonin uptake: Lilly 110140,3-(p-trifluoromethylphenoxy)-N-methyl-3-phenylpropylamine. LifeSci. 1974; 15:471-9.
329. Fuller RW, Perry KW, Molloy BB. Effect of 3-(p-trifluoromethylphenoxy)-N-methyl-3-phenylpropylamine on the depletion of brain serotonin by 4-chloroamphetamine. JPharmacol Exp Ther. 1975; 193:796-803.
330. Fuller RW, Snoddy HD, Perry KW et al. Importance of durationof drug action in the antagonism of p-chloroamphetaminedepletion of brain serotonin—comparison of fluoxetine and chlorimipramine. Biochem Pharmacol. 1978; 27:193-8. https://pubmed.ncbi.nlm.nih.gov/623674
331. Westerink BHC, Lejeune B, Korf GE et al. On the significance of regional dopamine metabolism in the rat brain for the classification of centrally acting drugs. Eur J Pharmacol. 1977; 42:179.
332. Baxter LR, Phelps ME, Mazziotta JC et al. Local cerebral glucose metabolic rates in obsessive-compulsive disorder. Arch Gen Psychiatr. 1987; 44:211-8. https://pubmed.ncbi.nlm.nih.gov/3493749
333. Swedo SE, Schapiro MB, Grady CL et al. Cerebral glucose metabolism in childhood-onset obsessive-compulsive disorder. Am J Psychiatr. 1989; 46:518-23.
334. Baxter LR, Schwartz JM, Mazziota JC et al. Cerebral glucose metabolic rates in non-depressed patients with obsessive-compulsive disorder. Am J Psychiatr. 1988; 145:1560-3. https://pubmed.ncbi.nlm.nih.gov/3264118
335. Nordahl TE, Benkelfat C, Semple WE et al. Cerebral glucose metabolic rates in obsessive-compulsive disorder. Neuropsychopharmacology. 1989; 2:23-8. https://pubmed.ncbi.nlm.nih.gov/2803479
336. Hahan H, Ogren S. Effects of antidepressant drugs on different receptors in the brain. Eur J Pharmacol. 1981; 70:393-407. https://pubmed.ncbi.nlm.nih.gov/6262100
337. Delini-Stula A, Vassout A. Modulation of dopamine-mediated behavioral responses by antidepressants: effects of single and repeated treatment. Eur J Pharmacol. 1979; 58:443-51. https://pubmed.ncbi.nlm.nih.gov/574454
338. Chen CN. Sleep, depression and antidepressants. Br J Psychiatry. 1979; 135:385-402. https://pubmed.ncbi.nlm.nih.gov/231990
339. Faravelli C, Brat A, Marchetti G et al. Cardiac effects ofclomipramine treatment: ECG and left ventricular systolic time intervals. Neuropsychobiology. 1983; 9:113-8. https://pubmed.ncbi.nlm.nih.gov/6621851
340. Jones RB, Luscombe DK, Groom GV. Plasma prolactin concentrations in normal subjects and depressive patients following oral clomipramine. Postgrad Med J. 1977; 53(Suppl. 4):166-71. https://pubmed.ncbi.nlm.nih.gov/600893
341. Reviewer comments (personal observations).
342. Novartis, East Hanover, NJ: Personal communication.
343. Agency for Health Care Policy and Research. Management of cancer pain: clinical practice guideline. AHCPR publication No. 94-0592. Rockville, MD: Department of Health and Human Services; 1994 Mar.
344. Kloke M, Hoffken K, Olbrich H et al. Anti-depressants and anti- convulsants for the treatment of neuropathic pain syndromes in cancer patients. Onkologie. 1991; 14:400-3.
345. Abbott Laboratories. Tdx/TDxFLx tricyclic antidepressants assay. List No. 9681. (66-6424/R1). Abbott Park, IL; 1996 Feb.
346. Michalets EL. Update: clinically significant cytochrome P-450 drug interactions. Pharmacotherapy. 1998; 18:84-112. https://pubmed.ncbi.nlm.nih.gov/9469685
347. Ballenger JC, Davidson JRT, Lecrubier Y et al. Consensus statement on panic disorder from the International Consensus Group on Depresion and Anxiety. J Clin Psychiatry. 1998; 59(Suppl 8):47-54. https://pubmed.ncbi.nlm.nih.gov/9707162
348. Food and Drug Administration. Class suicidality labeling language for antidepressants. From the FDA website:. http://www.fda.gov/downloads/Drugs/DrugSafety/InformationbyDrugClass/UCM161641.pdf
349. Food and Drug Administration. Public health advisory: suicidality in children and adolescents being treated with antidepressant medications. Rockville, MD; 2004 Oct 15. From the FDA website:. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm161679.htm
350. Anon. FDA statement on recommendations of the psychopharmacologic drugs and pediatric advisory committees. Rockville, MD; 2004 Sep 16. From the FDA website:. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2004/ucm108352.htm
351. American Psychiatric Association (APA). APA responds to FDA’s new warning on antidepressants. Arlington, VA; 2004 Oct. 15. From the APA website:. http://www.psych.org/news_room/press_releases/04-55apaonfdablackboxwarning.pdf
352. American Academy of Child and Adolescent Psychiatry (AACAP). AACAP responds to the new FDA warnings on pediatric antidepressant medications. Washington, D.C; 2004 Oct 15. From the AACAP website:. http://www.aacap.org/cs/root/media/press_releases/2004_press_releases/aacap_responds_to_new_fda_warnings_on_pediatric_antidepressant_medication
353. American Academy of Pediatrics (AAP). Children, antidepressants and a black box warning. Washington, D.C; 2004 Oct. 15. From the AAP website:. http://www.aap.org/pressroom/aappr-pressreleases.htm
354. Food and Drug Administration. Medication guide: about using antidepressants in children or teenagers. Rockville, MD; 2005 Jan 16. From the FDA website:. http://www.fda.gov/downloads/Drugs/DrugSafety/InformationbyDrugClass/UCM161646.pdf
a. Mallinckrodt, Inc. Anafranil (clomipramine hydrochloride) prescribing information. Hazelwood, MO; 2001 Sept 5.
b. Volkmar F, Cook EH Jr, Pomeroy J et al for the American Academy of Child and Adolescent Psychiatry Working Group on Quality Issues. Practice parameters for the assessment and treatment of children, adolescents, and adults with autism and other pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry. 1999; 38(12 Suppl):32-54S.
c. AHFS drug information 2003. McEvoy GK, ed. Tricyclic antidepressants general statement. Bethesda, MD: American Society of Health-System Pharmacists; 2003:2161-9.
d. Food and Drug Administration. FDA news: FDA proposes new warnings about suicidal thinking, behavior in young adults who take antidepressant medications. Rockville, MD; 2007 May 2. From the FDA web site:. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108905.htm
e. Food and Drug Administration. Antidepressant use in children, adolescents, and adults: class revisions to product labeling. Rockville, MD; 2007 May 2. From the FDA web site:. http://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm096273.htm
f. Food and Drug Administration. Revisions to medication guide: antidepressant medicines, depression and other serious mental illnesses and suicidal thoughts or actions. Rockville, MD; 2007 May 2. From the FDA web site:. http://www.fda.gov/downloads/Drugs/DrugSafety/InformationbyDrugClass/ucm100211.pdf
g. Bridge JA, Iyengar S, Salary CB. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007; 297:1683-96. https://pubmed.ncbi.nlm.nih.gov/17440145
h. National Institutes of Health Office of Medical Applications of Research. NIH consensus statement: diagnosis and treatment of depression in late life. 1991; 9;1-27.
i. Reynolds CF. Treatment of depression in late life. Am J Med. 1994; 97(Suppl 6A):39-46S.
j. Stewart RB. Advances in pharmactherapy: depression in the elderly—issues and advances in treatment. J Clin Pharm Ther. 1993; 18:243-53. https://pubmed.ncbi.nlm.nih.gov/8227232
k. Bascara L. A double-blind study to compare the effectiveness and tolerability of paroxetine and amitriptyline in depressed patients. Acta Psychiatr Scand. 1989; 80(Suppl 350):141-2.
Related/similar drugs
Frequently asked questions
More about clomipramine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (318)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: tricyclic antidepressants
- Breastfeeding
- En español