Alosetron (Monograph)
Brand name: Lotronex
Drug class: Anti-inflammatory Agents
VA class: GA900
Chemical name: 2,3,4,5-Tetrahydro-5-methyl-2-[(5-methyl-1H-imidazol-4-yl)methyl]- 1H-pyrido[4,3-b]indol-1-one monohydrochloride
Molecular formula: C17H18N4O•HCl
CAS number: 122852-69-1
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for alosetron to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of alosetron and consists of the following: elements to assure safe use. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
- Serious GI Effects
-
Infrequent but serious adverse GI effects reported, including ischemic colitis and serious complications of constipation; in some cases, resulted in hospitalization, blood transfusion, surgery (e.g., colectomy) and/or death. (See Warnings under Cautions.)
-
Discontinue immediately and contact clinician if manifestations of constipation or ischemic colitis develop.
-
Do not resume alosetron in patients who develop ischemic colitis.
-
Contact clinician if constipation does not resolve after discontinuance of alosetron; if constipation resolves after discontinuance, resume therapy only on advice of clinician.
- Restricted Use
-
Voluntarily withdrawn from US market by manufacturer in November 2000 because of numerous reports of severe adverse effects, including ischemic colitis, severely obstructed or ruptured bowel, and death; FDA approved a supplemental New Drug Application (sNDA) for alosetron in June 2002, permitting remarketing under restricted conditions of use.
-
Approved only for severe diarrhea-predominant irritable bowel syndrome (IBS) in women with chronic symptoms who have not responded adequately to conventional therapy. (See Uses.)
Introduction
Selective serotonergic type 3 (5-HT3) receptor inhibitor; may modulate serotonin-sensitive GI processes.
Uses for Alosetron
Severe Diarrhea-predominant Irritable Bowel Syndrome in Women
Only for management of severe diarrhea-predominant IBS in women with chronic symptoms (generally lasting ≥6 months) who have had anatomic or biochemical GI abnormalities excluded and have not responded to conventional therapy. Diarrhea-predominant IBS is considered severe if accompanied by at least one of the following symptoms: frequent and severe abdominal pain and/or discomfort; frequent bowel urgency or fecal incontinence; or disability or restriction of daily activities.
Use restricted to patients for whom benefit-to-risk balance is considered to be most favorable. (See Boxed Warning.)
Efficacy in men not adequately demonstrated in clinical studies.
Alosetron Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.
If a dose is missed, skip dose and take next dose at regularly scheduled time. Do not take a double dose to make up for missed dose.
Dosage
Available as alosetron hydrochloride; dosage expressed in terms of alosetron.
Adults
Severe Diarrhea-predominant IBS in Women
Oral
Initially, 0.5 mg twice daily is recommended to minimize risk of constipation (although efficacy of this dosage has not been established in clinical studies).
If constipation occurs at a dosage of 0.5 mg twice daily, interrupt therapy until constipation resolves; may then reinitiate at a reduced dosage of 0.5 mg once daily. If constipation recurs, immediately discontinue therapy.
May continue on a dosage of 0.5 mg once or twice daily as maintenance therapy if dosage is well tolerated and IBS symptoms are adequately controlled. If patient tolerates, but does not respond adequately to the dosage after 4 weeks, may increase up to 1 mg twice daily. If adequate control of symptoms not achieved after 4 weeks on a dosage of 1 mg twice daily, discontinue therapy.
Discontinue immediately and permanently in patients who develop ischemic colitis. (See Ischemic Colitis under Cautions.)
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time. (See Hepatic Impairment under Cautions.)
Renal Impairment
No specific dosage recommendations at this time. (See Renal Impairment under Cautions.)
Geriatric Patients
No specific dosage recommendations at this time. (See Geriatric Use under Cautions.)
Cautions for Alosetron
Contraindications
-
Current constipation, history of chronic or severe constipation, or history of complications related to constipation.
-
History of intestinal obstruction, stricture, toxic megacolon, GI perforation, and/or adhesions.
-
History of ischemic colitis, impaired intestinal circulation, thrombophlebitis, or hypercoagulable state.
-
History of Crohn’s disease, ulcerative colitis, or diverticulitis.
-
History of severe hepatic impairment.
-
Concomitant use of fluvoxamine. (See Specific Drugs under Interactions.)
Warnings/Precautions
Warnings
Serious Complications of Constipation
Serious complications of constipation (e.g., obstruction, perforation, ileus, impaction, toxic megacolon, secondary bowel ischemia, death) reported infrequently. (See Boxed Warning.)
No dose-response relationship has been established; reported with dosages of 1 mg twice daily or less.
Geriatric or debilitated patients or those taking drugs that decrease GI motility may be at increased risk.
Discontinue immediately if constipation occurs. If constipation resolves, resume therapy only on the advice of clinician. (See Dosage under Dosage and Administration.)
Ischemic Colitis
Ischemic colitis reported infrequently; may be life-threatening. (See Boxed Warning.)
No dose-response relationship has been established; reported with dosages of 1 mg twice daily or less.
Discontinue immediately if symptoms of ischemic colitis (e.g., rectal bleeding, bloody diarrhea, new/worsening abdominal pain) occur. Promptly evaluate and perform appropriate diagnostic tests.
Do not resume therapy in patients who develop ischemic colitis. (See Contraindications under Cautions.)
Specific Populations
Pregnancy
Category B.
No adequate and well-controlled studies in pregnant women; no evidence of fetal harm demonstrated in animal studies. Use during pregnancy only if clearly needed.
Lactation
Distributed into milk in rats; not known whether distributed into milk in humans. Caution advised.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Not recommended in pediatric population because of risk of serious GI complications.
Geriatric Use
Geriatric patients may be at greater risk for complications of constipation. Exercise appropriate caution and follow-up.
Hepatic Impairment
Extensively metabolized in liver; increased exposure to alosetron and/or its metabolites likely in patients with hepatic impairment, which can increase risk of serious adverse effects.
Use with caution in patients with mild or moderate hepatic impairment; contraindicated in patients with severe hepatic impairment. (See Contraindications under Cautions and see Absorption: Special Populations, under Pharmacokinetics.)
Renal Impairment
Renal impairment not expected to affect clearance of alosetron. (See Elimination: Special Populations, under Pharmacokinetics.)
Not evaluated in patients with end-stage renal disease.
Common Adverse Effects
Constipation, abdominal discomfort or pain, nausea, GI discomfort or pain, abdominal distention, regurgitation and reflux, hemorrhoids.
In women with severe diarrhea-predominant IBS, diarrhea and flatulence also reported.
Drug Interactions
Metabolized by CYP isoenzymes, principally by CYP1A2, and to a lesser extent by CYP3A4 and 2C9.
Inhibits CYP1A2 and CYP2E1 in vitro at very high concentrations (27-fold higher than peak plasma concentrations observed with 1-mg dose); in vivo, inhibits CYP1A2, but no effect on CYP2E1. Inhibits N-acetyltransferase in vivo. Does not inhibit CYP2C9, C19, 2E1, or 3A4.
Does not appear to induce CYP3A, 2E1, or 2C19.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potential pharmacokinetic interaction (altered alosetron clearance) when used concomitantly with drugs that inhibit or induce CYP1A2, 3A4, or 2C9.
CYP1A2 inhibitors: Avoid concomitant use.
CYP3A4 inhibitors: Caution advised when used concomitantly.
Potential to inhibit clearance of drugs metabolized by CYP1A2. Unlikely to inhibit clearance of drugs metabolized by CYP2C9, 2C19, 2E1, or 3A4.
Drugs Metabolized by N-Acetyltransferase
Potential pharmacokinetic interaction (decreased metabolism of drugs metabolized via N-acetyltransferase).
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antifungals, azoles (itraconazole, ketoconazole, voriconazole) |
Possible increased plasma alosetron concentrations Ketoconazole: Increased systemic exposure of alosetron by 29% |
Use concomitantly with caution |
|
Cimetidine |
Possible increased plasma alosetron concentrations |
Concomitant use not recommended unless clinically required |
|
Cisapride |
No substantial effect on cisapride metabolism or QT interval |
|
|
Fluvoxamine |
Increased plasma concentrations and half-life of alosetron by approximately sixfold and threefold, respectively |
Concomitant use contraindicated |
|
Hormonal contraceptives, oral (ethinyl estradiol, levonorgestrel) |
No clinically important effect on plasma contraceptive concentration |
|
|
Hydralazine |
Possible increased concentrations of hydralazine via N-acetyltransferase inhibition |
|
|
Isoniazid |
Possible increased concentrations of isoniazid via N-acetyltransferase inhibition |
|
|
Macrolides (clarithromycin, telithromycin) |
Possible increased plasma alosetron concentrations |
Use concomitantly with caution |
|
Procainamide |
Possible increased concentrations of procainamide via N-acetyltransferase inhibition |
|
|
Protease inhibitors |
Possible increased plasma alosetron concentrations |
Use concomitantly with caution |
|
Quinolone anti-infectives |
Possible increased plasma alosetron concentrations |
Concomitant use not recommended unless clinically required |
|
Theophylline |
Potential inhibition of theophylline metabolism; however, no clinically important effect observed in one study |
Alosetron Pharmacokinetics
Absorption
Bioavailability
About 50–60%.
Food
25% decrease in absorption; 15 minute delay in reaching peak plasma concentration.
Special Populations
In some studies in geriatric adults, about 40% increase in plasma concentrations observed.
In one female with severe hepatic impairment, exposure to alosetron following administration of a single 1-mg dose was approximately 14-fold higher than that reported in healthy individuals. In another female with moderate hepatic impairment, exposure to alosetron was increased by 1.6-fold.
Distribution
Plasma Protein Binding
82%.
Elimination
Metabolism
Extensively metabolized in liver to several metabolites. Circulating metabolites are present in low concentrations (≤15% of unchanged alosetron), and therefore not likely to contribute to pharmacologic activity of the drug.
Elimination Route
Excreted principally in urine (74%), mainly as metabolites, and in feces (11%). Also excreted as unchanged drug in urine (13%) and feces (1%).
Half-life
About 1.5 hours.
Special Populations
Renal impairment (Clcr 4–56 mL/minute) has no effect on renal elimination of alosetron. Effects on metabolite pharmacokinetics not studied in patients with renal impairment.
Stability
Storage
Oral
Tablets
20–25°C; protect from light and moisture.
Actions
-
Inhibition of enteric neuronal, peripheral, and CNS serotonergic type 3 (5-HT3) receptors may modulate serotonin-sensitive GI processes (visceral pain, colonic transit, and GI secretion) related to the pathophysiology of IBS.
Advice to Patients
-
Importance of patients reading the manufacturer’s patient information (medication guide) prior to starting therapy and each time the prescription is refilled.
-
Importance of not starting alosetron if constipated.
-
Importance of immediately discontinuing alosetron and informing clinician if constipation occurs or does not resolve after discontinuance.
-
Importance of resuming alosetron only if constipation is resolved and clinician treating IBS agrees.
-
Importance of immediately discontinuing alosetron and informing clinician if signs or symptoms of acute ischemic colitis (e.g., blood in stools, bloody diarrhea, new or worsening abdominal pain) occur.
-
Importance of not resuming alosetron if ischemic colitis has occurred.
-
Importance of discontinuing alosetron and consulting clinician if IBS symptoms are not adequately controlled after 4 weeks of taking 1 mg twice daily.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., hepatic disease).
-
Importance of informing patients of other precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
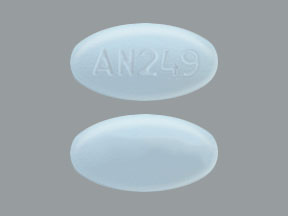
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
0.5 mg (of alosetron)* |
Alosetron Hydrochloride Tablets |
|
|
Lotronex |
Prometheus |
|||
|
1 mg (of alosetron)* |
Alosetron Hydrochloride Tablets |
|||
|
Lotronex |
Prometheus |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 5, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about alosetron
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (34)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: serotoninergic neuroenteric modulators
- Breastfeeding
- En español