Pioglitazone Disease Interactions
There are 9 disease interactions with pioglitazone.
- CHF
- Type I diabetes
- Bladder cancer
- Edema
- Liver disease
- Macular edema
- Premenopausal anovulation
- Weight gain
- Anemia
Thiazolidinediones (applies to pioglitazone) CHF
Major Potential Hazard, Moderate plausibility. Applicable conditions: Congestive Heart Failure
The use of thiazolidinediones, alone or in combination with other antidiabetic agents, has been associated with fluid retention and new onset or exacerbation of heart failure. An increased risk of cardiovascular events (heart failure worsening; new or worsening edema; new or worsening dyspnea; increases in heart failure medication; myocardial infarction; angina; cardiovascular hospitalization and deaths) has been reported with rosiglitazone therapy in type II diabetic patients with New York Heart Association (NYHA) Class I or II congestive heart failure compared to placebo. Likewise, overnight hospitalization for CHF was observed in 9.9% of diabetic patients with NYHA Class II and III heart failure on pioglitazone compared to 4.7% of patients on glyburide. An increased incidence of cardiovascular adverse events including edema and cardiac failure has also been reported in patients receiving a thiazolidinedione in combination with insulin relative to insulin and placebo. Therapy with thiazolidinediones should be administered cautiously and initiated at the lowest recommended dosage in patients with congestive heart failure. Thiazolidinediones are contraindicated for the treatment of patients with NYHA Class III or IV cardiac status. Patients should be monitored for signs of worsening heart failure such as increased dyspnea, edema, and weight gain. Therapy should be discontinued if any deterioration in cardiac status occurs.
Thiazolidinediones (applies to pioglitazone) type I diabetes
Major Potential Hazard, Moderate plausibility. Applicable conditions: Diabetic Ketoacidosis, Diabetes Type 1
Thiazolidinediones exert their hypoglycemic effect only in the presence of insulin. Therefore, these agents should not be used in patients with type I diabetes or for the treatment of diabetic ketoacidosis.
Pioglitazone (applies to pioglitazone) bladder cancer
Moderate Potential Hazard, Moderate plausibility.
There are insufficient data to determine if pioglitazone has an effect on preexisting bladder tumors or if it can cause bladder cancer. However, the manufacturer does not recommend the use of pioglitazone in patients with active bladder cancer. In patients with history of bladder cancer the benefit of treatment versus the risk of cancer recurrence during treatment should be considered.
Thiazolidinediones (applies to pioglitazone) edema
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hypertension, Pleural Effusion, Pulmonary Edema, Fluid Retention
Thiazolidinediones can cause dose-related edema. Therapy with thiazolidinediones should be administered cautiously in patients at risk for congestive heart failure as well as those with fluid overload or other conditions that may be adversely affected by excess fluid such as hypertension. Patients should be monitored for signs and symptoms of heart failure such as dyspnea, swelling of legs or ankles, and weight gain.
Thiazolidinediones (applies to pioglitazone) liver disease
Moderate Potential Hazard, Moderate plausibility.
Initiation of rosiglitazone or pioglitazone therapy is not recommended in patients who exhibit clinical evidence of active liver disease or increased baseline serum transaminase levels (ALT exceeding 2.5 times upper limit of normal). Use of these agents is also not recommended in patients who have experienced jaundice during treatment with troglitazone. The use of troglitazone, another agent in the thiazolidinedione class, has been associated with clinically significant elevations in liver enzymes, reversible jaundice, and idiosyncratic hepatocellular injury including rare cases of liver failure, liver transplants, and death. Injury has occurred after both short- and long-term treatment. While these effects have not been associated with other thiazolidinediones in clinical trials, concerns exist because of their structural similarities. In addition, isolated cases of hepatitis and hepatic enzyme elevations to 3 or more times the upper limit of normal have been reported with both rosiglitazone and pioglitazone during postmarketing use. Rarely, these events have involved hepatic failure with and without fatal outcome, although causality has not been established. Until more safety data are available, patients who are prescribed thiazolidinedione therapy should have serum transaminase levels checked at baseline and periodically thereafter as clinically necessary. Mild to moderate elevations (ALT less than or equal to 2.5 times ULN) require cautious use with more frequent monitoring to determine if the elevations resolve or worsen. Patients who develop potential symptoms of hepatic injury such as unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, and dark urine should have liver enzymes checked. Therapy should be withdrawn if ALT is elevated and persists above 3 times ULN or if jaundice develops.
Thiazolidinediones (applies to pioglitazone) macular edema
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus, Diabetic Macular Edema
New onset or worsening diabetic macular edema with decreased visual acuity have been reported in postmarketing reports in some diabetic patients who were taking thiazolidinedione drugs. Some patients presented with blurred vision or decreased visual acuity, but some patients appear to have been diagnosed on routine ophthalmologic examination. Most patients had peripheral edema at the time macular edema was diagnosed. Some patients had improvement in their macular edema after discontinuation of their thiazolidinedione. Patients with diabetes should have regular eye exams by an ophthalmologist according to current standards of care. Additionally, any diabetic who reports any kind of visual symptom should be promptly referred to an ophthalmologist, regardless of the patient's underlying medications or other physical findings.
Thiazolidinediones (applies to pioglitazone) premenopausal anovulation
Moderate Potential Hazard, Moderate plausibility.
In premenopausal, anovulatory patients with insulin resistance, treatment with thiazolidinediones may result in resumption of ovulation. Due to improved insulin sensitivity, pregnancy can occur if adequate contraception is not used.
Thiazolidinediones (applies to pioglitazone) weight gain
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Obesity
Thiazolidinediones can cause dose-related weight gain, which may be undesirable in obese patients attempting to lose weight. The mechanism of weight gain is unclear but probably involves a combination of fluid retention and fat accumulation. In postmarketing experience with rosiglitazone, there have been reports of unusually rapid increases in weight, greater than those generally observed in clinical trials. Patients who experience such increases should be assessed for fluid retention and volume-related events such as excessive edema and congestive heart failure.
Thiazolidinediones (applies to pioglitazone) anemia
Minor Potential Hazard, Moderate plausibility.
Thiazolidinediones can cause slight decreases in hemoglobin and hematocrit. In clinical studies, hemoglobin levels were reduced primarily within the first 4 to 12 weeks of therapy but remained relatively constant thereafter. These changes may be related to increased plasma volume and have rarely been associated with any significant hematologic clinical effects. Nevertheless, caution may be advisable when thiazolidinediones are prescribed to patients with certain anemias.
Switch to professional interaction data
Pioglitazone drug interactions
There are 351 drug interactions with pioglitazone.
Pioglitazone alcohol/food interactions
There are 3 alcohol/food interactions with pioglitazone.
More about pioglitazone
- pioglitazone consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (54)
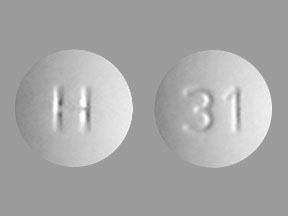
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thiazolidinediones
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.