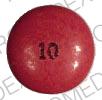
Mesoridazine Disease Interactions
There is 1 disease interaction with mesoridazine.
Atypical antipsychotic agents (applies to mesoridazine) dementia
Major Potential Hazard, High plausibility.
Antipsychotic drugs are not approved for the treatment of patients with dementia-related psychosis. Older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death; although the causes were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. A causal relationship with antipsychotic use has not been established. In controlled trials in older patients with dementia-related psychosis, patients randomized to risperidone, aripiprazole, and olanzapine had higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, compared to patients treated with placebo.
Switch to professional interaction data
Mesoridazine drug interactions
There are 703 drug interactions with mesoridazine.
Mesoridazine alcohol/food interactions
There is 1 alcohol/food interaction with mesoridazine.
More about mesoridazine
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: phenothiazine antipsychotics
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.