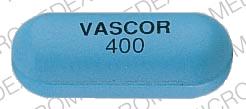
Vascor Disease Interactions
There are 8 disease interactions with Vascor (bepridil).
- Agranulocytosis
- Arrhythmias
- CHF
- Electrolyte imbalance/hypokalemia
- MI
- Bradyarrhythmia/AV block
- Cardiogenic shock/hypotension
- Liver disease
Bepridil (applies to Vascor) agranulocytosis
Major Potential Hazard, Low plausibility. Applicable conditions: Neutropenia
According to the manufacturer, there have been two cases of marked leukopenia and neutropenia reported in U.S. clinical trials of over 800 patients treated with bepridil for up to five years. Both involved diabetic and elderly patients, with one case resulting in death and the other recovering after discontinuation of the drug. In a postmarketing report, a 72-year-old man with severe angina pectoris developed fever and chills associated with an absolute neutrophil count of 35/mm3 six weeks after switching from diltiazem and nitrates to bepridil and nitrates. A bone marrow biopsy revealed profound myeloid hypoplasia. The patient recovered after discontinuation of bepridil and institution of granulocyte colony-stimulating factor and broad-spectrum antibiotics. Therapy with bepridil should be administered cautiously in patients with preexisting neutropenia or agranulocytosis. The drug should be withdrawn promptly if these conditions develop during therapy.
References (3)
- Singh BN (1991) "Comparative efficacy and safety of bepridil and diltiazem in chronic stable angina pectoris refractory to diltiazem. The Bepridil Collaborative Study Group." Am J Cardiol, 68, p. 306-12
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
- Weiss RJ (1993) "Bepridil and agranulocytosis." Am Heart J, 125, p. 1819-20
Bepridil (applies to Vascor) arrhythmias
Major Potential Hazard, High plausibility. Applicable conditions: Abnormal Electrocardiogram, Tachyarrhythmia
The use of bepridil is contraindicated in patients with a history of serious ventricular arrhythmias; patients with congenital or acquired QT interval prolongation syndromes; and patients treated concomitantly with class IA or III antiarrhythmic drugs or other medications that are known to produce increases in the QT interval or cause torsade de pointes. Bepridil has class I antiarrhythmic properties and can induce new arrhythmias, including ventricular tachycardia and ventricular fibrillation. Patients with other severe arrhythmias may have increased susceptibility to the proarrhythmic effects of bepridil, but use in such patients has been limited. Bepridil can also cause torsade de pointes type ventricular tachycardia secondary to its ability to prolong the QT interval. In U.S. clinical trials, the mean prolongations of QTc and QT were 8% and 10%, respectively, but increases of 25% or more occurred in 5% of the studied population for QTc and 8.7% for QT. Although the absolute safe upper limit of QT is not known, the manufacturer recommends that the dosage be reduced in patients whose QT interval exceeds 0.52 seconds during treatment. If prolongation remains excessive, the drug should be discontinued.
References (5)
- Singh BN (1992) "Bepridil therapy: guidelines for patient selection and monitoring of therapy." Am J Cardiol, 69, d79-85
- Coumel P (1992) "Safety of bepridil: from review of the European data." Am J Cardiol, 69, d75-8
- Singh BN (1992) "Safety profile of bepridil determined from clinical trials in chronic stable angina in the United States." Am J Cardiol, 69, d68-74
- Shapiro W (1992) "Comparative efficacy of bepridil versus placebo in angina pectoris: treatment and withdrawal studies." Am J Cardiol, 69, d43-9
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
Bepridil (applies to Vascor) CHF
Major Potential Hazard, High plausibility. Applicable conditions: Myocardial Infarction, Congestive Heart Failure
Bepridil may have a negative inotropic effect, particularly at high dosages. Congestive heart failure has been observed infrequently (approximately 1%) in U.S. controlled clinical trials. However, experience with the use of bepridil in the presence of significantly impaired ventricular function is limited, and there is little information on the effect of concomitant administration with digoxin. Therapy with bepridil should be administered cautiously in patients with congestive heart failure, especially if they have severe left ventricular dysfunction (e.g., ejection fraction < 30%) or if they are receiving a beta-adrenergic blocker. Likewise, bepridil should not be given to patients with acute myocardial infarction and pulmonary congestion documented by X-ray on admission, since associated heart failure may be acutely worsened. Mild symptoms of cardiac failure should be under control, if possible, prior to initiating bepridil therapy.
References (5)
- Singh BN (1992) "Bepridil therapy: guidelines for patient selection and monitoring of therapy." Am J Cardiol, 69, d79-85
- Coumel P (1992) "Safety of bepridil: from review of the European data." Am J Cardiol, 69, d75-8
- Singh BN (1992) "Safety profile of bepridil determined from clinical trials in chronic stable angina in the United States." Am J Cardiol, 69, d68-74
- Shapiro W (1992) "Comparative efficacy of bepridil versus placebo in angina pectoris: treatment and withdrawal studies." Am J Cardiol, 69, d43-9
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
Bepridil (applies to Vascor) electrolyte imbalance/hypokalemia
Major Potential Hazard, High plausibility. Applicable conditions: Electrolyte Abnormalities, Magnesium Imbalance, Diarrhea
Bepridil can cause torsade de pointes type ventricular tachycardia secondary to its ability to prolong the QT interval. In U.S. clinical trials, the mean prolongations of QTc and QT were 8% and 10%, respectively, but increases of 25% or more occurred in 5% of the studied population for QTc and 8.7% for QT. Electrolyte disturbances such as hypokalemia and hypomagnesemia may augment the prolongation effect of bepridil on the QT interval and should be corrected prior to institution of bepridil therapy. In addition, patients who experience frequent, severe, and/or prolonged diarrhea may be subject to electrolyte losses and should be followed closely and managed accordingly during therapy with bepridil.
References (5)
- Singh BN (1992) "Bepridil therapy: guidelines for patient selection and monitoring of therapy." Am J Cardiol, 69, d79-85
- Coumel P (1992) "Safety of bepridil: from review of the European data." Am J Cardiol, 69, d75-8
- Singh BN (1992) "Safety profile of bepridil determined from clinical trials in chronic stable angina in the United States." Am J Cardiol, 69, d68-74
- Shapiro W (1992) "Comparative efficacy of bepridil versus placebo in angina pectoris: treatment and withdrawal studies." Am J Cardiol, 69, d43-9
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
Bepridil (applies to Vascor) MI
Major Potential Hazard, High plausibility. Applicable conditions: Myocardial Infarction, Post MI Syndrome, History - Myocardial Infarction
Bepridil has class I antiarrhythmic properties and can induce new arrhythmias, including ventricular tachycardia and ventricular fibrillation. In the National Heart, Lung, and Blood Institute's Cardiac Arrhythmia Suppression Trial involving patients with asymptomatic, non-life-threatening ventricular arrhythmias who have had myocardial infarctions for less than two years previously, an excess rate of mortality/nonfatal cardiac arrest was seen in patients treated with the class I antiarrhythmic agents, encainide and flecainide, compared with that seen in patients assigned to matched placebo-treated groups. Although the applicability of these results to other antiarrhythmic agents is uncertain, the manufacturer recommends generally avoiding the use of bepridil in the post-infarction period. There is also limited experience in the use of bepridil within three months following a myocardial infarction, since it was one of the exclusion criteria in U.S. clinical trials.
References (1)
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
CCBs (applies to Vascor) bradyarrhythmia/AV block
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block, Sinus Node Dysfunction
The use of some calcium channel blockers (CCBs) is contraindicated in patients with severe bradyarrhythmia, sick sinus syndrome (unless a functioning pacemaker is present), or heart block greater than the first degree (unless a functioning pacemaker is present). CCBs like bepridil, diltiazem and verapamil have a negative effect on AV conduction and the SA node and may exacerbate these conditions.
References (14)
- Reams GP, Lau A, Messina C, et al. (1987) "Efficacy, electrocardiographic and renal effects of intravenous diltiazem for essential hypertension." Am J Cardiol, 60, i78-84
- Nagle RE, Low-Beer T, Horton R (1989) "Diltiazem and heart block." Lancet, Apr, p. 907
- Imamura T, Koiwaya Y, Nakamura M (1986) "Sinoatrial block induced by oral diltiazem." Clin Cardiol, 9, p. 33-4
- Woehler TR, Eff J, Graney W, et al. (1992) "Multicenter evaluation of the efficacy and safety of sustained-release diltiazem hydrochloride for the treatment of hypertension." Clin Ther, 14, p. 148-57
- Colombo G, Zucchella G, Planca E, Grieco A (1987) "Intravenous diltiazem in the treatment of unstable angina: a study of efficacy and tolerance." Clin Ther, 9, p. 536-47
- Aromatorio GJ, Uretsky BF, Reddy PS (1985) "Hypotension and sinus arrest with nifedipine in pulmonary hypertension." Chest, 87, p. 265-7
- Baky SH, Singh BN (1982) "Verapamil hydrochloride: pharmacological properties and role in cardiovascular therapeutics." Pharmacotherapy, 2, p. 328-50
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
- (2002) "Product Information. Cardizem (diltiazem)." Hoechst Marion Roussel
- (2001) "Product Information. Calan (verapamil)." Searle
- Andrivet P, Beaslay V, Kiger JP, Gnoc CV (1994) "Complete sinus arrest during diltiazem therapy - clinical correlates and efficacy of intravenous calcium." Eur Heart J, 15, p. 350-4
- Gobel EJAM, Hautvast RWM, Vangilst WH, Spanjaard JN, Hillege HL, Dejongste MJL, Molhoek GP, Lie KI (1995) "Randomised, double-blind trial of intravenous diltiazem versus glyceryl trinitrate for unstable angina pectoris." Lancet, 346, p. 1653-7
- (2001) "Product Information. Covera-HS (verapamil)." Searle
- Pahor M, Manto A, Pedone C, Carosella L, Guralnik JM, Carbonin P (1996) "Age and severe adverse drug reactions caused by nifedipine and verapamil." J Clin Epidemiol, 49, p. 921-8
CCBs (applies to Vascor) cardiogenic shock/hypotension
Major Potential Hazard, High plausibility.
In general, calcium channel blockers (CCBs) should not be used in patients with hypotension (systolic pressure < 90 mm Hg) or cardiogenic shock. Due to potential negative inotropic and peripheral vasodilating effects, the use of CCBs may further depress cardiac output and blood pressure, which can be detrimental in these patients. The use of verapamil and diltiazem is specifically contraindicated under these circumstances.
References (6)
- Stehle G, Buss J, Eibach J, et al. (1990) "Cardiogenic shock associated with verapamil in a patient with liver cirrhosis." Lancet, 336, p. 1079
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
- (2002) "Product Information. Cardizem (diltiazem)." Hoechst Marion Roussel
- (2001) "Product Information. Calan (verapamil)." Searle
- Kubota K, Pearce GL, Inman WHW (1995) "Vasodilation-related adverse events in diltiazem and dihydropyridine calcium antagonists studied by prescription-event monitoring." Eur J Clin Pharmacol, 48, p. 1-7
- Pahor M, Manto A, Pedone C, Carosella L, Guralnik JM, Carbonin P (1996) "Age and severe adverse drug reactions caused by nifedipine and verapamil." J Clin Epidemiol, 49, p. 921-8
CCBs (applies to Vascor) liver disease
Major Potential Hazard, High plausibility.
Calcium channel blockers (CCBs) are extensively metabolized by the liver. The half-lives of CCBs may be prolonged substantially in patients with severe hepatic impairment, with the potential for significant drug accumulation. In addition, the use of some CCBs has been associated with elevations in serum transaminases, both with and without concomitant elevations in alkaline phosphatase and bilirubin. While these effects may be transient and reversible, some patients have developed cholestasis or hepatocellular injury. Therapy with CCBs should be administered cautiously and often at reduced dosages in patients with significantly impaired hepatic function. Periodic monitoring of liver function is advised.
References (54)
- Echizen H, Eichelbaum M (1986) "Clinical pharmacokinetics of verapamil, nifedipine and diltiazem." Clin Pharmacokinet, 11, p. 425-49
- Saracheck NS, London RL, Matulewicz TJ, et al. (1985) "Diltiazem and granulomatous hepatitis." Gastroenterology, 88, p. 1260-2
- Shallcross H, Padley SP, Glynn MJ, Gibbs DD (1987) "Fatal renal and hepatic toxicity after treatment with diltiazem." Br Med J, 295, p. 1256-7
- Colombo G, Zucchella G, Planca E, Grieco A (1987) "Intravenous diltiazem in the treatment of unstable angina: a study of efficacy and tolerance." Clin Ther, 9, p. 536-47
- Toft E, Vyberg M, Therkelsen K (1991) "Diltiazem-induced granulomatous hepatitis." Histopathology, 18, p. 474-5
- Abramson M, Littlejohn GO (1985) "Hepatic reactions to nifedipine." Med J Aust, 142, p. 47-8
- Toner M, White A, Moriarty J, Clancy L (1988) "Allergic urticarial eruption, leukocytosis and abnormal liver function tests following nifedipine administration." Chest, 93, p. 1320-1
- Babany G, Uzzan F, Larrey D, et al. (1989) "Alcoholic-like liver lesions induced by nifedipine." J Hepatol, 9, p. 252-5
- Brodsky SJ, Cutler SS, Weiner DA, Klein MD (1981) "Hepatotoxicity due to treatment with verapamil." Ann Intern Med, 94, p. 490-1
- Somogyi A, Albrecht M, Kliems G, et al. (1981) "Pharmacokinetics, bioavailability and ECG response of verapamil in patients with liver cirrhosis." Br J Clin Pharmacol, 12, p. 51-60
- Woodcock BG, Rietbrock I, Vohringer HF, Rietbrock N (1981) "Verapamil disposition in liver disease and intensive-care patients: kinetics, clearance, and apparent blood flow relationships." Clin Pharmacol Ther, 29, p. 27-34
- Woodcock BG, Rietbrock N (1982) "Verapamil bioavailability and dosage in liver disease." Br J Clin Pharmacol, 13, p. 240-1
- Stern EH, Pitchon R, King BD, Wiener I (1982) "Possible hepatitis from verapamil." N Engl J Med, 306, p. 612-3
- Stehle G, Buss J, Eibach J, et al. (1990) "Cardiogenic shock associated with verapamil in a patient with liver cirrhosis." Lancet, 336, p. 1079
- Hare DL, Horowitz JD (1986) "Verapamil hepatotoxicity: a hypersensitivity reaction." Am Heart J, 111, p. 610-11
- Guarascio P, D'Amato C, Sette P, et al. (1984) "Liver damage from verapamil." Br Med J, 288, p. 362-3
- Dow RJ, Graham DJM (1986) "A reveiw of the human metabolism and pharmacokinetics of nicardipine hydrochloride." Br J Clin Pharmacol, 22, s195-202
- McAllister RG Jr, Hamann SR, Blouin RA (1985) "Pharmacokinetics of calcium-entry blockers." Am J Cardiol, 55, b30-40
- Kates RE (1983) "Calcium antagonists: pharmacokinetic properties." Drugs, 25, p. 113-24
- Finucci GF, Padrini R, Piovan D, et al. (1988) "Verapamil pharmacokinetics and liver function in patients with cirrhosis." Int J Clin Pharmacol Res, 8, p. 123-6
- Giacomini KM, Massoud N, Wong FM, Giacomini JC (1984) "Decreased binding of verapamil to plasma proteins in patients with liver disease." J Cardiovasc Pharmacol, 6, p. 924-8
- Razak TA, McNeil JJ, Sewell RB, Drummer OH, Smallwood RA, Conway EL, Louis WJ (1990) "The effect of hepatic cirrhosis on the pharmacokinetics and blood pressure response to nicardipine." Clin Pharmacol Ther, 47, p. 463-9
- Rush WR, Alexander O, Hall DJ, Cairncross L, Dow RJ, Graham DJ (1986) "The metabolism of nicardipine hydrochloride in healthy male volunteers." Xenobiotica, 16, p. 341-9
- Benet LZ (1985) "Pharmacokinetics and metabolism of bepridil." Am J Cardiol, 55, c8-13
- Kurosawa S, Kurosawa N, Owada E, et al. (1990) "Pharmacokinetics of diltiazem in patients with liver cirrhosis." Int J Clin Pharmacol Res, 10, p. 311-8
- Elliott HL, Meredith PA (1991) "The clinical consequences of the absorption, distribution, metabolism and excretion of amlodipine." Postgrad Med J, 67, s20-3
- Stopher DA, Beresford AP, Macrae PV, Humphrey MJ (1988) "The metabolism and pharmacokinetics of amlodipine in humans and animals." J Cardiovasc Pharmacol, 12, s55-9
- Kleinbloesem CH, van Harten J, Wilson JP, et al. (1986) "Nifedipine: kinetics and hemodynamic effects in patients with liver cirrhosis after intravenous and oral administration." Clin Pharmacol Ther, 40, p. 21-8
- Raemsch KD, Sommer J (1983) "Pharmacokinetics and metabolism of nifedipine." Hypertension, 5, p. 18-24
- Ramsch KD, Graefe KH, Scherling D, et al. (1986) "Pharmacokinetics and metabolism of calcium-blocking agents nifedipine, nitrendipine, and nimodipine." Am J Nephrol, 6, p. 73-80
- Challenor VF, Waller DG, Renwick AG, et al. (1987) "The trans-hepatic extraction of nifedipine." Br J Clin Pharmacol, 24, p. 473-7
- Dunselman PH, Edgar B (1991) "Felodipine clinical pharmacokinetics." Clin Pharmacokinet, 21, p. 418-30
- Regardh CG, Edgar B, Olsson R, Kendall M, Collste P, Shansky C (1989) "Pharmacokinetics of felodipine in patients with liver disease." Eur J Clin Pharmacol, 36, p. 473-9
- Cotting J, Reichen J, Kutz K, Laplanche R, Nuesch E (1990) "Pharmacokinetics of isradipine in patients with chronic liver disease." Eur J Clin Pharmacol, 38, p. 599-603
- Tse FL, Jaffe JM (1987) "Pharmacokinetics of PN 200-110 (isradipine), a new calcium antagonist, after oral administration in man." Eur J Clin Pharmacol, 32, p. 361-5
- Graham D, Dow R, Hall D, Alexander O, Mroszczak E, Freedman A (1985) "The metabolism and pharmacokinetics of nicardipine hydrochloride in man." Br J Clin Pharmacol, 20, s23-8
- Gengo FM, Fagan SC, Krol G, Bernhard H (1987) "Nimodipine disposition and haemodynamic effects in patients with cirrhosis and age-matched controls." Br J Clin Pharmacol, 23, p. 47-53
- Meredith P, Elliott H (1992) "Clinical pharmacokinetics of amlodipine." Clin Pharmacokinet, 22, p. 22-31
- (2002) "Product Information. Norvasc (amlodipine)." Pfizer U.S. Pharmaceuticals
- (2002) "Product Information. Vascor (bepridil)." McNeil Pharmaceutical
- (2002) "Product Information. Cardizem (diltiazem)." Hoechst Marion Roussel
- (2002) "Product Information. Plendil (felodipine)." Merck & Co., Inc
- (2002) "Product Information. Cardene (nicardipine)." Syntex Laboratories Inc
- (2002) "Product Information. Procardia (nifedipine)." Pfizer U.S. Pharmaceuticals
- (2002) "Product Information. Nimotop (nimodipine)." Bayer
- (2001) "Product Information. Calan (verapamil)." Searle
- Johnson KE, Balderston SM, Pieper JA, Mann DE, Reiter MJ (1991) "Electrophysiologic effects of verapamil metabolites in the isolated heart." J Cardiovasc Pharmacol, 17, p. 830-7
- "Product Information. Dynacirc (isradipine)." Sandoz Pharmaceuticals Corporation
- Kumar KL, Colley CA (1994) "Verapamil-induced hepatotoxicity." West J Med, 160, p. 485-6
- Traverse JH, Swenson LJ, Mcbride JW (1994) "Acute hepatic injury after treatment with diltiazem." Am Heart J, 127, p. 1636-9
- Scherling D, Karl W, Ahr G, Ahr HJ, Wehinger E (1988) "Pharmacokinetics of nisoldipine. III. Biotransformation of nisoldipine in rat, dog, monkey, and man." Arzneimittelforschung, 38, p. 1105-10
- (2001) "Product Information. Sular (nisoldipine)." Astra-Zeneca Pharmaceuticals
- Abernathy DR, Schwrtz JB (1999) "Calcium-antagonist drugs." N Engl J Med, 341, p. 1447-57
- (2020) "Product Information. Conjupri (levamlodipine)." CSPC Ouyi Pharmaceutical Co, Ltd
Switch to consumer interaction data
Vascor drug interactions
There are 580 drug interactions with Vascor (bepridil).
Vascor alcohol/food interactions
There are 3 alcohol/food interactions with Vascor (bepridil).
More about Vascor (bepridil)
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: calcium channel blockers
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.